HYPOPHARYNX AND CERVICAL ESOPHAGUS: ACUTE AND CHRONIC EFFECTS OF BLUNT, PENETRATING, AND IATROGENIC TRAUMA
KEY POINTS
- Computed tomography is the imaging examination of choice for evaluating blunt-force and penetrating trauma.
- Computed tomography is an ideal complement to clinical and endoscopic examinations.
- Swallowing studies are still sometimes useful.
- Acute associated laryngeal injury must be diagnosed and treated within 3 to 7 days for optimal outcome.
- Hypopharyngeal, esophageal, and laryngeal injury is sometimes overlooked in multitrauma victims with more obviously life-threatening problems.
INTRODUCTION
Etiology
The hypopharynx and cervical esophagus can be injured accidentally or iatrogenically. The treatment principles for the injured hypopharynx and esophagus are intimately related to those of the larynx that have been in place for decades and well before the advent of computed tomography (CT) and magnetic resonance imaging (MRI). Treatment has varied minimally over the years; however, the triage, planning, and prognosis are executed in a more informed context because of diagnostic imaging and improved endoscopic technique input.
The imaging appearance of the hypopharynx and esophagus depends directly on the mechanism of injury. Imaging, almost entirely done nowadays with CT, shows the extent of injury to the laryngeal skeleton and related tissues, including the hypopharynx and its junction with the esophagus. In the late 1970s and into the 1980s, CT significantly advanced our understanding of how the larynx responds to blunt and other forms of trauma.1,2 Imaging with CT and occasionally other studies takes its place alongside endoscopy on the critical path for triage of hypopharyngeal and esophageal injuries to proper management plans.
Prevalence and Epidemiology
Blunt hypopharyngeal and esophageal trauma is a sporadic occurrence associated with motor vehicle accidents. Clothesline-type injuries are more associated with motorcycle, all-terrain vehicle, and bicycle accidents. Assaults and fights make up the bulk of other blunt-force trauma to the neck. Blunt and penetrating insults may occur with the same incident. Penetrating injuries are relatively uncommon. Retained foreign bodies are usually in the pharynx rather than the larynx.
Iatrogenic trauma is mainly the result of difficult endotracheal intubation, nasogastric tube placement, and unrelated surgical procedures such as the chronic effects of hardware placed at the time of spinal surgery or other hardware that rarely erodes into the esophagus and hypopharyngeal walls.
Tracheoesophageal fistulas are discussed in Chapter 214.
Clinical Presentation
Blunt-force and penetrating injuries of the hypopharynx and esophagus most often accompany injuries to the larynx and trachea; the latter may compromise critical functions. Airway maintenance is always the primary concern, and control of bleeding might be a secondary but equally emergent issue (Fig. 220.1). Once the airway is secured, therapy is focused on preserving other glottic function, including a normal voice, and assuring swallowing without aspiration. Acute injuries require a rapid examination that is accurate and free of potential added morbidity.
Clinical evaluation may suggest hypopharyngeal, esophageal, and laryngeal injury; however, this possibility may be overlooked when other extensive head and face injuries are present in the absence of life-threatening airway obstruction. Swelling of the cervical soft tissues can hide gross disruption of the normal visceral compartment anatomy from palpation. Failure to acutely establish the extent of injury can lead to swallowing disorders and laryngeal stenosis that has typically proven more difficult to manage at a later time. Delayed treatment can lead to a less satisfactory outcome and unfortunate complications such as deep neck abscess.
PATHOPHYSIOLOGY
Anatomy
A thorough knowledge of the following anatomy and anatomic variations of normal in each of the these areas is required for the evaluation of hypopharyngeal and esophageal trauma. This anatomy is presented in detail with the introductory material on the hypopharynx, larynx, cervical esophagus, and infrahyoid neck in general.
Evaluation of hypopharyngeal, esophageal, and laryngeal injury should include the following:
- Hypopharynx (Chapter 215)
- Cervical esophagus, most importantly the esophageal verge junction with the postcricoid portion of the hypopharynx (Chapter 221)
- Larynx, including the laryngeal skeleton, deep tissues spaces within the larynx, mucosal landmarks, and functional structures within larynx (Chapter 201)
- Tongue base region and low oropharyngeal wall (Chapter 190)
- Trachea (Chapter 209)
Evaluation of Injuries to Structures Outside of the Pharynx and Esophagus
- Visceral compartment of the neck and related fasciae (Chapter 149)
- Knowledge of the entire course of the vagus and recurrent laryngeal nerves on both sides (Chapter 201)
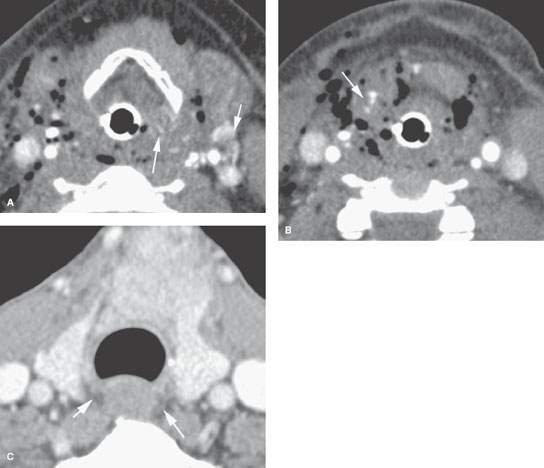
FIGURE 220.1. A, B: Patient 1 with a very severe injury to the neck due to a high-energy motor vehicle accident. The crushing force was centered at the thyrohyoid membrane, rupturing the hypopharynx and supraglottic larynx. A contrast-enhanced computed tomography study was done to evaluate the extent of neck injury. In (A) and (B), the laryngeal cartilages are shown to be grossly intact. There is generalized severe swelling throughout the neck with free air in the soft tissues. In addition, there are numerous areas of contrast puddling (arrows) in the injured pharyngeal and laryngeal soft tissues, which is consistent with vascular injury. The study also shows gas tracking from the lumen of the pharynx and larynx directly into the soft tissues due to mucosal tears. The findings were considered overall to be consistent with a very significant crush injury to the larynx, with the laryngeal cartilages remaining intact and the injury being predominately to soft tissues and connecting membranes and ligaments. (NOTE: More images on this patient are presented in Fig. 207.7, confirming a vascular injury and also spinal injuries.) C: Patient 2 had blunt trauma to the low neck causing a large hematoma due to a thyroid gland laceration. The patient had dysphagia. Only a minor amount of swelling is noted around the esophagus. Other images of this patient (Fig. 207.3) showed cricoid cartilage fractures, but there was no gross injury to the hypopharynx or cervical esophagus.
Pathology and Patterns of Disease
Blunt hypopharyngeal and esophageal trauma most commonly is due to a force applied from anterior to posterior. The most common impacts are between the neck and a dashboard; a punch of some sort to the neck; or a “clothesline” type of mechanism of injury, including strangulation. False passages that accompany blunt-force visceral compartment trauma typically affect the hypopharynx, esophagus, and the larynx.
Penetrating injuries are most frequently related to stab wounds, gunshot wounds, and intubation injuries.
Acute Injuries
In blunt-force trauma, compression of the hypopharynx and esophagus between the source of the force and cervical spine (Fig. 207.1) is the basic mechanism of injury. The amount and vector of the applied force, area impacted, and contour of the offending object all contribute to the extent of injury. As well, there are other factors that may influence the pattern of injury. For instance, if the hypopharynx and/or esophagus are actually compressed against the cervical spine, the size of arthritic spurs along the anterior aspect of the cervical spine may influence the injury pattern. The esophagus is actually less likely to be injured in such a manner below the esophageal verge since it will slide to one side, preferentially the left, and not be crushed against the cervical spine as much as the more rigidly attached larynx and hypopharynx. In any type of trauma, the level of the visceral compartment that is the central point of injury and its influence on modifying tensions exerted by the various pharyngeal muscular attachments, as well as the supra- and infrahyoid strap muscles, will clearly alter the pattern of injury.
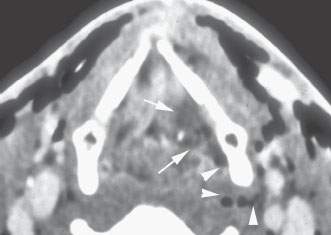
FIGURE 220.2. An image (others are shown in Fig. 207.5) from a contrast-enhanced computed tomography study in a patient experiencing neck trauma due to a motor vehicle accident. There is extensive swelling along the posterior aspect of the left false vocal fold (arrows) and some gas tracking in an enhancing soft tissue tract from the pyriform sinus (arrowheads). This suggests the presence of a false passage, which subsequently was confirmed at endoscopy.
Soft Tissue Injuries
Blunt trauma results in blood and edema that spreads through the deep planes surrounding the hypopharynx and esophagus. Just as with tumor, this will manifest as localized swelling and obliteration of fat within the peripharyngeal tissue spaces (Figs. 220.1 and 220.2).
Limited membranous lesions may cause air leakage and substantial neck emphysema without much effect on the pharyngeal tissues (Fig. 220.3). More severe lesions cause bleeding and edema, narrowing the pharynx as well as the airway (Fig. 220.1). Axial CT shows the cross-sectional area of the airway. Swelling within the portions of the hypopharynx, esophagus, or larynx may prevent a complete endoscopic examination of the region; if so, the CT examination becomes even more critical to assessing the next step in managing potential injuries to the hypopharynx, cervical esophagus, and/or larynx.
Mucosal injury extent is usually established by laryngoscopy. The exact mechanism of mucosal tears or avulsion in blunt-force trauma is unclear, but these injuries are common and likely due to shear. CT and endoscopy will normally provide all the information necessary for management (Figs. 220.2–220.6). Laryngoscopy directly evaluates the mucosal status, glottic function, and airway status. CT evaluates the laryngeal skeleton and deep planes and confirms the airway status. Water-soluble contrast swallow is held in reserve to identify an otherwise undetectable false passage. It is, however, interesting how often CT will provide clues or actually demonstrate the site of a false passage (Figs. 220.4–220.9). Gas outside of the hypopharyngeal and esophageal lumen but near an area of focal soft tissue swelling is a good clue (Figs. 220.2 and 220.3) if a tear is not plainly visible. Sometimes, a mucosal tear or pocket of fluid and air beyond the pharyngeal or esophageal wall can be seen (Figs. 220.4–220.9). Occasionally, a fistula to the neck or between the airway and pharynx or esophagus is seen on CT (Fig. 220.6).
If imaging is done several days or more out from the traumatic event but still during the subacute phase, then contrast may be used to help evaluate for associated infection and/or the types of mucosal injuries just described (Fig. 220.8). Penetrating injuries may leave tracts of gas, blood, edema, and foreign bodies along their pathway (Figs. 220.10–220.17). The offending “instrument” of the trauma may be seen (Fig. 220.13).
Retained foreign bodies that have been swallowed or expectorated can leave areas of local mucosal swelling (and enhancement if intravenous contrast is given), extraluminal gas, and actual false passages or fistula (Figs. 220.11 and 220.12).
Penetrating images tend to shatter the cartilages and the attachments of pharyngeal musculature or cause a laceration of the connecting membranes of the laryngeal skeleton that may result in further anatomic distortion and swallowing dysfunction (Fig. 220.9).
Supraglottic soft tissue avulsion seen on CT scans may herald significant epiglottic cartilage injury. Extensive mucosal irregularity cannot be distinguished from epiglottic and aryepiglottic fold (medial pyriform sinus wall) avulsion (Fig. 220.14).
The hyoid bone may be displaced by laryngeal and extrapharyngeal bleeding and edema. Hyoid fracture is distinctly uncommon, and its normal segmented appearance should not be mistaken for fractures.
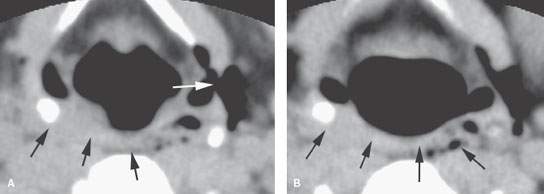
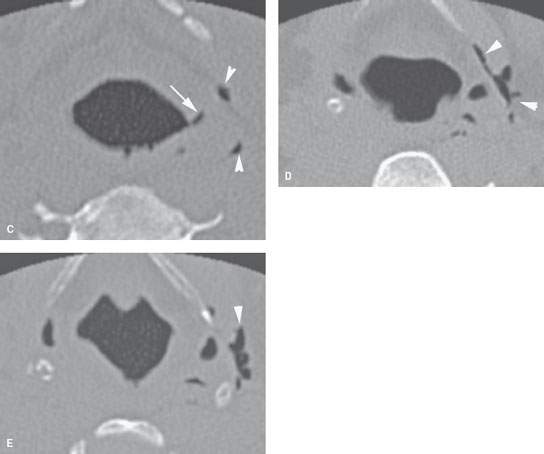
FIGURE 220.3. A patient suffering blunt laryngeal trauma. Non–contrast-enhanced computed tomography was done. A, B: There is a tear in the lateral wall of the pyriform sinus (white arrow in A) and tract of air extending into the neck. There is also soft tissue swelling of the contralateral posterior pharyngeal wall and retropharyngeal edema (black arrow). C–E: There is a small mucosal tear (white arrow in C) and multiple areas of air distributed peripherally along and outside the thyrohyoid membrane (arrowheads). The patient was endoscoped, and a false passage was identified but there was no intervention. The patient recovered with conservative care.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








