Imaging evaluation of postoperative spinal infection is challenging. A systematic approach and keen understanding of multimodality imaging techniques, as well as knowledge of the patient’s surgical procedure and clinical presentation, are critical for the radiologist to render an accurate diagnosis. Because of the overlap between diagnostic imaging findings in the postoperative spine and the infected spine, in those situations in which the index of clinical suspicion for spine infection is high, then immediate consideration ought to be given to performing a spine biopsy.
Key points
- •
Evaluation of postoperative spine infection is a challenging task that requires a systematic approach for the accurate interpretation of spine imaging studies.
- •
Distinguishing between postsurgical inflammatory changes and spondylodiskitis, as well as infected postoperative fluid collections, is crucial for successful interpretation and successful patient management.
Introduction
Evaluation of potential complications in the postoperative spine is a challenging assignment and is the responsibility of many radiologists on a daily basis. The growth in surgical spine intervention has driven the advancement and use of multimodality imaging of the preoperative and postoperative spine. The radiologist interpreting postoperative spine examinations is presented with difficult conditions related to metallic instrumentation and implants, which result in artifacts obscuring anatomic detail, as well as the difficulties in distinguishing postsurgical inflammation from infection. Despite preprocedure antibiotic prophylaxis and improved surgical techniques and postoperative care, as well as advances in multimodality diagnostic imaging, postoperative infectious complications result in significant morbidity and occasional mortality. The diagnosis and management of postoperative spine infections are dependent on the assessment of multimodality imaging.
Postoperative spine infections are classified as either superficial or deep. Infectious processes contained within the skin and subcutaneous tissues without fascial involvement such as cellulitis or subcutaneous abscess are considered superficial. Deep infections occur deep to the lumbodorsal fascia for posterior lumbar wounds and deep to the ligamentum nuchae for posterior cervical wounds. Spondylodiskitis, epidural abscess, and paravertebral collections with superimposed infections are considered deep infections.
Introduction
Evaluation of potential complications in the postoperative spine is a challenging assignment and is the responsibility of many radiologists on a daily basis. The growth in surgical spine intervention has driven the advancement and use of multimodality imaging of the preoperative and postoperative spine. The radiologist interpreting postoperative spine examinations is presented with difficult conditions related to metallic instrumentation and implants, which result in artifacts obscuring anatomic detail, as well as the difficulties in distinguishing postsurgical inflammation from infection. Despite preprocedure antibiotic prophylaxis and improved surgical techniques and postoperative care, as well as advances in multimodality diagnostic imaging, postoperative infectious complications result in significant morbidity and occasional mortality. The diagnosis and management of postoperative spine infections are dependent on the assessment of multimodality imaging.
Postoperative spine infections are classified as either superficial or deep. Infectious processes contained within the skin and subcutaneous tissues without fascial involvement such as cellulitis or subcutaneous abscess are considered superficial. Deep infections occur deep to the lumbodorsal fascia for posterior lumbar wounds and deep to the ligamentum nuchae for posterior cervical wounds. Spondylodiskitis, epidural abscess, and paravertebral collections with superimposed infections are considered deep infections.
Radiography
Baseline postoperative radiographs show initial implant positioning and may be used for future comparison in patients suspected of developing complications. Although plain radiography is insensitive in the detection of early postoperative infection, it still remains the initial imaging modality for postoperative evaluation, because fusion status, spinal stability, or hardware failure can all be shown on serial radiographs. The limited usefulness of plain radiography is because of a lack of sensitivity to the early findings of infection within both the soft tissues of the spine and the spine proper. Fluoroscopy does serve as a useful modality in performing image-guided percutaneous biopsy of the spinal axis, particularly in the lumbar spine.
Computed tomography
Most spine procedures use metallic instrumentation, with the goal of providing stability and reducing pain. Multidetector computed tomography (MDCT) is an excellent modality for assessing orthopedic spinal hardware complications. In the early postoperative period, MDCT can effectively evaluate spinal alignment and implant positioning in relation to adjacent cortical bone, thecal sac, and neural foramina. In the late postoperative period, MDCT can evaluate the progression of osseous fusion and bone graft incorporation. However, computed tomography (CT), like radiography, cannot readily distinguish the early findings of infection from the typical soft tissue, disk, and osseous changes that are encountered after spine surgery. With time, as is also seen in radiography, increased soft tissue swelling or induration, abnormal fluid collections, and osseous destruction may be seen on CT. Yet, the diagnosis of spine infection is usually established at this point in the patient’s clinical course. CT does serve as a useful modality to guide spine biopsy throughout the spinal axis in cases of suspected spine infection.
Ultrasonography
Sonography has a limited role in postoperative infection imaging with its primary usefulness in detection of postoperative fluid collections and abscesses. In addition, sonography could be used for imaging guidance aspirations of these superficial fluid collections when the diagnosis of infection of a collection needs to be excluded.
Magnetic resonance imaging
Magnetic resonance (MR) imaging has an increasing role in imaging postoperative patients with suspected infection, both without and with spinal hardware. Advances in MR imaging technology and pulse sequence development have facilitated imaging in postoperative patients because of its superior soft tissue resolution. Assessment of bone marrow edema, soft tissue signal changes and enhancement, and identification of abnormal fluid collections are more accurately and consistently detected with MR imaging than with other imaging modalities. MR imaging is particularly useful for detecting and monitoring osteomyelitis/diskitis and postoperative fluid collections. Typically, imaging of implants/spinal hardware produces geometric distortion, the so-called susceptibility artifact, which is caused by the differences in the magnetic properties of human tissue and those of the implanted hardware. Titanium implants, which have been increasingly used, are nonferromagnetic and produce fewer artifacts than those made of ferromagnetic materials, such as stainless steel. Nonmetallic devices, such as nonmetallic interbody spacers, produce little artifact on MR imaging. However, visualization of infectious disease that is close to hardware remains a challenge. One technique that can be used to reduce artifact from implants is to align the main magnetic field (z-axis of the scanner) parallel with the long axis of the implanted hardware. Typically, this technique is more easily used in open magnets, where there is less restriction on patient positioning within the bore. Several other techniques are available and have proved to reduce hardware artifact, including increasing the frequency encoding gradient strength, decreasing voxel size, increasing bandwidth, and decreasing field strength.
Nuclear medicine
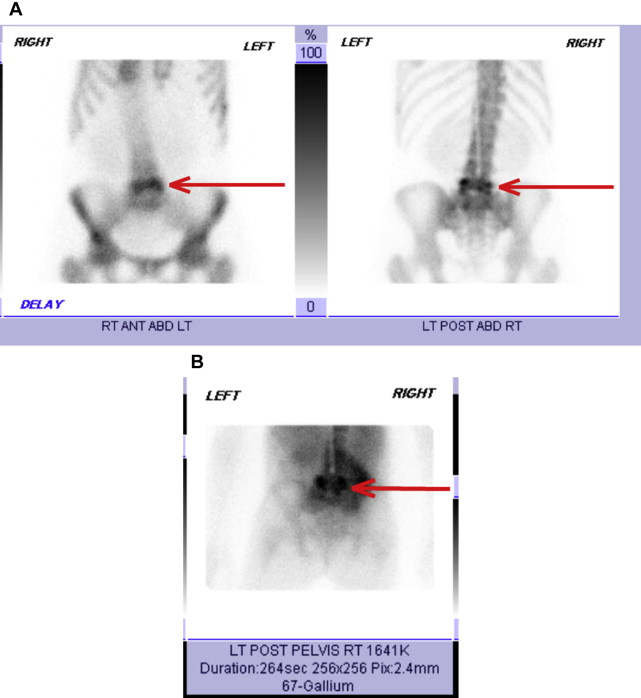
Nuclear medicine studies can also be used as part of the diagnostic workup of suspected spinal infection. These studies include 3-phase bone scans, gallium scans, and indium-111 leukocyte studies. These examinations are typically used in select situations, despite their high sensitivity and specificity, largely secondary to their poor spatial resolution and lengthy duration of the examinations. The current radionuclide imaging method of choice for diagnosing spinal osteomyelitis is combined bone-gallium imaging studies, which have been shown to be comparable with MR imaging. Uptake that is greater or discordant on gallium imaging compared with technetium (bone scan) is the most accurate finding for spondylodiskitis. Typically, this examination combination (bone-gallium scan) is used in patients in whom MR imaging is contraindicated or in whom MR imaging and CT are equivocal ( Fig. 1 ). Gallium single-photon emission CT can be comparable with combined bone-gallium imaging for diagnosing osteomyelitis. Fluorodeoxyglucose positron emission tomography also seems to be useful in diagnosing spinal osteomyelitis, with high sensitivities and specificities, although the data sample size is small.
Spondylodiskitis/epidural abscess
Spondylodiskitis is a term that encompasses a spectrum of infectious processes within the spine, including vertebral osteomyelitis and diskitis. Spinal column infections occur via several different routes, with direct hematogenous seeding of the vertebral bodies being the most common pathway. In adults, end arterioles are the vascular supply to the vertebral body subchondral endplates, with the adjacent intervertebral disks receiving nutrients via simple diffusion. Therefore, hematogenous seeding of vertebral body infection occurs at the level of the end arterioles adjacent to the subchondral endplates, with pyogenic infection subsequently spreading from the endplate into the adjacent intervertebral disk. Hematogenous spread may also occur via epidural venous extension. Direct inoculation stemming from penetrating trauma or direct exposure from open wounds, previous spinal surgery, and diagnostic and therapeutic interventional procedures, as well as contiguous spread from adjacent soft tissue infection, are other known routes of spinal column inoculation. Untreated infection can spread into adjacent soft tissues, resulting in paravertebral, psoas, and epidural abscess formation.
The diagnosis of postoperative spine infection is based on clinical, laboratory, and radiologic features. Complaints of vague or increasing neck or low back pain may be the only early indication of postprocedural diskitis. However, this complaint profile overlaps significantly with postoperative spine pain. Fever is an inconsistent sign of diskitis; however, a persistently increased C-reactive protein level for more than 2 weeks after a spine procedure is concerning and is an early indication of postoperative infection. Furthermore, postoperative spondylodiskitis is an uncommon complication of spinal surgery, with a reported incidence of 0.2% to 2.75%.
Radiographic findings may take between 2 and 4 weeks to manifest after the onset of symptoms, and thus a negative postoperative radiograph does not exclude the presence of infection. However, in cases of postoperative diskitis, disk collapse can be an early sign of infection, occurring 4 to 6 weeks after surgery. As infection spreads through and replaces the normal vertebral medullary marrow, a relative decrease in bone density may be detected. Approximately 30% to 40% of normal mineralization is usually needed to detect osteopenia within the infected vertebral body. Progression leads to subchondral endplate erosions, loss of intervertebral disk space height, osteolysis surrounding hardware, and bone destruction. Loss of subchondral endplate definition or endplate erosions can be a subtle finding but is the most reliable radiographic feature in detecting underlying early diskitis with vertebral osteomyelitis. Endplate sclerosis may be seen in the later stages of chronic infection, followed by fusion of the disk space.
Detection of endplate erosions and cortical discontinuity may be identified earlier with CT compared with plain films, as well as paraspinal inflammatory changes and psoas abscess formation with the addition of contrast-enhanced scans. The latter study is not commonly performed, but is often considered when patients are not candidates for an MR imaging examination.
MR imaging remains the preferred modality for the evaluation of potential postoperative spine infections, in particular diskitis and epidural abscess. Nevertheless, differentiating postsurgical changes versus developing infection is challenging. Subchondral endplate irregularity and erosions may be seen as loss of the normal cortical bone on T1-weighted images. Bone marrow infiltration along the vertebral endplates is classically shown by hypointense T1 and hyperintense T2 signal, as well as enhancement on postcontrast images. Progression of infection through the endplates results in diskitis. Subsequent edema and purulent material in the disk space show hypointense T1 and hyperintense T2 signal ( Fig. 2 ). There is significant overlap of imaging findings between the postoperative spine and the infected postoperative spine. For example, after diskectomy, hyperintense T2 signal is seen within the intervertebral disk space and adjacent subchondral endplates. Varying amounts of intradiskal enhancement are seen after intravenous gadolinium contrast agent administration in patients after surgery. Peripheral enhancement of the remaining disk without adjacent reactive endplate changes is suggestive of infection, whereas linear areas of enhancement are more likely postsurgical in cause. Vertebral body and intervertebral disk space enhancement may normally be seen at 6 weeks and up to 6 months after surgery in the absence of infection. An enhancing soft tissue mass in the paravertebral or epidural space is highly suggestive of septic spondylodiskitis. Given variable appearances of disk enhancement and postoperative marrow changes, spondylodiskitis may be difficult to reliably diagnose on MR imaging in the absence of epidural or paravertebral abscesses. Restricted diffusion using diffusion-weighted imaging has been shown to be present in the endplates and intervertebral disk spaces of patients with infection, but not in those with degenerative disease. Diffusion sequences are not routinely included in spine imaging protocols, but can be useful in cases in which there is a specific question regarding degeneration versus infection.










