HYPOGLOSSAL NERVE NEUROPATHY AND DYSARTHRIA
KEY POINTS
- Computed tomography including computed tomographic angiography is the primary tool for looking for a structural cause of a cranial neuropathy that is likely to involving the skull base or more distal course of the nerve in question.
- Magnetic resonance imaging may be used if the pathology likely localizes to the brain stem or cisternal segment of the nerve(s) in question.
- Magnetic resonance imaging and magnetic resonance angiography cannot be trusted to confidently exclude all conditions that may lead to these neuropathies.
INTRODUCTION
Clinical Presentation
The hypoglossal, vagus, glossopharyngeal, and spinal accessory nerves and cervical sympathetic plexus may be considered as a unit as well as individually. Although one of these may dominate the clinical presentation, more than one will often be involved following careful clinical testing. In this light, a proximal injury to the hypoglossal nerve may also involve the IX, X, XI complex and cause a complex neuropathy with oropharyngeal signs and symptoms and hoarseness as well as tongue weakness.
Hypoglossal neuropathy is frequently an isolated situation. When more than one nerve is affected, and possibly associated with other symptoms or neurologic deficits, localization may be much easier and a very “directed” and concise imaging evaluation is possible. A hypoglossal neuropathy will generally require a study only from the low posterior fossa to the hyoid bone.
Sometimes, lesions outside the expected course of the nerves or those involving end organs will be the source of symptoms—for example, a tongue base carcinoma causing ear pain that is referred along the glossopharyngeal nerve. It is critical to understand all of the neurologic deficits and complaints that might arise from these nerves to enable effective imaging and interpretation of the images. This clinically responsive tactical approach should become apparent later in this chapter as well as in Chapters 137 through 139 and 141.
Cranial nerve (CN) XII dysfunctions cause fasciculation of the tongue and eventually atrophy. The protruded tongue will deviate toward the side of the lesion in the case of a nuclear or infranuclear lesion and away from the side of the lesion in the case of a unilateral supranuclear lesion and dysarthria.
Common general clinical presentations that may involve the various segments of the hypoglossal nerve are outlined as follows:
Lesions within the skull
- Brain stem and extra-axial lesions in the low cerebellopontine angle and medullary cisterns may present as lower CN deficits. Intra-axial lesions will almost always be accompanied by some sensory or motor symptoms and related physical findings. This is an uncommon site for the origin of isolated hypoglossal nerve palsy.
Hypoglossal canal–jugular fossa syndromes
- Several French eponyms have been applied to clinical findings when three, four, or five (if the sympathetics are included) members of this group of nerves are involved. These include Vernet syndrome (IX–XI), Collet-Sicard syndrome (IX–XII), and Villaret syndrome (IX–XII and the sympathetic plexus).
- French eponyms are mentioned because they are occasionally presented as an indication for the imaging procedure; however, it is more useful to describe the specific nerves at risk. If three of the five are involved, the lesion will be at or near the skull base. The lesion will usually be somewhere between the medullary cistern–jugular fossa region and the posterior belly of the digastric muscle. If just two are involved, the lesion could lie in this relatively confined space in and around the skull base but a more comprehensive imaging evaluation may become necessary.
APPLIED ANATOMY
Cranial Nerve Nucleus and Cisternal Segment
The CN XII nuclei lie close to the midline in the ventral aspect of the medulla oblongata and extend to the hypoglossal trigone in the floor of the fourth ventricle (Fig. 140.1A). The paired hypoglossal nuclei receive fibers from the precentral gyrus. Root fibers from the nuclei course anteriorly and then laterally and leave the medulla at the anterolateral sulcus. In their cisternal segment, the rootlets traverse the basal cistern above the vertebral artery to enter the hypoglossal canal.
Foraminal/Skull Base Segment
The hypoglossal canal traverses the basiocciput superiorly and medially to the occipital condyles; the condylar canal transmitting draining veins should not be mistaken for the hypoglossal canal (Fig. 140.2).1
Peripheral Segment
CN XII shares its extracranial course with CNs IX, X, and XI in the nasopharyngeal segment of the carotid sheath that lies in the retrostyloid portion of the parapharyngeal space (Fig. 140.1C–G). The hypoglossal nerve courses within the carotid sheath to the hyoid bone level, where it turns relatively abruptly anterior to travel to its distal sites of muscular innervation.
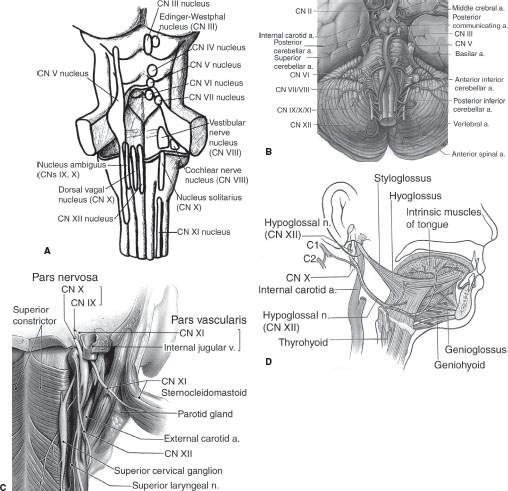
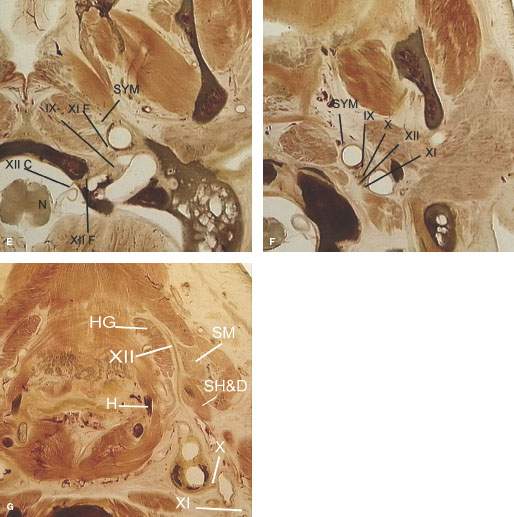
FIGURE 140.1. Anatomy of the hypoglossal nerve. A–D: Anatomic drawings of the hypoglossal nuclei in the medulla oblongata (A), the cisternal segment coursing above the vertebral arteries (B), and the skull base segment traversing the hypoglossal canal (C). The peripheral segment courses within the carotid sheath to the level of the hyoid bone, where it turns anteriorly toward the tongue to supply motor innervation (D). E–G: Anatomic sections showing the course of cranial nerve XII from its nucleus in the medulla (N) to the tongue. (XIIc, cisternal segment; XIIf, foraminal segment; H, hyoid bone; HG, hyoglossus muscle; SH&D, stylohyoid and digastric muscles; SM, submandibular gland; SYM, sympathetic plexus.)
Distal and End Organ Innervation
CN XII is the motor nerve of the tongue (Fig. 140.1D–G). It supplies all intrinsic tongue muscles, including the longitudinal, transverse, and vertical bundles, and almost all extrinsic tongue muscles, including the genioglossus, geniohyoid, hyoglossus, and styloglossus muscles.
Isolated injury causes fasciculation of the tongue or atrophy with deviation of the protruded tongue toward the side of the lesion in the case of a nuclear or infranuclear lesion and away from the side of the lesion in the case of a unilateral supranuclear lesion and dysarthria.
IMAGING APPROACH
Techniques and Relevant Aspects
General imaging parameters used in cranial and cervical sympathetic neuropathies often require a combination of high-detail images from the posterior fossa to the hyoid bone and more of a survey approach from the hyoid to the thoracic inlet and upper chest. Detailed views of a specific end organ such as the tongue may also be required. Overall, multidetector computed tomography (MDCT) is well suited to accomplishing all of these tasks very efficiently, and magnetic resonance imaging (MRI) can be focused on a specific area for problem solving when required.
For patients with hypoglossal neuropathy, a complete study should include high-detail images from the posterior fossa to the hyoid bone. The temporal bone and posterior skull base reconstructions should be completed with the same technique used to study primary temporal bone problems. Detailed views of the tongue and floor of the mouth are included in the field of view.
A detailed negative study can reassure the patient and referring physician that no treatable cause has been left uncovered.
Magnetic resonance (MR) may be used for the investigation of a hypoglossal neuropathy if the lesion is likely intracranial; however, it does not definitively exclude smaller skull base lesions.
Specific protocols for computed tomography (CT) and MR studies for investigating a hypoglossal neuropathy appear in Appendixes A and B.
Diagnostic catheter angiography may be necessary in some instances to confirm the diagnosis of a paraganglioma if it is equivocal on imaging. Until newer MDCT techniques such as the 320 MDCT units released in 2008 that are capable of assessing flow dynamics and detailed angioarchitecture become generally available, diagnostic catheter techniques will remain necessary to assess these parameters, often as a prelude to endovascular interventions that may be an adjunct to surgical removal.
Radionuclide studies are used sparingly in cases likely to be due to skull base osteomyelitis. Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) should have a minor adjunctive role in evaluating diseases that lead to these neuropathies.
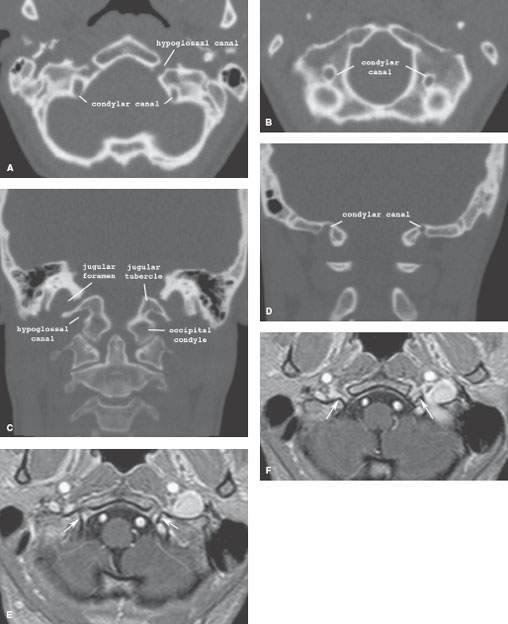
FIGURE 140.2. Normal imaging appearance of the foraminal segment of cranial nerve XII. A–D: The hypoglossal canal seen on axial (A, B) and coronal (C, D) computed tomography sections should not be confused with the condylar canal. E, F: On magnetic resonance imaging, enhancement within the hypoglossal canal with anterior extension beneath the skull base is a normal finding.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








