Pre- and postoperative imaging is increasingly used in plastic and reconstructive surgery for the evaluation of bony and soft tissue anatomy. Imaging plays an important role in preoperative planning. In the postoperative setting, imaging is used for the assessment of surgical positioning, bone healing and fusion, and for the assessment of early or delayed surgical complications. This article will focus on imaging performed for surgical reconstruction of the face, including orthognathic surgery, facial feminization procedures for gender dysphoria, and face transplantation.
Key points
- •
Three commonly used orthognathic procedures include the Le Fort type I osteotomy, bilateral sagittal split osteotomy (BSSO), and osseous genioplasty. These procedures are used to correct deformities of the midface, lower face, and chin, respectively.
- •
Reference to the surgeon’s operative note, or direct communication with the surgical team is extremely helpful and highly recommended to avoid language in the imaging report which may be incorrect, misleading, or results in unnecessary patient concern or confusion.
- •
Commonly addressed areas in facial feminization surgery (FFS) include the frontal and periorbital region, the nose, chin, and jawline, as these areas have been shown to play an important role in gender discrimination.
- •
Interdisciplinary preparation for the face transplant recipient and donor imaging is of paramount importance for operative planning.
- •
At our institution, preoperative imaging for both the donor and recipient consists of a high-resolution craniofacial CT, arterial, and venous phase CT angiogram of the head and neck, and 6-vessel digital subtraction angiography (DSA).
Introduction
Pre- and postoperative imaging is increasingly used in plastic and reconstructive surgery for evaluation of bony and soft tissue anatomy. Imaging plays an important role in preoperative planning and can also be used for computerized surgical planning and 3D modeling. In the postoperative setting, imaging is used for the assessment of surgical positioning, bone healing and fusion, and early or delayed surgical complications. This article will focus on imaging performed for surgical reconstruction of the face, including orthognathic surgery, facial feminization procedures for gender dysphoria, and face transplantation.
Orthognathic surgery
Orthognathic surgery involves repositioning of the maxilla and mandible to correct facial deformities that may be genetic, posttraumatic or otherwise cosmetically or functionally impairing. The maxilla and mandible, or components of each, can be deficient or excessive in any of the 3 orthogonal planes resulting in facial deformity of various types, and often dental malocclusion. Multiple surgical options are available for correcting dentofacial deformities; however, 3 commonly used procedures include the Le Fort type I osteotomy, the bilateral sagittal split osteotomy (BSSO), and osseous genioplasty. The Le Fort type I osteotomy is used to correct deformities of the midface, whereas the BSSO and osseous genioplasty involve the lower face and chin, respectively.
At our institution, a noncontrast craniofacial CT [ Box 1 ] is often performed preoperatively, particularly for patients with complex syndromic conditions such as Treacher Collins, Crouzon, or Apert syndrome. CT imaging is also frequently performed in the immediate postoperative period to assess overall osseous alignment and hardware positioning, or performed in the delayed setting if there is a concern infection, nonunion, or hardware fracture.
- •
Helical scan from vertex to below mandible, include entire face and calvarium in anteroposterior dimension
- •
Slice thickness 0.75 mm. Axial, coronal, sagittal reconstruction in soft tissue and bone windows
- •
Voltage ∼120kVp, Reference mAs ∼300
- •
3D volumetric images created on a separate workstation and sent to PACS
Le Fort type I osteotomy
The Le Fort type I osteotomy allows the manipulation of the position of the upper lip and nose without affecting the orbit and zygomatic region. The surgeon may use Le Fort type II or III procedure to alter the nasomaxillary region, or the orbits and zygoma, respectively. A typical Le Fort type I osteotomy is a horizontally oriented maxillary osteotomy, approximately 5 mm above the tooth root apices, involving the inferior aspect of the nasal septum, the lateral nasal walls, and the anterior and posterolateral maxillary sinus walls to the junction of the pterygoid plates and maxillary tuberosity. , As opposed to the classic Le Fort fracture patterns, the Le Fort type osteotomies typically do not include the pterygoid plates, though unintentional fractures through the pterygoid plates do occur and may be encountered on postoperative imaging. , Positioning of the anterior nasal spine affects the nasolabial angle and may or may not be included in the osteotomized segment. The maxilla can be advanced, vertically distracted, or segmented and laterally distracted to correct maxillary hypoplasia. Similarly, impaction or bone removal can be used to decrease dental protrusion and correct vertical maxillary excess or a long inferior face; rotation or asymmetric positioning can be used to correct a slanted bite or asymmetric face. , ( Figs. 1–4 ). During surgery, impacted third molar teeth may be removed, or large inferior turbinates may require reduction.




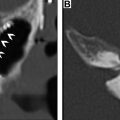
At our institution, imaging is often performed in the immediate postoperative period (usually postoperative day 1). Prominent, extensive soft tissue edema and infiltration, and high-density fluid levels in the sinuses are expected findings. However, larger hematomas or hemorrhages can occur and may be venous or arterial, involving the pterygoid plexus, the internal maxillary artery, or palatine branches arising from the facial, ascending pharyngeal, or maxillary arteries. , , Arteriovenous fistulas and pseudoaneurysm related to orthognathic surgery have been described and may not be obvious at the time of the surgery due to the deep location of the vessels, or may occur in the delayed postoperative setting ( Fig. 5 ). Recurrent epistaxis should raise suspicion for a vascular injury and CT or conventional angiography should be considered with attention to appropriate regional vessels.

Asymmetric osteotomies, step-off, or gaps between bone segments are frequently intentional and should be noted, but not reported as abnormal findings. Reference to the surgeon’s operative note or direct communication with the surgical team is extremely helpful and is highly recommended to avoid language in the imaging report which may be incorrect, misleading, or results in unnecessary patient concern or confusion. Knowledge of expected osteotomy patterns is helpful to avoid mislabeling osteotomies as fractures. Mild comminution at the level of the osteotomies, particularly involving the thinner maxillary sinus walls or nasal septum, is also frequently encountered. However, both unplanned fractures and fracture fragment displacement do occur and should be described, particularly if extending to the skull base, vascular canals, or orbit, as this may require a return to the operating room ( Fig. 6 ). Separation of the pterygomaxillary junction is technically challenging and may result in uncontrolled fractures through the maxillary tuberosity or pterygoid plates, which may contribute to operative complications.

Other described complications that may present in the later postoperative period include oronasal fistulas following palatal expansion with sagittal segmental maxillary osteotomies, or alveolar/periodontal bone loss or dental devitalization due to vascular compromise. ,
Bilateral sagittal split osteotomy
The BSSO originally described by Obwegeser in 1955 is used to correct mandibular retrognathism or prognathism by advancement or setback, respectively, of the mobilized mandibular arch. The procedure involves horizontal osteotomies through the medial half of the mandibular rami, and sagittally oriented osteotomies through the ramus and posterior mandibular body, anteriorly exiting the buccal cortex and posteriorly involving the lingual cortex, separating the tooth-bearing portion of the mandible from the bilateral lateral ramus segments. The horizontal osteotomy is performed superior and posterior to the mandibular foramen. The sagittal osteotomy should be lateral to the course of the inferior alveolar nerve to avoid injury (see Figs. 1–4 ; Fig. 7 ).

Unanticipated fractures during a BSSO may involve the condylar neck, the buccal plate, or lingual plate. The inferior alveolar nerve is at high risk during a BSSO, and violation of the mandibular foramen or nerve canal by the osteotomy, fixation hardware, or unintentional fractures may occur and should be communicated to the surgeon ( Fig. 8 ). Arteries at risk during the procedure include the inferior alveolar artery, facial, lingual, and internal maxillary arteries.

Condylar resorption has been described by several authors following orthognathic surgery including the BSSO and Le Fort type I osteotomy and is a risk factor for relapse of maloccusion. Condylar resorption can occur from 6 months postoperatively to well beyond the first postoperative year. Findings on CT include unilateral, bilateral, or asymmetric flattening and erosion of the condyle in anteroposterior, transverse, or craniocaudal dimensions.
Osseous genioplasty
The osseous genioplasty involves a horizontal osteotomy through the anterior inferior mandibular body 5 to 6 mm below the tooth root apices and mental foramen. The separated segment can be advanced or distracted to correct a small chin in the anteroposterior or craniocaudal dimensions, set back for an overly prominent chin, or tilted in the horizontal plane to correct an asymmetry. Parallel osteotomies may be used for a stepwise advancement, or to remove bone to decrease vertical height of the chin.
As described above, the mobilized osseous segments during orthognathic surgery can be variably set, rotated, or further segmented depending on the unique anatomy of the patient; therefore, the radiologist should be aware that gaps, asymmetry, or step-offs can all be expected postoperative findings and should not be referred to as malalignment. Similarly, depending on surgeon preference, bone graft, resorbable, or titanium plates, in variable bent or prefabricated shapes and configurations, may be used (see Figs. 1–3 ).
For any of the above procedures, additional pertinent postoperative imaging findings may include temporomandibular joint dislocation, particularly in the immediate setting, evidence of soft tissue infection, osseous nonunion, hardware loosening, infection, or fracture. Careful evaluation should also be conducted for areas of bone loss or erosion as this may reflect underlying osteomyelitis or avascular necrosis, and may result in delayed complications including relapse of the corrected facial deformity.
Facial feminization surgery
Gender-affirming surgery in the transgender population is being increasingly used in the United States. At our institution, the transgender health program performs upwards of 550 gender-affirming surgeries per year, mirroring trends in the overall US population. , Facial reconstruction procedures are an important component of treatment options available for gender dysphoria and have been shown to improve psychosocial metrics in the transgender population. , Procedures for the male to female transition more commonly involve osseous reconstruction or remodeling, and therefore are more likely to use pre- and postoperative imaging than procedures for the female to male transition, which rely more heavily on soft tissue-based remodeling with injectable fillers and lipotransfer.
Facial feminization surgery (FFS), more inclusively referred to as facial gender confirmation surgery, includes a conglomerate of procedures aimed to address the phenotypically male characteristics of the craniofacial skeleton and soft tissues. Head and neck radiologists should be familiar with the types of procedures performed and pre- and postoperative considerations that may be relevant for the referring surgeon.
Imaging considerations and protocol
Care and considerations should be taken before, during, and after imaging to ensure a positive health care experience and to avoid transgender discrimination. Front desk staff, technologists, nurses, and radiologists should be educated regarding the needs and experiences of the transgender population. All staff should seek out and use the preferred pronoun of the patient, which at our institution is indicated in the patient’s electronic medical record. Similarly, the imaging facility must be appropriately equipped with gender-neutral bathrooms and changing areas to promote an inclusive environment.
A preoperative craniofacial CT is performed on all potential candidates for facial feminization procedures. The study is used to identify key features which may impact the type of procedures best suited for the individual needs and anatomy of the patient. Additionally, the craniofacial CT can be used with image-guided surgical navigation software for the construction of individualized surgical cutting guides, hardware, or implants, or used in a more qualitative fashion depending on the preference of the individual surgeon. The radiologist can highlight salient anatomic features which may be relevant to presurgical planning, and identify pathology which may need to be addressed before surgery, or may pose additional challenges during surgery. 3D volumetric images are also helpful for patients to visualize their own bony anatomy and understand planned surgical procedures.
Surgical procedures and relevant imaging findings
The most common areas addressed in FFS include the frontal and periorbital region, the nose, chin, and jawline, as these areas have been shown to play an important role in gender discrimination.
Upper face
The forehead and supraorbital region contribute strongly to gender identity. A prominent supraorbital rim with frontal bossing and a more narrow nasofrontal angle have been shown to confer masculinity, whereas a smooth, gently curved forehead contour with a relatively wider nasofrontal angle is associated with female gender ( Fig. 9 ).