Fig. 11.1
CE1 type of hydatid cyst. (a) Axial T2-weighted MRI shows a large well-defined unilocular cystic lesion in the right parietal region with thick hypointense wall and mild marginal edema. (b) Post-contrast axial T1-weighted MRI shows homogenous low signal intensity of the cyst with mild marginal contrast enhancement
The CE2 cyst: It appears as a unilocular maternal cyst with peripherally arranged broad daughter vesicles. The presence of smaller daughter cysts within the primary maternal cyst is considered to be pathognomonic of a hydatid cyst. It signifies an attempt at survival by a damaged or dying cyst. Daughter vesicles (broad capsules) are small spheres that carry the protoscoleces. Daughter vesicles are formed from internal budding of the germinal layer. The wall of the daughter cysts appears as low signal intensity (Abdel Razek et al. 2009, 2011). A high-signal-intensity rim may be seen around the maternal cyst on T2-weighted images. This is explained by degenerating larvae releasing metabolic products that disrupt the blood-brain barrier with host inflammatory response (Fig. 11.2).
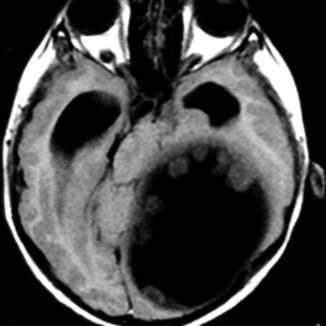
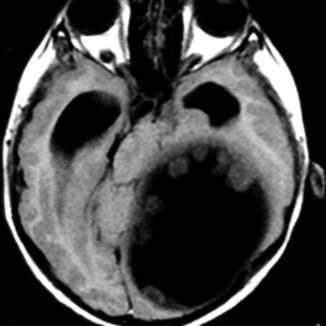
Fig. 11.2
CE2 type of hydatid cyst. Axial T1-weighted MRI shows a large maternal cyst with small peripherally arranged daughter vesicles
The CE3 type: It develops from rupture of the primary cyst with endocystic proliferation of the hydatid cyst, and the cyst contents are confined within the pericyst, resulting in maternal cyst with multiple large daughter cysts. The maternal and daughter cysts are isointense on both T1- and T2-weighted images. When the daughter cysts completely fill the maternal cyst, the cysts appear as multiseptated and may produce “grapelike,” “wheel-like,” “rosette-like,” or “honeycomb-like” structures (Abdel Razek et al. 2009, 2011) (Fig. 11.3).
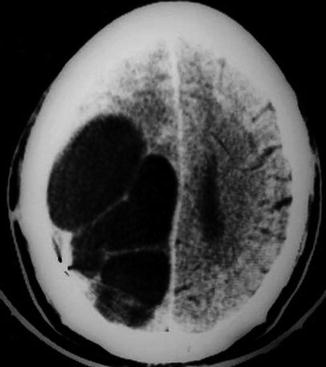
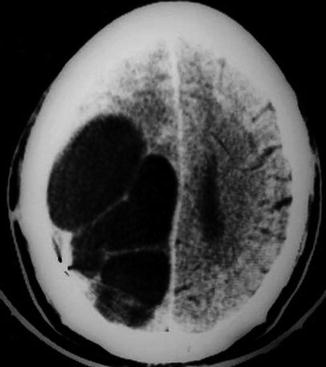
Fig. 11.3
CE3 type of hydatid cyst. Axial CT scan of the brain shows a large cyst with honeycomb appearance after surgery
The CE4 type: It appears as a cystic lesion with serpentine bands or floating membranes representing the detached or ruptured membranes. When the viability of the parasite is lost, the intracystic pressure is lowered and the endocystic membranes are detached and float freely. Intracystic wavy or serpentine bands (“water-lily sign”) may appear, representing the delaminated germinal layer and rupture of the membranes. The presence of detached membranes with a ball-of-wool appearance is a sign of severe degeneration. Degenerated cysts consist of a heterogeneous, solid-looking pseudotumor that may show a “ball-of-wool sign” as the cystic lesion gradually becomes smaller and solidifies. Degenerating cysts show wavy or serpentine bands or floating membranes representing the detached or ruptured membranes (Abdel Razek et al. 2009, 2011) (Fig. 11.4).
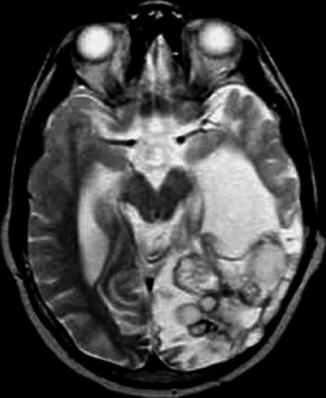
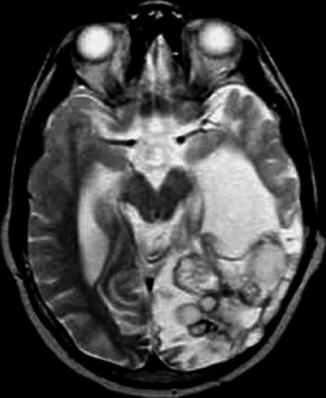
Fig. 11.4
CE4 type of hydatid cyst. Axial T2-weighted MRI shows a large cyst with ball-of-wool appearance in the left occipital region
The CE5 type: It is the infertile and dead form of CE. The dead cysts are characterized by a thick calcified wall in 50 % of patients. The degree of calcification varies from partial to complete calcification of the cyst. CT scan is best for detection of calcification. On MRI, the calcified lesion appears as signal void region (Abdel Razek et al. 2009; Basraoui et al. 2010; Bartosch et al. 2011) (Fig. 11.5).
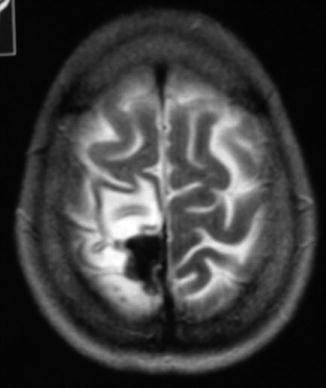
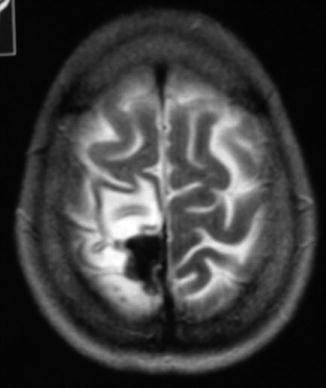
Fig. 11.5
CE5 type of hydatid cyst. Axial T2-weighted MRI shows a hypointense calcified dead cyst in the brain
Advanced Magnetic Resonance Imaging
Magnetic Resonance Spectroscopy
MRS may be added to the routine MRI protocol for a more accurate etiological diagnosis of a cystic lesion. MRS of cerebral CE shows dominant resonances of acetate (1.92 ppm), succinate (2.4 ppm), lactate (1.33 ppm), and glycine (3.56 ppm) and small contributions from alanine and isoleucine, leucine, and valine. The most specific metabolite of CE is a peak of succinate (2.4 ppm); however, a succinate peak has also been seen in pyogenic abscesses and neurocysticercosis. Other less-specific metabolites, such as lactate and acetate, are suggestive of infectious diseases. MRS studies ex vivo have found malate (4.3 ppm) and fumarate (6.5 ppm) in fertile cysts (Garg et al. 2002; Chawla et al. 2004; Hosch et al. 2008).
Diffusion Magnetic Resonance Imaging
CE is isointense with cerebrospinal fluid at diffusion-weighted MRI. The apparent diffusion coefficient (ADC) value of CE is 1.33 ± 0.15 × 10−3 s/mm2 (Kittis et al. 2004).
Special Types
Multiple Hydatid Cysts
Multiple cerebral hydatid cysts, secondary or primary, are rare. Secondary infertile cysts are due to the surgical, spontaneous, or traumatic rupture of a viable primary lesion with spilling of the scolices inside the cerebral parenchyma, while multiple primary cysts result from embolization of a ruptured cardiac cyst (Al Zain et al. 2002; Lotfinia et al. 2007; Yurt et al. 2007) (Fig. 11.6).
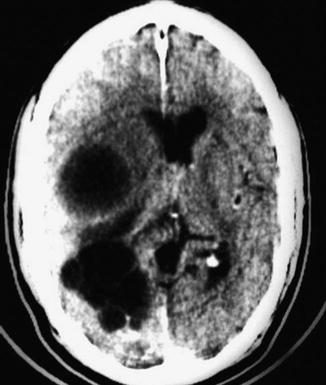
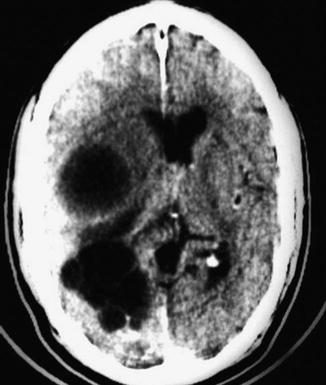
Fig. 11.6
Multiple hydatid cysts. Axial CT scan of the brain shows multiple hydatid cysts are seen in the right cerebral hemisphere
Extraparenchymal Hydatid Cyst
The reported sites of extraparenchymal hydatid cyst include the subarachnoid space, cisterns, ventricles, pons, cerebellum, aqueduct of Sylvius, extradural space, and diploic space of skull bones (Diren et al. 1993; Tsitouridis et al. 1997; Lakhdar et al. 2010; Wani et al. 2010). Cranial extradural hydatid cyst is extremely rare because the physiologic flow of blood to the brain is mainly through the internal carotid system, so the likelihood of the larvae traveling through the external carotid system is very low (Cemil et al. 2009; Turgut 2010). Primary calvarial hydatid cysts arising from the dipole of the cranial bones with intracranial extension are extremely rare (Erman et al. 2001; Sharma et al. 2011). Different forms of extraparenchymal hydatidosis is discussed in detail in Chap. 21.
Infected Hydatid Cyst
When a secondary process occurs in the cyst, such as infection or rupture, the signal intensity tends to be slightly decreased on T2- and a little higher on T1-weighted images. When rupture, superinfection, or hemorrhage occurs in the cyst, the signal intensity may be slightly decreased on T2-weighted images and slightly increased on T1-weighted images (El-Shamam et al. 2001).
Stroke
Embolic stroke due to rupture of a hydatid cyst in cardiac cavity, a cause of ischemic infarction and multiple metastatic cyst formation, is an extremely rare entity (Martin et al. 1996; Turgut and Bayülkem 1998). Stroke as a complication of cardiac hydatidosis is discussed in detail in Chaps. 21 and 22.
Differential Diagnosis
CE on CT needs to be differentiated from porencephalic cyst, arachnoid cyst, brain abscess, and cystic tumor. Porencephalic and arachnoid cysts are not spherical and are not surrounded entirely by brain parenchyma. Porencephalic cyst shows signs of volume loss and gliosis in adjacent white matter. Arachnoid cyst is extra-axial in location, whereas intra-axial hydatid cyst is surrounded by brain parenchyma all around. Cystic tumor and brain abscess show definite contrast enhancement in the wall and/or mural nodule; perilesional edema is also present in case of abscess (Wani et al. 2010; Bartosch et al. 2011). The presence of multiple daughter cysts and hypointense ring in T2-weighted imaging is characteristic of CE (da Rocha et al. 2005).
Posttreatment
Methods
The treatment of cerebral CE is surgical and the aim of surgery is to excise the cyst completely without rupture to prevent anaphylactic reaction and local recurrence. The most commonly utilized surgical procedure designed to remove the intact cyst completely without rupture is by irrigating saline into the interface between the cyst wall and brain. However, medical treatment with albendazole has been reported with favorable results as an adjunct and, in certain circumstances, as the primary mode of treatment (Wani et al. 2010; Bartosch et al. 2011).
Surgical
The complications of hydatid cyst surgery are various and depend on the location, size, and multiplicity of the cysts. Intraoperative cyst rupture is the most common and serious complication which can lead to widespread dissemination followed by severe inflammatory or anaphylactic response. Subdural effusion occurs due to rapid drop of the intracranial pressure after the removal of the cyst with opening up the subdural space. Porencephalic cysts are abnormal brain cavities resulting from trauma and iatrogenic (postoperative) or perinatal vascular occlusion. These cavities are filled with cerebrospinal fluid and commonly connected with ventricles or subdural spaces (Fig. 11.7




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree