Pathology
Procedure
Tenosynovitis
Ultrasound-guided aspiration/injection
Tendinopathy
Ultrasound-guided tenotomy, blood injection, steroid injection, PRP injection
Tendon tears (partial)
Ultrasound-guided tenotomy, blood injection, PRP injection
Ganglion
Ultrasound-guided aspiration, wall disruption, and steroid injection
Joint
Ultrasound-guided aspiration +/− injection, synovial biopsy (CT or fluoroscopy for deeper joints)
Bursa
Ultrasound-guided aspiration +/− injection
Calcific tendinosis
Ultrasound-guided barbotage
Soft tissue lesion
Biopsy (usually in consultation with soft tissue tumor surgeon), ultrasound-guided for superficial lesions (CT guidance for deeper lesions)
Miscellaneous
Muscle biopsy for diagnosis myositis, Morton’s neuroma injection, trigger finger, perineural diagnostic and therapeutic injections, e.g., carpal tunnel syndrome
Imaging Modalities
Ultrasound is an ideal imaging technique for image-guided therapy (Figs. 4.1 and 4.2). Ultrasound is readily available and inexpensive and involves no ionizing radiation. It provides direct communication with the patient throughout the procedure. Assessment of the soft tissue mass, localization of solid components suitable for biopsy, and assessing lesional and adjacent soft tissue vascularity with Doppler are all possible with ultrasound. The dynamic real-time imaging allows for continuous imaging of needle tract and localization of injectate throughout the procedure. In addition, alternate sources of pathology can be identified and assessed, e.g., identification of a periarticular bursa in a patient with suspected septic arthritis. If a joint effusion is present, aspiration of the joint and bursa may be required but as separate procedures.
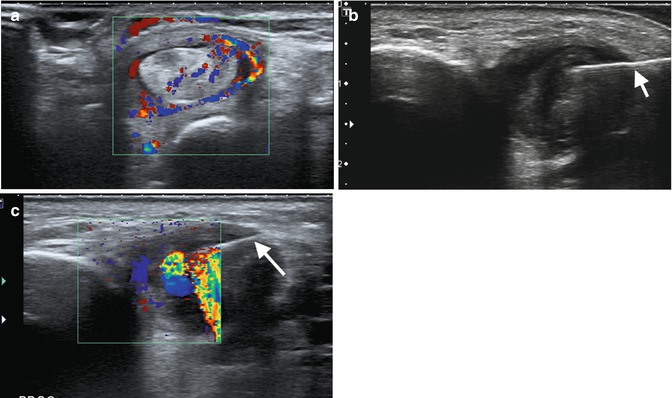
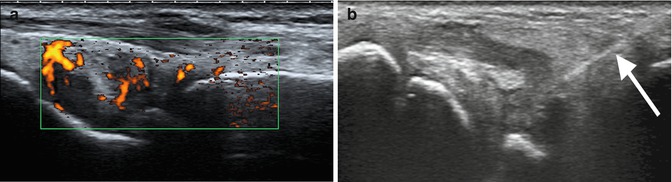
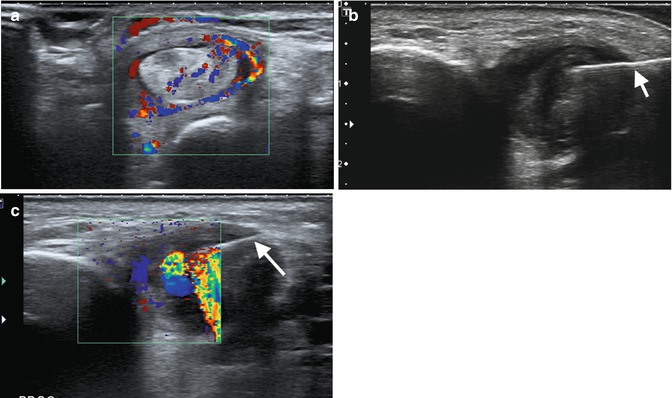
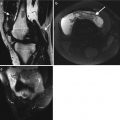
Fig. 4.1
A 59-year-old female patient with marked posterior tibialis (PT), tendinosis, and tenosynovitis. (a) Transverse ultrasound level of the medial malleolus demonstrating thickened heterogenous tendon and distended tendon sheath with increased flow within on color Doppler. (b) Needle (arrow) within PT tendon sheath. (c) Color Doppler demonstrating motion injectate during injection
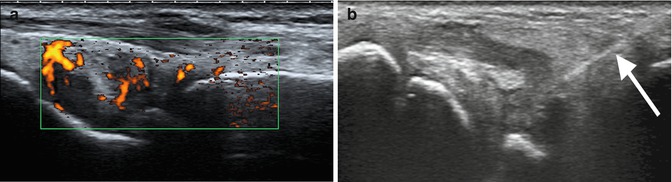
Fig. 4.2
A 29-year-old female with subacute right wrist synovitis of unknown etiology for ultrasound-guided synovial biopsy. (a) Active synovitis of the dorsal radiocarpal joint with moderate flow on power Doppler and (b) synovial biopsy needle (arrow)
CT is usually reserved for musculoskeletal procedures not suitable for ultrasound guidance (Fig. 4.3). Deep soft tissue masses, where ultrasound may have difficulty visualizing the mass, are suitable for CT guidance. All masses where there is any possibility of malignancy require review by an oncology surgeon prior to procedure, so the correct access path is employed as this will be resected at the time of surgery. Bone biopsies can be performed under fluoroscopy or CT, the latter allowing for greater precision.
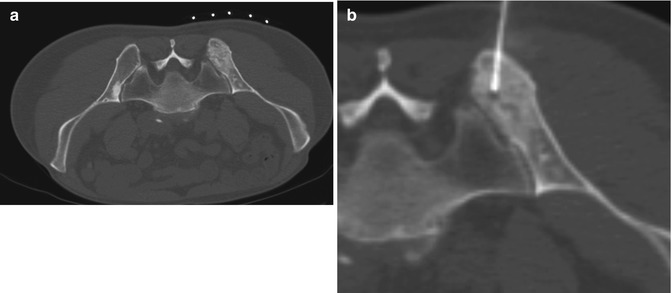
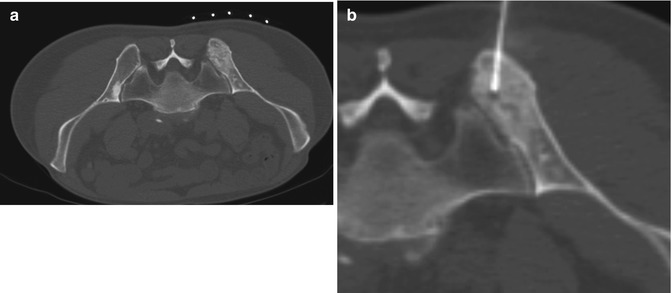
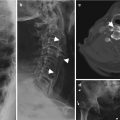
Fig. 4.3
A 68-year-old male with right pelvic pain. (a) Axial CT with patient prone demonstrates ill-defined sclerotic lesion of the right posterior ilium and (b) CT-guided bone biopsy with in situ needle. Lesion confirmed to be metastatic deposit from prostate carcinoma
Fluoroscopy is most commonly employed for joint injections and aspirations. Fluoroscopy is also used for image-guided biopsy of bone lesions, vertebroplasty, and kyphoplasty. MRI is currently not used for MSK-guided procedures due to cost, time restraints, the requirement of non-ferromagnetic instruments, and the ready availability of ultrasound and CT.
Procedures
Tenotomy or dry needling is performed in selected cases for tendinopathy or partial tears. The involved tendons should not be involved by a systemic process as can be seen in seronegative arthropathies, which usually require treatment of the underlying systemic disease. A 22G needle repeatedly transverses the local pathology under ultrasound guidance, disrupting areas of fibrosis and chronic inflammation and inducing an acute injury. Localized intratendinous hemorrhage occurs with an influx of platelets, containing multiple growth factors, which in turn stimulate healing. Activity related to the treated tendon is limited for 2 weeks, and then a graduated return to normal activity is employed. Education with respect to the initiating pathology is required to prevent recurrent tendinopathy. Physiotherapy is often used in conjunction with tenotomy after a period of 2–4 weeks. An extension of tenotomy is whole blood injection and plasma-rich platelet (PRP) injections (Figs. 4.4 and 4.5). Tenotomy is performed as described above. After tenotomy, 3–5 ml of the patient’s whole blood or PRP is directly injected into the tendon at the tenotomy site. PRP requires centrifuging 10–20 ml of the patient’s whole blood. This allows separation of plasma and RBCs. Platelets are concentrated in the plasma, ideally at least five times the blood concentration, and hence contain a greater proportion of growth factors, which should have a greater impact on healing. Further research is required directly comparing tenotomy, blood injection, and PRP injection. The most common tendons treated in our center include the common extensor tendon at the elbow, the Achilles tendon, the common flexor tendon, and the patellar tendon.
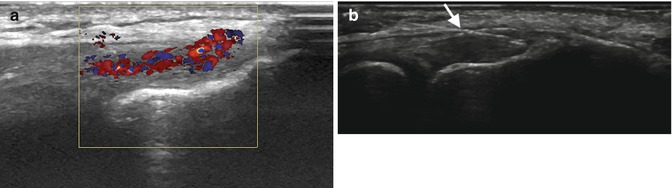
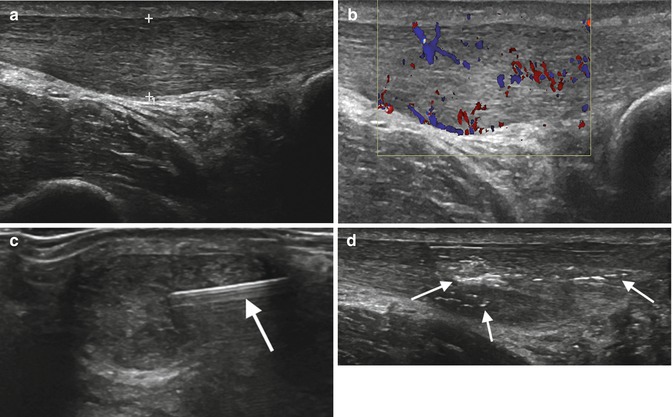
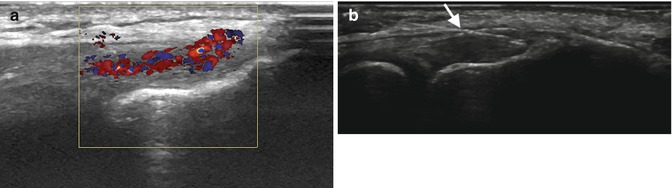
Fig. 4.4
A 44-year-old male with chronic extensor tendinosis at the elbow unresponsive to conservative treatment. (a) Pre-procedural ultrasound demonstrates tendon heterogeneity and significant internal flow on power Doppler; patient had also severe tenderness with mild probe compression over this region. (b) Needle (arrow) transversing the tendon as part of tenotomy immediately pre-PRP injection
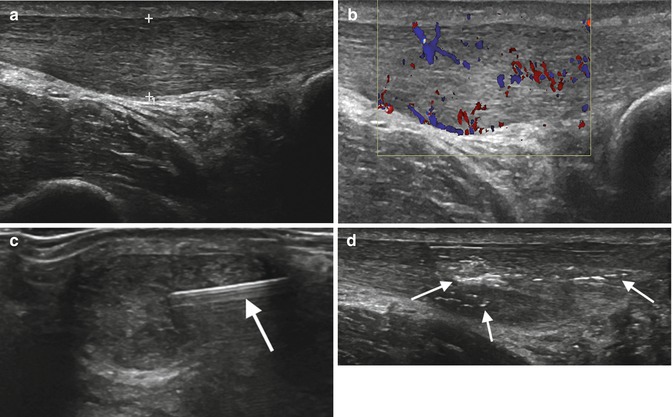
Fig. 4.5
A 52-year-old male with Achilles tendinosis with limitation activity and pain on compression of the mid-Achilles. (a) Longitudinal ultrasound demonstrates mid AT tendinosis with (b) increased internal flow on color Doppler. (c) Tenotomy needle (arrow) on transverse image and (d) longitudinal ultrasound image post PRP injection demonstrating the expected proximal and distal propagation of the injectate (arrows)
Barbotage, calcific tendinosis disruption and aspiration, is used in selected cases for treatment of symptomatic calcific tendinosis. Identification of calcific tendinosis on imaging should be correlated with the patient’s symptoms. It is most commonly identified within the rotator cuff. Symptoms directly over the area of calcification and lack of adjacent pathology should be assessed prior to barbotage. If there is a generalized tendinopathy without exaggeration of symptoms over the area of calcific tendinosis, we will often advise a conservative treatment for tendinopathy in the first instance. In those cases selected for barbotage, the calcification is identified under ultrasound, and a 20–22G needle is repeatedly passed through the calcification while flushing and aspirating with local anesthetic (Fig. 4.6). Some centers use a two-needle approach, one for injection of local anesthetic and the second to aspirate. Steroid should be injected into any overlying bursa, e.g., subacromial-subdeltoid bursa when performed for the supraspinatus tendon, to limit secondary bursitis due to potential leakage of crystals into the bursa. Radiographs are taken pre- and post-procedure and at 3 months. There is often residual calcification immediately post barbotage that is gradually reabsorbed on follow-up.
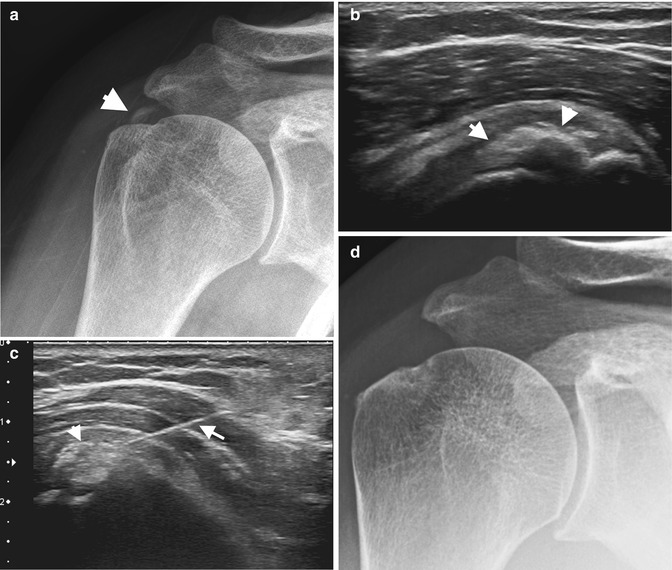
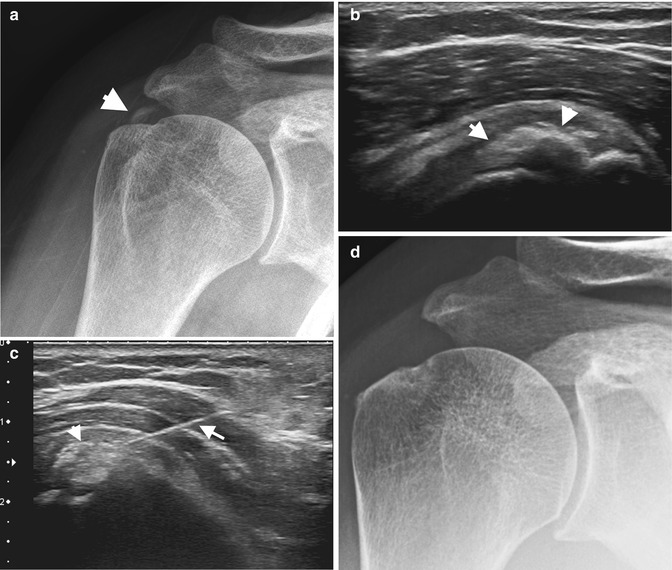
Fig. 4.6
A 28-year-old female with calcific tendinopathy of the supraspinatus tendon with persistent pain and limited range of motion for 1 year. (a) AP radiograph demonstrates calcification of the supraspinatus tendon (arrowhead). (b) Longitudinal ultrasound with hyperechoic calcific deposit corresponding to radiograph (arrowheads), patient had tenderness on probe compression directly over the calcification. (c) Needle (arrow) transversing the calcification (arrowhead) which is already partially disrupted after previous passes by the needle. (d) Follow-up radiograph 3 months post-procedure with no residual calcification. Patient reported complete relief of symptoms
Arthrography
Arthrography, injection of a contrast into a joint space, may be performed for diagnostic or therapeutic purposes (Table 4.2). A conventional arthrogram is usually performed as a fluoroscopically guided injection of a joint but may be performed under ultrasound or CT guidance in selected cases. Intra-articular position is confirmed by injection of a small amount of iodinated contrast into the joint space. Depending on the procedure, the joint is further distended with contrast for MRI or CT arthrogram, gadoliniums versus iodinated-based contrast respectively, or alternate injectate for therapeutic or diagnostic injection. The latter may include an anesthetic agent, viscosupplementation, or steroids. Anesthetic may be short or long acting and may help identify the origin of pain. This is commonly used for diagnostic hip injections where the symptoms may be related to intra-articular pathology of the hip, which will be relieved with anesthetic, whereas referred pain from degenerative lumbar spine disc disease or periarticular pathology will not be relieved. Use of a visual analogue score sheet for the patient pre- and post-procedure can be useful in grading any relief from anesthetic. We also advise patients to maintain a pain diary to document any long-term relief from therapeutic injections.
Table 4.2




Indications for joint-related procedures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree