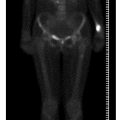
Fig. 1
68Ga- DOTANOC (DOTA-Tyr3-octreotide) positron emission tomographycomputed tomography in metastatic carcinoid. Metastatic disease in the liver and bone. There is an example of an early small metastasis in the left scapule (for color reproduction see p 312)
Response of bone metastases after treatment with 177Lu-octreotate can be evaluated efficiently by SRS or 68Ga-somatostatin PET [13]. Interestingly, in a recent study, it has been suggested that successful treatment of bone metastases can represent as lesions that increase in size on CT as a result of the repair process while showing a decrease in labeled somatostatin uptake [14].
18F-fluoride is a PET bone-seeking agent with uptake mechanism similar to that of the single-photon emitting tracer 99mTc-MDP. Fluoride ions exchange with hydroxyl groups in hydroxyapatite crystal bone to form fluoro — apatite, and are deposited at the bone surface where bone turnover is greatest. Similar to 99mTc-MDP, accumulation of 18F-fluoride uptake in bone metastases reflects increased regional blood flow and high bone turnover. 18Ffluoride has better pharmacokinetic characteristics compared with those of 99mTc-MDP. The bone uptake of the former is twofold higher, and in contrast to 99mTc-MDP it does not bind to protein. The capillary permeability of 18F-fluoride is higher and its blood clearance is faster, resulting in a better target-to-background ratio. Regional plasma clearance of 18F-fluoride is reported to be three to ten times higher in bone metastases compared with that in normal bone [15, 16]
18F-fluoride PET is very sensitive for detection of osteoblastic metastases and also lytic metastases, as the latter, even when considered “pure lytic”, do have minimal osteoblastic activity, which is enough for detection by 18F-fluoride PET. It should be borne in mind that 18F-fluoride is not tumor specific and therefore is a sensitive modality for detection of any bone abnormalities, not only malignant abnormalities.
When interpreting 18F-fluoride PET-CT for assessment of metastatic skeletal spread, the morphologic appearance of the bone should be carefully considered on the CT data, in order to accurately separate benign and malignant sites of 18F-fluoride uptake [17].
Several clinical reports in various malignancies have illustrated the superiority of 18F-fluoride PET-CT over BS for detection of bone metastases, with an excellent negative predictive value [18–21]. In patients with prostate cancer, 18f-Fluoride PET-CT showed a greater sensitivity than 18F-fluorocholine in the detection of bone metastasis, although the differences were not statistically significant [22]. In patients with lung cancer, it was found to be complementary to 18F-FDG PET-CT mainly for detection of sclerotic type abnormalities [23].
There are early data suggesting that 18F-fluoride PET can be used to assess treatment response in metastatic prostate cancer. PET was performed 6 and 12 weeks after treatment with Alpharadin® in a small pilot study of patients with prostate cancer. Measurement of serial standard uptake values allowed separation of responders and nonresponders [24].
However, use of 18F-floride PET is not yet routine. There is a multicenter study underway in the USA to assess the use of this modality in routine use of skeletal staging in cancer, comparing 18F-fluoride PET-CT with MDP bone scintigraphy in 500 patients with breast, prostate and non-small-cell lung cancer.
References
1.
2.
Even-Sapir E (2005) Imaging of malignant bone involvement by morphologic, scintigraphic, and hybrid modalities. J Nucl Med 46:1356–1367PubMed
3.
4.
Cook GJR (2010) PET and PET/CT imaging of skeletal metastases. Cancer Imaging 10:153–160PubMedCentralCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree