Hypopharynx and Cervical Esophagus: Infectious and Noninfectious Inflammatory Diseases
KEY POINTS
- Imaging is occasionally useful in the management of epiglottitis/supraglottitis and other acute pyogenic laryngeal infections that potentially spread to the hypopharynx.
- Computed tomography can provide a safe and rapid assessment of the airway in a patient who is stable, under the control of the treating physician for airway management decisions, and wishes to avoid endoscopy.
- Imaging in noninfectious inflammatory hypopharyngeal and esophageal diseases is generally nonspecific for diagnostic purposes.
- Atypical clinical and imaging features of hypopharyngeal and esophageal pathology should raise the possibility of an inflammatory process rather than cancer.
- Relatively few people undergo imaging for this group of diseases.
A variety of infectious and noninfectious inflammatory disorders may affect the hypopharynx and esophagus. The vast majority never come to imaging. In particular, those of the esophagus are usually only images in the context of secondary infectious involvement from an adjacent source or as a complex matter such as an infected tracheoesophageal fistula. An imaging study is often obtained because the etiology of the disease is uncertain, and it is thought that imaging might help with the diagnostic process. This might occur in diseases that may mimic cancer, and several diseases in this category are capable of that masquerade. Others come to imaging for a noninvasive assessment of the static airway dimensions when it is felt that this might be less risky and/or sufficient to decide on how to manage the airway.
The vast majority of these diseases arise in conjunction with laryngeal infectious and noninfectious inflammatory diseases or are secondary due to such disease arising in the retropharyngeal, prevertebral, and other deep neck spaces or spreading inferiorly from the oropharynx. Because of these trends, this chapter summarizes information provided in Chapters 146, 151, 155, 160, 192, and 204. The pathophysiology and imaging appearance of inflammatory and infectious diseases is presented Chapters 13 through 20.
ANATOMIC CONSIDERATIONS
A thorough knowledge of hypopharyngeal, esophageal, and related laryngeal anatomy, as well as anatomic variations, is required for the evaluation of hypopharyngeal and esophageal inflammatory diseases. This anatomy is presented in detail with the introductory material on the hypopharynx, cervical esophagus, larynx, and infrahyoid neck in general.
Evaluation of the hypopharynx and esophagus and related structures frequently involved with contiguous inflammatory disease should include the following:
- Hypopharynx, including its posterior pharyngeal wall, pyriform sinus, and postcricoid components and their attachments to the laryngeal skeleton (Chapter 215)
- Cervical esophagus, in particular its junction with the postcricoid portion of the hypopharynx (Chapter 221)
- Larynx (Chapter 201)
- Trachea (Chapter 209)
- Tongue base region and low oropharyngeal wall (Chapter 190)
Evaluation of Spread Beyond the Pharynx and Esophagus
- Visceral compartment of the neck and related fasciae and retropharyngeal space (Chapter 149)
Evaluation of Regional Lymph Node Disease
- Detailed knowledge of normal node and perinodal morphology and the common drainage pathways of pharyngeal disease (Chapters 149 and 159)
IMAGING APPROACH
Techniques and Relevant Aspects
The hypopharynx and esophagus are studied in essentially the same manner as the larynx and trachea. The principles of performing these studies are reviewed in Chapter 201. Specific problem-driven protocols for computed tomography (CT) and magnetic resonance imaging (MRI) are presented in Appendixes A and B. For the esophagus, such studies should be carried to the carina and sometimes the distal esophagus.
There is little or no use for external ultrasound in studying the hypopharynx and esophagus. Endoluminal techniques are very useful but beyond the scope of this text.
The approach with radionuclide studies depends on the aim of the examination. Most of the current usage is limited to cancer evaluation with fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET). This is discussed in more detail in conjunction with the larynx (Chapter 201).
Pros and Cons
Evaluation of Disease of Uncertain Etiology and/or Extent
Inflammatory disease limited to the hypopharynx and esophagus may mimic the initial presentation of cancer (Fig. 217.1). Any condition, regardless of etiology, that is suspicious for deep infiltration or cancer should be studied primarily with CT, if imaging is desired as part of the evaluation. MRI is rarely indicated in inflammatory conditions of the hypopharynx or esophagus since a significant proportion of magnetic resonance (MR) studies will be of poor quality owing to motion artifacts and will add no additional information that will alter medical decision making. Supplemental MR study, in the uncommon situation where it might add meaningful incremental data (Fig. 217.2A,B), is best directed by CT findings to a localized area of interest where its strengths related to better soft tissue contrast resolution may be exploited; this is often at the junction of the postcricoid region and cervical esophagus (Fig. 217.2D,E).
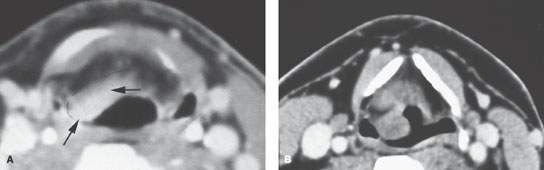
FIGURE 217.1. Contrast-enhanced computed tomography study in two patients with inflammatory disease mimicking cancer. A: Patient 1. The focal mass of the aryepiglottic fold (arrows) was thought to represent cancer clinically. It was subsequently shown to be secondary to laryngeal tuberculosis. B: Patient 2. The mass of the aryepiglottic fold and pyriform sinus thought to be cancer was eventually proven to be a manifestation of amyloidosis.
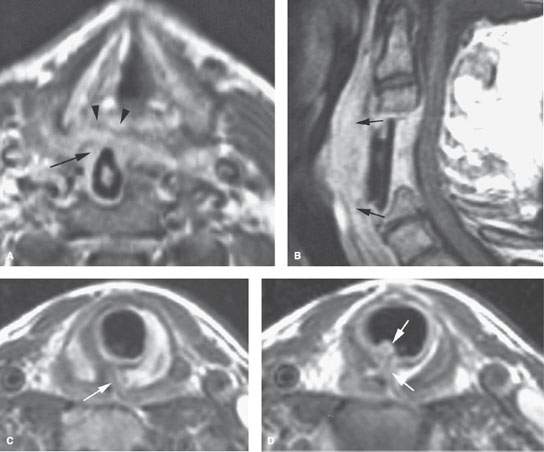
FIGURE 217.2. Two patients with magnetic resonance (MR) studies of inflammatory processes affecting the hypopharynx. A, B: Patient 1 presenting with dysphagia and an extruding strut graft surrounded by enhancing, chronically infected granulation tissue. The contrast-enhanced T1-weighted images show the granulation tissue to be homogenously enhancing and bulging (arrows) into the posterior pharyngeal wall, which was also thickened and inflamed (arrowhead in A). C, D: Patient 2 with autoimmune disease. This MR study shows abnormal mucosal thickening in the subglottic larynx related to a fistula between the larynx and postcricoid hypopharynx with secondary chondritis (arrows).
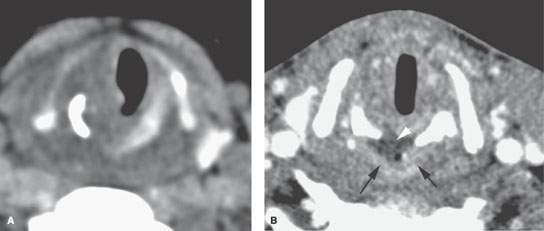
FIGURE 217.3. Two patients with chondritis affecting the postcricoid region. Both had dysphagia. A: Patient 1 had a prior history of attempted intubation with computed tomography (CT) study showing extensive edema and erosion of the upper right side of the cricoid cartilage. These changes were due to infectious chondritis following traumatic intubation. B: Patient 2 had a chronic burn injury to the upper airway resulting in dysphagia and chronic hoarseness without an obvious mucosal lesion. The contrast-enhanced CT shows enhancing tissue surrounding lower-density, likely necrotic, tissue (arrows) and irritating the upper postcricoid hypopharynx.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








