Fig. 1.1
(a) Ultrasonographic morphology of the normal arterial wall with quantification of the intima–media thickness (IMT). (b) Increased IMT with destruction of the normal artery morphology
Fig. 1.2
Progression from the normal arterial wall morphology to atheromatous plaque
More advanced (Figs. 1.2 and 1.3) or complicated lesions result from persistence of the injury mechanisms to the arterial wall, promoting an inflammatory reaction with development of neovascularization from the vasa vasorum which can also be detected in vivo by enhanced color-flow Doppler imaging technologies using microparticles [19] or by using micro-CT assessment of symptomatic coronary arteries [20]. Extensive plaque neovascularization in carotid endarterectomy specimens was predictor of late cardiovascular events [21]. This process is associated with higher production of several proteases and other enzymes inducing cell destruction and loss of tensile strength of the plaque by the hemodynamic stress resulting from flow disturbances which lead to rupture of the fibrous cap, intraplaque hemorrhage, and thrombosis inside the lesion and at its surface [22–24] as shown in Fig. 1.3b, c.


Fig. 1.3
(a) Stable carotid plaque. (b) Carotid lesion with intraplaque hemorrhage. (c) Carotid plaque showing extensive surface thrombosis (atherothrombosis)
These morphologic changes lead to an increase in the volume of the lesion, rupture of the plaque with extrusion of material from its core nucleus, associated thrombosis and increased severity of the stenosis, or complete arterial occlusion.
It is important to understand the underlying mechanisms that increase plaque progression and its biological markers in order to improve our capability for its recognition.
The concept of vulnerable plaque introduced by Fuster and others [25, 26] shifted the emphasis from degree of stenosis to plaque composition and structure, which increases the risk of rupture and associated clinical acute events.
The major determinants of plaque’s vulnerability to rupture may be listed as follows [26]:
Size and location of the core nucleus rich in lipids and cell debris.
Thickness and collagen content of the fibrous cap overlying the core.
Exposure of plaque components to circulating blood, which have a potent thrombogenic effect.
Active inflammatory and immunological processes resulting from increased deposition and activation of macrophages, T lymphocytes, and mast cells.
Systemic thrombotic propensity from the individual patient.
In vivo detection of plaque morphology, recognition of individual inflammatory activity, and immunological status plus increased propensity to intravascular thrombosis completely changed the scope of diagnostic methods in atherosclerosis. The challenge is no longer the assessment of severity of stenosis and its hemodynamic effect but the identification of these potentially dangerous lesions, which are associated with increased risk of adverse clinical events.
The new developments on imaging technology, both morphological and functional, will be briefly dealt subsequently.
3 Imaging Technologies
3.1 Arteriography
Introduced by Egas Moniz in 1926 [31] for the diagnosis of brain tumors it provided the first clinical correlations between ischemic stroke and occlusion of extracraneal internal carotid [32]. It was subsequently extended to visualize the abdominal aorta and peripheral arteries [33]. Selective intra-arterial catheterization by Seldinger [34] provided an extraordinary expansion of the arteriographic method, which for decades was only available method to study atherosclerosis in vivo (Fig. 1.4).


Fig. 1.4
Arteriography of the carotid bifurcation with tight stenosis in the origin of the internal carotid artery
The development of arterial reconstructive surgery, from endarterectomy introduced by Cid dos Santos in 1946 [35] and bypass techniques popularized by M.E. DeBakey in the early 1950s, to present-day endovascular intervention rested upon arteriography.
Arteriography is a luminography: its images are of the contrasted blood flow and indentations upon the circulating flow produced by the diseased arterial wall. It does not provide any image of the vessel wall and nature of the disease, but only its effect upon blood flow.
It does not also provide accurate information on plaque morphology characteristics relevant to clinical management as previously described, although the presence of irregularities and/or ulceration in carotid arteriography performed within the scope of the ECST trial were markers of higher risk for stroke in the medical arm of the study [36].
Its invasiveness, toxicity associated with contrast injection, X-ray exposure, and high costs have reduced its scope for diagnostic purposes. In today’s clinical practice conventional or digital arteriography for management of atherosclerotic patients is part of the interventional treatment procedure aimed to correct both occlusive and dilating disease.
3.2 CT Angiography and Magnetic Resonance Angiography
New developments in computed tomography technology including multi-detector CT and ECG-gated CT for accurate visualization of coronary circulation provided an useful tool to study atherosclerosis by combining flow assessment with arterial wall imaging (Fig. 1.5a, b).
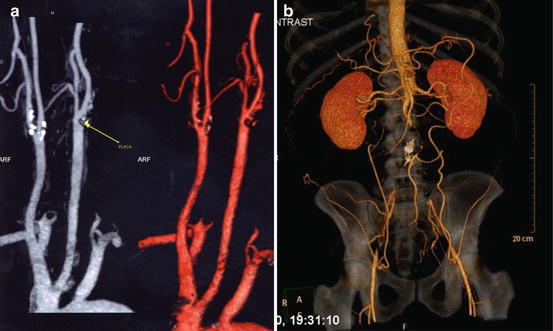
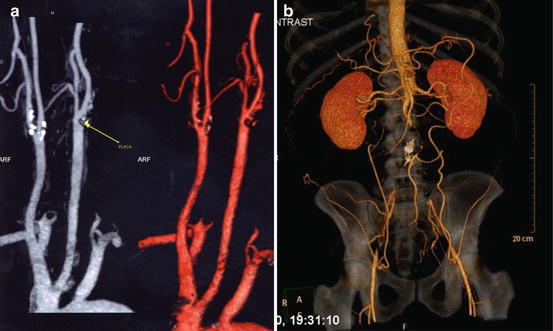
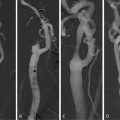
Fig. 1.5
(a) CT-angio of the supra-aortic trunks (calcified carotid plaques). (b) CT-angio of the abdominal vessels (aortic thrombosis)
Identification of plaque morphology in carotid bifurcation disease using CT angiography (CTA) provided identification of intraplaque hemorrhage and ulceration confirmed by histology [37].
For coronary circulation CTA has been correlated with conventional arteriography and used to quantify the calcium content of the lesions (calcium score) and to correlate with symptoms.
A recent trial [38] using a 64 row multi-detector CTA confirmed its accuracy for identification of coronary stenosis and to assess disease severity in symptomatic patients with calcium score <600, but could not replace conventional coronary angiography because of negative predictive value of 83% and positive predictive value of 91%.
Failure to use this technology to identify vulnerable plaques and to discriminate between fibrous tissue and lipids was reported [39], although experimental evidence for the detection of macrophages in a rabbit model of atherosclerosis [40].
For peripheral lower limb arterial disease CTA provides acceptable visualization of the arteries useful for planning the treatment particularly in the absence of extensive calcification.
Although less invasive than conventional arteriography, CTA requires iodine contrast use and radiation exposure which limits its use.
Magnetic resonance imaging is safer, without conventional radiation and less toxic contrast agents. It provides flow images equivalent to conventional arteriography, with better visualization of low flow perfusion situations, like in critical lower limb ischemia, but it has limitations for the assessment of coronary circulation due to its low specificity [41]. Technical refinements provided suitable information to assess arterial remodeling in the presence of moderate stenosis [42] and to characterize unstable fibrous caps in advanced carotid atherosclerosis [43].
New molecular imaging tools and the use of nanotechnology are promising developments for MR imaging of atherosclerotic lesions and to provide more objective identification of markers of plaque vulnerability [44, 45] both in animal models and in humans.
However, this is an expensive technology and time-consuming, which reduces its applicability for routine clinical use.
3.3 B-Mode High-Definition Ultrasound and Color-Flow Duplex Scan
Color-flow duplex scan (CF DS) provides accurate visualization of the arterial system, from extracraneal to intracranial vessels from abdominal aorta and its major visceral branches to the arteries of both upper and lower limbs. It provides visualization of the arterial wall and its changes as well as the flow abnormalities directly induced by the lesions.
Extensive literature has been published to validate objective criteria from flow velocity changes to quantify the degree of stenosis [46–49] from carotids to renal and mesenteric circulation to peripheral limb occlusive disease.
Accurate quantification of stenosis severity is a key factor for clinical management in carotid bifurcation disease and it is extensively dealt in another chapter.
However high-definition B-mode echography offers an objective, noninvasive, reliable, and inexpensive tool to identify early atherosclerotic lesions (Fig. 1.1) and to measure intima–media thickness (IMT) a powerful marker of late occurrence of cardiovascular events. It also provides an objective quantification of the total atherosclerotic burden by using as windows to the arterial system, both the common carotid and femoral bifurcations [50, 51].
By using computerized technology and image standardization of carotid bifurcation plaques (Fig. 1.6a, b) it is possible to quantify the echogenicity of the plaque, to assess its homogenous or heterogeneous quality, and to identify markers of plaque vulnerability and obtain correlations with its biochemical composition and clinical outcomes [28, 30, 52–60].
Fig. 1.6
(a) Homogenous carotid plaque visualized by high-definition ultrasonography. (b) Computer-assisted plaque analysis. (c) Activity index
In a previously published report using computer-assisted HD echography we described ultrasonographic equivalents to histological markers of lesion instability and showed a good separation between symptomatic and asymptomatic lesions and also a positive correlation with ipsilateral brain hemispheric infarcts [28, 61, 62].
Extending further the analysis an indicator of plaque activity was obtained [63]—Activity Index—which had an excellent correlation with appropriate neurological symptoms and was a predictor of late ipsilateral cerebrovascular events in asymptomatic patients followed for a period of 4 years (Fig. 1.6c).
Recently the ACSRS trial was published [64] providing evidence on the value of plaque morphology analysis to stratify clinical and neurological risk in asymptomatic patients with carotid bifurcation stenosis >50%.
Also the efficacy of lipid-lowering agents like statins can be monitored by changes in echogenicity of the plaque and increased thickness of the fibrous cap [65].
There is now substantial evidence pointing to the possibility of this simple, noninvasive, and inexpensive technology to provide adequate imaging for atherosclerotic lesions in accessible sites, accurate measurements of lesion severity, and its direct hemodynamic repercussion and to obtain reliable information on plaque structure to identify vulnerable/unstable plaques.
Using a 2 MHz probe and injecting echogenic particles it has been possible to identify increased vascularization in segments of unstable carotid plaques, which could be a marker of active inflammation [66].
3.4 Intravascular Ultrasound
This is an invasive technology catheter-based providing two-dimensional and cross-section images of the arteries, thus providing accurate measurement of stenosis severity and plaque volume. It has been used associated with catheter-based techniques to improve selection of lesions for treatment and for completion assessment following interventional procedures [67].
Advances in intravascular ultrasound (IVUS) technology with spectral analysis of the signals provide plaque characterization and evaluation of its composition, which has been referred as Virtual Histology [68].
Several studies have provided validation of this technology. However it is invasive, expensive, and not suitable for routine clinical use and epidemiological studies.
3.5 Optical Coherence Tomography
It is an optical analogue of intravascular ultrasound with excellent spatial resolution and providing also a cross-sectional image of the artery [69].
Its clinical advantage seems to provide completion assessment following angioplasty and stent deployment in both coronary and carotid arteries and to identify intimal hyperplasia in early re-stenosis.
3.6 Fluorescence Imaging
This technology is available and provides the visualization of the inflammatory reaction within the plaque. [70] and visualize the inflammatory reaction within the plaque. It targets molecules and follows its incorporation and degradation in the structures. Its use has been experimental to test new imaging tools, but the recent developments with catheter technology allowed incorporation of a fluorescence probe which can be directed to coronary or other arterial bed. By injecting fluorochromes and activating them with the laser probe it is feasible to track down enzymes or other molecules involved in plaque instability [71].
3.7 Nuclear Imaging PET-SCAN
Single photon emission computed tomography (SPECT) and PET imaging of vascular structures have improved their sensitivity and accuracy by accurate anatomic location of the radiation source. Using 18 FDG (fluorodeoxyglucose), which is taken by active cells, has provided interesting images of carotid plaques correlating with neovascularization [72, 73]. It targets individual molecules involved in different metabolic pathways (VCAM-1), which adhere to endothelial cell in early atherosclerosis.
These technologies are promising tools for research, but its use in clinical practice requires further improvements on its sensitivity and specificity and also easier and less expensive instrumentation.
We have briefly described several technologies, some already tested in clinical studies and used in practice, and others still within the realm of experimentation and animal models.
There is a fundamental need to achieve better diagnosis of the unstable plaque, which often is not associated with severe stenosis and is a major cause of atherothrombosis and leads to acute cardiovascular events.
Some of the technologies provide only morphological imaging, but a new era of functional biological imaging is beginning with new optical devices and nuclear-based technology often used with combined MR and CT Imaging to achieve better resolution and accuracy. They offer new ways to visualize the ongoing metabolic process that leads to the morphological changes that are markers of plaque instability.
Also a new area of clinical research will be the combined use of these technologies with biomarkers of inflammation like CPR or others, which may help to identify the vulnerable lesions and the patients at a higher risk of cardiovascular events.
The road from arteriography to molecular and biological imaging is fascinating and provides a good example of translational research from the bench and animal experiments to the bedside, by allowing a better selection of patients who really need of interventional treatment and thus saving a relevant number from unnecessary procedures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree