
Image Guidance for Scoliosis
Image guidance for spinal procedures has been a recent addition to neurosurgery.1–11 The most common use for stereotactic guidance in the spine is to place pedicle screws.5,9,11 The ability of image guidance to safely place pedicle instrumentation in rotated, abnormal, or small pedicles has dramatically changed scoliosis surgery.
The complex anatomic relationships and rotation seen in spinal deformities such as scoliosis can place anatomic structures in very different locations than a surgeon might expect based on experience with more routine cases. This has limited the use of pedicle screws, particularly in the thoracic and high lumbar spine where the pedicles are smallest. Unfortunately, these are the most common areas for spinal deformity and the sites of the greatest rotation of the spine.
Although hooks and rods allow segmental control, they provide less corrective power and less stabilization control. This can lead to a partial postoperative loss of the initial surgical correction. Over the years, standard hook patterns and plans for deformity correction were based on such instrumentation.
Pedicle screws constructs provide much more powerful correction and better holding power. The preservation of the ligamentum flavum and interspinal ligament possible with pedicle screws decreases the risk of junctional deformity. The power of correction that screws provide can limit the number of segments involved in the reconstruction. The only segments anatomically required for correction are the rigid portion of the curve.
The rotation seen in spinal deformity, such as scoliosis, not only limits anatomic orientation to screw placement, it makes fluoroscopy virtually useless. The parallax introduced into the fluoroscopic image can lead the surgeon to believe that there is proper orientation when in reality, the screw trajectory is grossly in error. Image guidance allows the surgeon to accurately assess pedicle size and determine screw diameter and length before surgery. This, combined with the inherent accuracy of placement that image guidance offers, allows constructs to be planned using pedicle screws for the majority or all desired fixation points. This has led to a fundamental change in the rules of correction. Constructs can be limited to the rigid portion of the curve. Greater correction is possible, and more segments of control are available.
The planning programs for the image-guidance system also clarify the anatomic relationships of spinal deformity, and the presence of hemivertebrae or severely distorted spinal anatomy can be better understood prior to surgery (Fig. 22–1). Improved understanding of anatomy prior to surgery leads to a safer procedure, even if the system is not used for intraoperative guidance.
Improved preoperative planning also leads to accurate implant size selection, which saves time. Knowing what type, size, and position the implants will be in allows the surgeon to know exactly what construct will be in place after surgery. In spinal deformity, such knowledge leads to more realistic plans by allowing the surgeon to assess what forces can be applied in correction.
This chapter explores in detail the preoperative planning and surgical techniques for image guidance in spinal deformity.
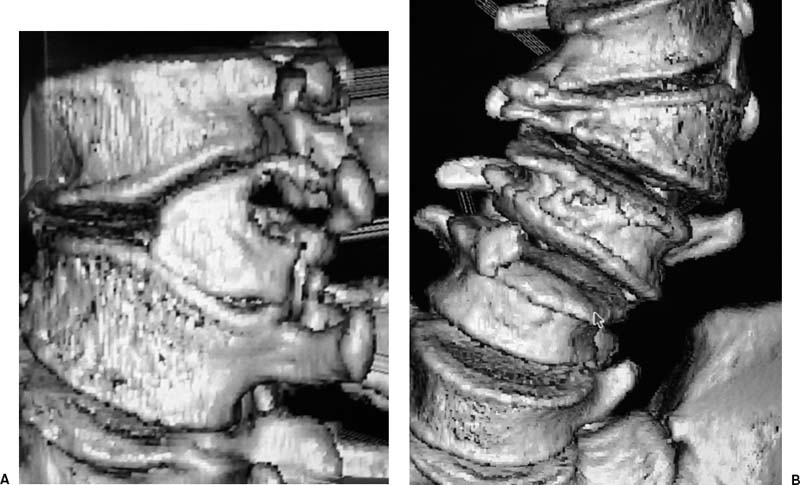
FIGURE 22–1. Anteroposterior and lateral 3-D reconstructed views of the lumbar spine in a patient with a congenital hemivertebrae showing the hemivertebrae and the adjacent segment abnormalities associated with it.
 Preoperative Planning
Preoperative Planning
Once the patient has been scanned, the data are transferred to the workstation, and the software is used to reconstruct the images. The system software then displays the images in two- or three-dimensional (2-D or 3-D) multiplanar views. The 3-D view can be rotated. The planes of the simultaneous 2-D views can be selected, and areas of interest can be highlighted to improve understanding of a particular anatomy or pathology. This is particularly important in spinal deformity cases. In these situations, anatomic relationships can be distorted, confusing the surgeon and making accurate preoperative planning difficult. Combining a rotatable 3-D image with 2-D reference in multiple planes allows a surgeon to understand even the most complex anatomic distortion. The image sizes can also be manipulated. Some systems provide drop-down menus with tools that enable precise measurement of structures.
Lending even more power to these systems is the capability to superimpose precisely scaled cursors with the same relative dimensions as planned implants. Prior to surgery, we will place virtual screws in each pedicle that we would like to control. This generates a realistic assessment of where screws can go or hooks must be utilized, and accurate preoperative plans that are critical in deformity corrections can be made. The surgeon will know precisely the length and diameter of each implant. The entry point, angle of entry, or dimensions of the screw can be manipulated to obtain an appropriate fit.
This preoperative plan can be stored and used intra-operatively to select the appropriate screw, to find the entry point, and to follow the selected trajectory. Some systems integrate this information into a targeting view so that the multiple images do not need to be simultaneously viewed and processed during the actual placement of the instrumentation. This precise localization and placement allows safe placement of implants. Implants placed in ideal positions offer more powerful control and corrective force. Eliminating maneuvers such as laminotomies to palpate pedicles saves bone surface for grafting and prevents blood loss. With experience, time savings are also realized.
 Operating Room Setup and Patient Positioning
Operating Room Setup and Patient Positioning
The patient is positioned on the operating room table as for a conventional spinal procedure. The workstation monitor is placed so that the surgeon has a clear view (Fig. 22–2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



