Age >80 years
Diabetes mellitus
Rheumatoid arthritis
Prosthetic joint
Recent joint intervention, including surgery and intra-articular steroid injection
Soft tissue infection
IV drug use
Alcoholism
Table 13.2
Bacteria causing nongonococcal septic arthritis
Staphylococcus aureus |
Streptococcal species |
Gram negatives |
Mycobacterial species |
Borrelia burgdorferi |
Mycoplasma hominis |
Clinical Presentation
The presentation is typically monoarticular, with >1 joint involved in only 20 % of cases. The joint most commonly infected is the knee. Patients typically present acutely with a hot, red, swollen joint with severe pain on active and passive range of motion. Fever is usually, though not always, present. Given the associated rapid joint destruction, joint aspiration should be performed as soon as possible. Arthrocentesis typically exhibits high numbers of white blood cells: the likelihood ratio associated with septic arthritis increases with increasing number of leukocytes. For example, a WBC count of >100,000 × 10*6 cells has an associated positive likelihood ratio of 47 for septic arthritis. There are typically >80 % neutrophils. Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are usually elevated, sometimes dramatically so. Treatment is typically intravenous antibiotics initially for 2–3 weeks based on the gram stain and culture results, followed by several weeks of oral antibiotics. Joint drainage is indicated, preferably through arthroscopic or open surgical techniques.
Gonococcal arthritis often presents as an oligo- or polyarthritis in the setting of a gonococcal rash. It should be suspected in younger individuals with risk factors for sexually transmitted infections. Neisseria gonorrhoeae is not reliably isolated from gram stain or culture of the joint aspirate, and diagnosis requires culturing all potentially infected sites (urethra, cervix, pharynx, and blood), in addition to synovial fluid culture. Tuberculous arthritis is typically more indolent in presentation, with pain progressing over weeks to months, and fewer inflammatory joint symptoms with less erythema, swelling, and heat. The diagnosis is often delayed as the indolent nature of the symptoms leads to consideration of noninfectious arthropathies such as osteoarthritis or rheumatoid arthritis. Phemister’s triad seen in TB arthritis includes periarticular osteopenia, marginal erosions, and progressive joint space loss. Acute viral arthritis, usually occurring in children, is self-limiting and benign. It may be mono- or polyarticular and may present like septic arthritis as described above or like an inflammatory arthropathy. Complications of septic arthritis include joint destruction, joint deformity, osteonecrosis of intra-articular bodies, premature osteoarthritis, and ankylosis.
Differential diagnosis of a septic arthritis includes crystalline arthropathies, seronegative spondyloarthropathies, and less commonly monoarthritic presentations of rheumatoid arthritis or other varieties of inflammatory arthritis. It is typically the crystalline arthropathies that mimic the septic joint most closely, with rapid onset of symptoms, erythema and swelling of the joint, and significant pain and disability. It must not be forgotten that infection and a crystalline arthropathy can coexist in the same joint. For these reasons, no modality aside from aspiration and analysis of synovial fluid can reliably and safely distinguish these entities.
Imaging Features
Radiographs (Fig. 13.1)


Fig. 13.1
A 28-year-old male with soft tissue laceration of the radial aspect of the index finger overlying the DIPJ, (a) initial AP and (b) lateral radiograph demonstrating soft tissue swelling with no acute bone injury or retained metallic foreign body, metallic pin denotes site of injury and mild flexion deformity at DIPJ, (c) follow-up radiographic series 2 weeks later after minor trauma with fracture of the proximal diaphysis of the distal phalanx; however, there is now progressive joint space loss at the DIPJ and periarticular osteopenia with osteolysis at the ulnar margin of the distal phalanx in keeping with septic arthritis and osteomyelitis, (d) progression osteolysis and subluxation at the DIPJ
Radiographs in septic arthritis are often normal at presentation. Joint effusion, possibly leading to initial joint space widening, and/or soft tissue swelling may be detectable. Later findings include subchondral bony erosion/destruction that is present on both sides of the joint, uniform joint space narrowing secondary to cartilage damage, reactive bony sclerosis, and juxta-articular osteopenia. The regional osteopenia that develops in septic arthritis occurs as a result of the regional exuberant immune response with high levels of inflammatory cytokines and prostaglandins that act to inhibit regional bone formation and promote absorption. Coincident osteomyelitis is often present, leading to cortical destruction and reactive new bone formation of the periosteum termed “periosteal reaction” (see section entitled “Osteomyelitis”). There can be severe bony disorganization and destruction at this stage with secondary osteoarthritic change. Bony ankylosis can occur. Abscesses can form adjacent to the site of infection (see section “Abscess” below).
Ultrasound (Fig. 13.2)
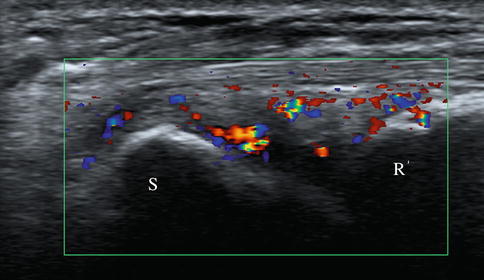
Fig. 13.2
Ultrasound in a 37-year-old female patient with septic arthritis of the wrist, longitudinal image demonstrating the radius (R) and scaphoid (s) with radiocarpal joint space distension with heterogeneous tissue demonstrating marked flow within on color Doppler. Note that ultrasound can only demonstrate an active inflammatory process and clinical correlation, and joint aspiration is required for diagnosis
Ultrasound can demonstrate a joint effusion, which may not always be present, before it becomes visible on a radiograph. Septic joint effusion is usually complex in appearance with hyperechoic appearance secondary to pus, internal septations, and debris. Occasionally effusions are anechoic. The joint capsule is diffusely thickened. Hyperemia with increased flow on Doppler may be seen within the synovium and capsule. Depending on the joint and accessibility to detailed ultrasound evaluation, other changes may be visible including cartilage destruction demonstrated as loss of the normal convex hypoechoic cartilage contour which may be filled with hyperechoic synovium and complex fluid. Erosions, as focal cortical defects, and periosteal reaction with subperiosteal collection may also be visible. The adjacent soft tissues are also evaluated for associated collections. Assessment of osteomyelitis is limited and is best performed with MRI. Ultrasound can also confirm joint effusion and guide needle placement for joint aspiration.
MRI (Fig. 13.3)
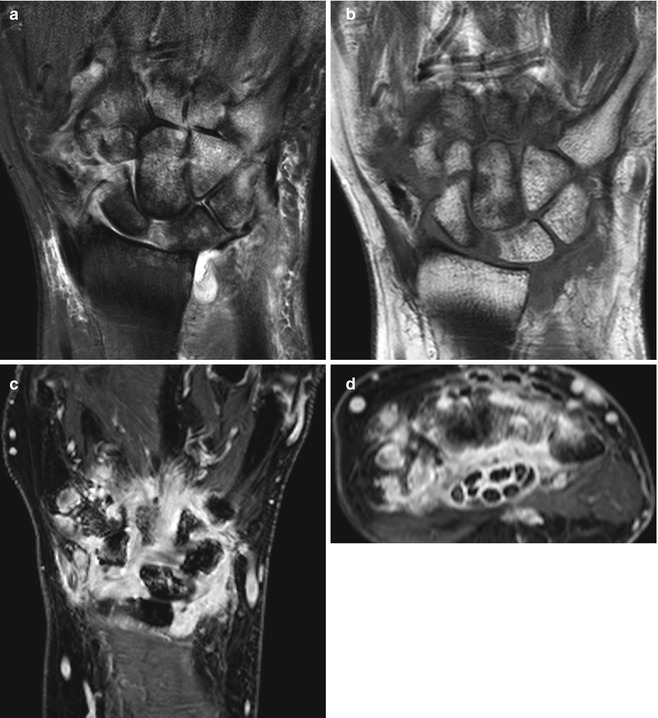
Fig. 13.3
MRI in a patient presenting with acute inflamed right wrist without prior history of inflammatory arthropathy, with septic arthritis of the radiocarpal joint with extension to the midcarpal and distal radioulnar joint with secondary multifocal osteomyelitis. (a) Cor T2FS and (b) Cor T1 demonstrating joint effusions and extensive osteitis. (c, d) Cor and reformatted axial T1FS, respectively, with diffuse enhancing synovitis, erosions, and osteitis with marked enhancement of flexor tendon sheaths (infective tenosynovitis) within the carpal tunnel. Imaging finding suggests the diagnosis, but aspiration is required for confirmation
While the diagnosis of septic arthritis should always be made based on appropriate synovial fluid sampling and culturing techniques, MRI can be a helpful adjunct to diagnosis. Multiple suggestive findings occurring in concert should raise suspicion. The adjacent bone can demonstrate erosions. Erosion is defined as a loss of the normal cortical contour of the bone, seen in two adjacent slices on MRI. The erosion shows loss of the normal cortical hypointensity and the normal trabecular hyperintensity on T1W images. Erosions are caused due to proliferative synovitis leading to pannus formation that invades into the adjacent bone, and thus post-gadolinium images show contrast enhancement within the pannus within the erosion. This pannus can also be seen as abnormal hyperintense signal within the erosion on T2W images due to the high water content in the inflamed tissue. Erosions typically occur first in the “bare area” – the marginal area of the joint near the area of attachment of the capsule that is minimally covered by cartilage and thus relatively unprotected. With continuing inflammation, however, erosions can involve any area of the articular surfaces, and severe bony destruction can occur. Adjacent bone marrow edema is also characteristic, which manifests as hypointensity on T1 and hyperintensity on T2. Synovial thickening and edema can be present, as well as a joint effusion. IV gadolinium can be used as a contrast agent and can differentiate synovium from joint effusion – in early post-gadolinium administration, synovium enhances, while joint effusion will not enhance. Soft tissue edema is present and occasionally soft tissue collections develop.
There are some unique features of tuberculous septic arthritis that can be seen on MRI. Forty percent develop synovial granulomas, which manifest as hypointense lesions on T2-weighted images. Areas of synovial proliferation (termed “pannus”) can be seen, and characteristically in tuberculous arthritis, there are both active (enhancing) and chronic (non-enhancing) pannus, which coexist. Intra-articular bodies, termed “rice bodies,” are related to ischemia of the synovium with subsequent shedding synovium and encasement by fibrin. They are classically seen in tuberculous arthritis but may also be present in entities such as rheumatoid arthritis and SLE. There can also be findings of microabscesses and evidence of osteomyelitis. Synovitis, effusions, and erosive changes are also seen as in other types of septic arthritis. Both central and peripheral erosions are seen.
Bone Scan
Bone scan is not commonly used to aid in the diagnosis of septic arthritis as the findings are indistinguishable from other types of arthritis. Classically, there is joint hyperperfusion and hyperemia on early imaging, with increased activity at articular surfaces on delayed imaging. Occasionally a WBC scan is performed in cases where there is a differential diagnosis such as Charcot joint.
CT
CT scanning is not commonly used in the setting of acute septic arthritis. Like plain radiographs, it can be normal in early stages or show only evidence of joint effusion or soft tissue swelling. It may be more sensitive to early findings of joint space widening due to effusion and later changes of erosions or periosteal reaction than radiographs, however. It could be considered when MRI is contraindicated but is generally considered inferior to MRI in septic arthritis.
Osteomyelitis
Overview
Like septic arthritis, osteomyelitis can arise due to hematologic spread of infection, direct inoculation from trauma or surgery, or contiguous spread from adjacent structures, such as an infected joint. The vertebral body is the most commonly affected area in adults and the long bones in children. Risk factors for osteomyelitis include diabetes mellitus, particularly with vascular insufficiency, peripheral neuropathy, the presence of decubitus or other chronic ulcers, prosthetic joint material, and a history of trauma. The organisms typically involved depend on the site and mode of transmission. Osteomyelitis secondary to hematogenous seeding is most commonly due to a single bacterium. Staphylococcal species, particularly Staphylococcus aureus, and aerobic gram-negative bacteria are the most common causes, with streptococci and enterococci occurring less frequently. Osteomyelitis secondary to direct inoculation, such as in patients with chronic nonhealing ulcers, is more likely to be polymicrobial.
Osteomyelitis can present either acutely or chronically, and presentation can vary by chronicity and site. Hematogenous osteomyelitis affects the medullary area of bone initially, and the subsequent inflammatory reaction causes increased intramedullary pressure that can rupture through the bony cortex. This can compromise blood flow to the periosteal region, which can lead to necrotic areas that then become separated from the rest of the bone. These sequestrated necrotic areas are characteristic of chronic osteomyelitis and are referred to as “sequestra.” These can be helpful in the identification of osteomyelitis radiologically. Typically a layer of granulation tissue separates the sequestrum from the living bone, and the sequestrum can then become encased in reactive bone (termed “involucrum”). Sinus tracts through the cortical bone to the medulla can also be seen. Abscesses can form, in the subacute to chronic phase of osteomyelitis, particularly within the ends of tubular bones, and may be single or multiple, “Brodie’s abscess.” Due to developmental changes in blood supply and end vessels, the epiphysis is a common location of osteomyelitis in the infant and the metaphysis in the child. Spondylodiscitis is reviewed in detail in Chap. 15
Clinical Presentation
Patients with acute osteomyelitis typically present with pain, warmth, and erythema of the affected site. Some sites, such as vertebral, hip, and sacroiliac, usually present with pain. Constitutional symptoms and signs such as fever and malaise may be present. In patients with ulcers, lack of improvement with appropriate wound care should raise the suspicion for underlying osteomyelitis. If an ulcer is larger than 2 × 2 cm in diameter or if bone is exposed, there is a high likelihood of underlying osteomyelitis. In these cases, treatment with antibiotics is often initiated empirically. A draining sinus tract and overlying tissue necrosis are also strong indicators.
Inflammatory markers such as erythrocyte sedimentation rate and C-reactive protein are usually elevated in osteomyelitis but are nonspecific. Blood cultures are only positive in approximately 50 % of patients with acute hematogenous osteomyelitis but should still be performed in all patients. The gold standard for diagnosis of osteomyelitis is bone biopsy, and a positive result for osteomyelitis on bone biopsy has both histopathologic and microbial components. The biopsy should show inflammatory infiltrate within the bone leading to bony resorption and subsequent necrosis on histopathology, and an offending organism should be isolated on microbial cultures. However, bone biopsy may not be feasible in the setting of inaccessible anatomic areas or if there is concern regarding lack of healing in patients with compromised vascularity, and in this case empiric treatment is typically undertaken. Superficial wound cultures are only consistent with bone biopsy results in about 30 % of cases and thus should not be used for diagnosis routinely.
Treatment of osteomyelitis is dependent on several factors, including culture and sensitivity results, chronicity, and amount of devitalized bone and necrotic tissue present, and involves a combination of antibiotic therapy and surgical debridement. Initial antibiotic therapy is typically administered intravenously. Chronic osteomyelitis and/or osteomyelitis associated with cutaneous ulcers in patients with compromised regional vascularity can require more prolonged courses of antibiotics. There is little randomized controlled data in this area to guide therapy. Uncomplicated hematogenous osteomyelitis in children can be treated for as few as 4 days with IV therapy, with transition to oral antibiotics for a period of 4 weeks. Chronic osteomyelitis in adults is typically treated with 2–6 weeks of IV antibiotics initially, then oral antibiotics subsequently to complete a course of 4–8 weeks. More prolonged courses can be required in more complicated infections. Recurrence rates in adults are quoted as being around 30 % at 1 year and even higher (~50 %) for infections with Pseudomonas aeruginosa. Bony debridement is indicated when there is necrotic tissue, and prosthetic material at the site of infection may need to be removed. Adjunctive modalities for treatment of osteomyelitis include hyperbaric oxygen therapy and negative pressure wound therapy with vacuum-assisted devices.
Imaging
Radiographs (Fig. 13.4)

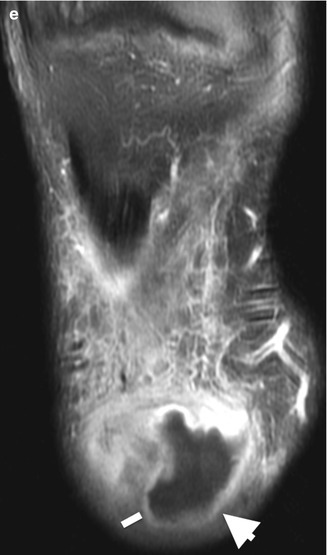
Fig. 13.4
A diabetic patient with right below-the-knee amputation presenting with soft tissue swelling, erythema, and fever. (a) Lateral radiograph stump demonstrates distal soft tissue swelling of increased density (arrowheads) when compared to adjacent soft tissue suggesting collection and underlying cortical irregularity, subtle periosteal reaction (dashed arrow), and adjacent mixed sclerosis and lucency in keeping with osteomyelitis. MRI of the same patient on the same day. (b) Axial T2FS with heterogeneous soft tissue collection (arrowheads), mild muscular edema (myositis), and subcutaneous edema (cellulitis) which enhance on T1FS PG. (c–e) The collection (line) demonstrates low central SI on (e) with rim enhancement (arrowhead) in keeping with a subcutaneous abscess (dashed arrow demonstrates adjacent osteomyelitis)
Radiographs are always the first-line examination when assessing for the presence of osteomyelitis, though notably sensitivity is low, and a normal x-ray result does not rule out the presence of osteomyelitis, particularly in the early stages (i.e., the first 1–2 weeks). There may be soft tissue abnormalities such as swelling if there is an overlying penetrating wound or cellulitis.
Radiographs can reveal soft tissue swelling, regional osteopenia progressing to mixed lucencies with areas of osteopenia and bony sclerosis, and later cortical destruction/erosions. Periosteal reaction is a very important finding and is very suggestive of osteomyelitis in the correct clinical setting. Brodie’s abscess in subacute to chronic osteomyelitis appears as single or multiple radiolucencies surrounded by ill-defined sclerosis. Sequestra, necrotic bone, can be visualized by 6–8 weeks as isolated radiodense fragments surrounded by the involucrum, periosteal new bone. A sinus tract may develop at this time. In TB osteomyelitis and fungal infections, osteopenia is usually present, but there is limited sclerosis or periosteal reaction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree