 Clinical Indications
Clinical Indications
The role of ultrasound in hand and finger imaging is progressively growing. Although much of the current imaging is still based on radiography in terms of traumatic injury and rheumatology, there has been definite recognition of the importance of visualization of the soft tissues, as well as imaging during dynamic movement, both of which are well demonstrated with ultrasound.
Acute hand and finger injuries would still require radiographs as the initial imaging modality, primarily to identify fractures or radiopaque foreign bodies. However, persistent posttraumatic pain or other symptoms in the absence of fracture or bony injury requires further evaluation. Ligament and tendon injuries make up a significant proportion of cases of dysfunction, which are not directly visible on radiographs other than as bony dislocation or subluxation.
Penetrating injuries by foreign bodies are also a frequently encountered indication for ultrasound imaging. It is not uncommon for retained foreign bodies to be nonopaque on radiographs, usually of organic material such as wooden splinters, plant thorn, insect stings, etc. In addition, the foreign bodies may be in multiple small fragments, each of which needs to be identified and removed, to reduce the risk of infection and inciting an inflammatory response. Ultrasound is able to detect such millimeter-sized foreign bodies, providing the hand surgeon with a road map for removal.
Lumps and bumps on the hand have always been a common indication for ultrasound imaging, with the main intention to identify if it is solid or cystic. Ancillary findings would include the relationship or attachment to the surrounding structures, compressibility, vascularity, and location.
The more diffuse swelling in the hand and fingers is usually due to soft tissue edema. The role that ultrasound is able to contribute is to assess if the edema is related to any particular anatomic structure or underlying injury. Joint effusions and fluid collections can also track within the fascial planes and present as swelling. Inflammatory or rheumatologic conditions may also present as joint swelling.
Erosive arthropathy has also become more often imaged with ultrasound, both by radiologists and rheumatologists. Bony erosions demonstrated on radiographs are a late manifestation of disease, and the direct visualization of soft tissue inflammatory pannus with increased vascularity allows earlier detection and diagnosis.
Biopsy, aspiration, or injection of the hand and fingers is easily done by the clinician, knowing the normal anatomy, and with the target area in a superficial location. Ultrasound-guided procedures are occasionally useful in situations where there is an unexpected “dry tap” of a cyst or collection; ultrasound would then be used to both assess if there is sufficient fluid for aspiration, or if the lesion is solid or a diffuse area of soft tissue edema.
 Technical Guidelines
Technical Guidelines
With the exception of ultrasound of the skin, the hand and fingers provide the next most superficial body part or organ to be imaged. This by itself demands that high frequency (10 mHz or more) be used to provide adequate resolution. Newer transducers that are commercially available have frequencies up to 17 MHz.
The shape or configuration of the transducer probe is also another matter for consideration. A linear array is a definite requirement, and the two most common forms are the larger (6 to 8 cm width) probes (Fig. 4.1A), or the smaller (2 to 3 cm) “hockey-stick” probe (Fig. 4.1B). The hockey-stick probe is named as such due to its angled head in relation to the handle of theprobe. The larger probes allow greater appreciation at any one point due to the larger field-of-view, which is useful in demonstration of the length of a tendon. The hockey-stick probes are easier to manipulate given their small size, but that same factor reduces the field of view in any single image. Multiple images or extended field of view imaging is then needed to cover the same area.
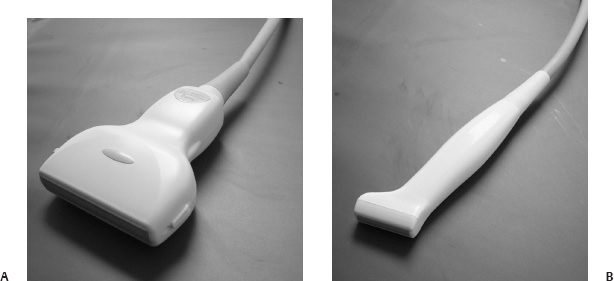
Fig. 4.1 Linear ultrasound probes commonly used in musculoskelet al imaging, with a linear (A) and “hockey stick” (B) configuration.
One of the disadvantages of standard ultrasound of the fingers is that the finger needs to be fully extended to allow adequate contact with the probe surface. This may not be always possible in patients who have joint deformities, and the finger joints are subluxed or held in fixed flexion. There is also another category of patients who may not be able to straighten the finger due to pain or swelling.
Dynamic assessment of the finger tendons for evaluation of integrity and excursion necessitates active or passive flexion and extension of the metacarpophalangeal and interphalangeal joints. This movement will reduce contact of the finger with the ultrasound probe, precluding accurate and detailed visualization. Usage of liberal amounts of ultrasound gel or a stand-off gel pad or plastic block may be able to overcome these factors, but excessive gel may be messy and the ultrasound stand-off pad or block may be difficult to handle and stabilize.
A water bath was used as the original coupling agent in the early development of medical ultrasound scanning in the 1950s, where the patient was placed into a large container filled with water, and the ultrasound probe mounted on a mechanical arm was moved around the patient. Immersion of the hand and fingers into a small water bath is feasible, and part of the ultrasound probe can also be safely immersed underwater, but not up to the junction of the probe and the cable (Fig. 4.2A,B). This will allow water to act as a coupling medium, and there will be no loss of sound wave transmission even with the finger and the probe not being in direct contact (Fig. 4.2C). The finger can then be placed in various degrees of flexion and extension without loss of sound signal, and dynamic movement and assessment can be performed.
The temperature of the water in the water bath should be tepid or around room temperature, for the comfort of the patient. The water bath should also allow the patient to rest the wrist or forearm, rather than having to hold or suspend it up, which can lead to fatigue or movement.
The ability of cine-loop display, recording, and storage has become more important, in tandem with the development of higher-resolution ultrasound of the hands and fingers. Cine-loop display has been facilitated by picture archiving and communication systems (PACS) or by direct recording via a CD/DVD writer built into the ultrasound unit. Tendon excursion and integrity, in particular, are best assessed with active or passive movement of the fingers. Demonstration of movement assists in distinguishing different anatomic or pathologic structures, given that the gray-scale appearance of many of the normal soft tissues in the hand is of similar echogenicity.
Generally, the most comfortable position for both the patient and examiner is to be seated across the couch from each other. This will allow the patient’s forearm and wrist to rest on the couch, and the wrist can be supported by a small sponge. The hand can then be pronated and supinated easily, to allow ready access and quick examination of all the relevant surfaces. The other advantage is that the patient is usually able to see the ultrasound screen, and the radiologist can then choose to show and explain the relevant images to the patient during or at the end of the study.
 Normal Anatomy
Normal Anatomy
Many of the structures in the palm and dorsum of the hand are continuations from the wrist. At the start of the study, it is sometimes better to delineate the anatomy at the level of the wrist, and then trace the structure distally into the hand.
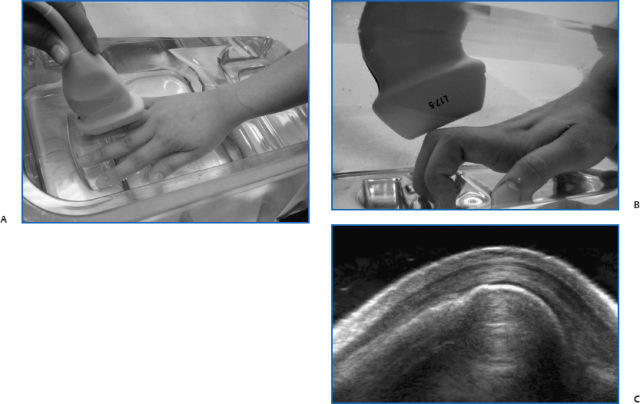
Fig. 4.2 Underwater ultrasound examination showing the position of the hand and ultrasound probe from the top (A) and side (B) views. Ultrasound image in the water bath of the proximal interphalangeal joint in flexion shows ideal coupling with no loss of sound wave (C).
Tendons and Pulleys
The volar flexion tendons to each finger are composed of both the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP). Within the carpal tunnel, all the flexor tendons may not be arranged in any specific order, and it is only by tracing the tendons distally to see which finger it is associated with can one identify each tendon with certainty. Within the palm at the level of the metacarpals, the FDS lies superficial to the FDS (Fig. 4.3A,B). The FDP tendon inserts onto the distal phalanx, whereas the FDS tendon divides into two parts at the level of the metacarpal head, with each passing around the associated profundus tendon on either side, to wind up deeper than the profundus tendon and attaching on to the base of the middle phalanx. This relationship can be shown on transverse images of the flexor tendons, scanning from proximal to distal (Fig. 4.3C,D).
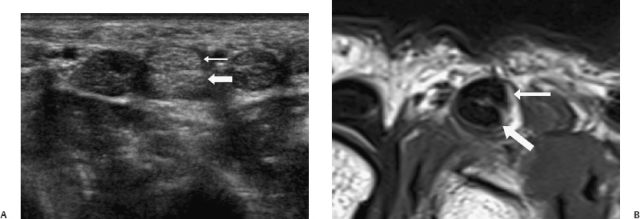

Fig. 4.3 Transverse ultrasound and magnetic resonance images at the palm and along the middle finger showing the relationship of the flexor digitorum superficialis (FDS) and flexor digitorum profundus (FDP) tendons. At the palm, the FDS tendon (thin white arrow) lies immediately superficial to its corresponding FDP tendon (thick white arrow) (A,B). Within the finger, the FDS tendon divides into two (white arrows) and passes around the FDP tendon to end up deep to the FDP before attaching to the middle phalanx (C,D).
In the longitudinal plane, the flexor tendons show a fibrillar echogenic appearance, with the FDP inserting onto the distal phalanx (Fig. 4.4). The flexor tendon sheath around each tendon begins in the palmat the level of the metacarpal neck, and follows the tendon distally. Even with the double layer or synovium, it is extremely thin in the normal state and closely apposed to the flexor tendon.
The flexor tendon of each finger passes through the fibroosseous tunnel, which is formed by the annular and cruciate pulleys, and the palmar cortical surface of the phalanges and palmar plates. The pulleys are condensations of the tendon sheath, and are attached to the adjacent phalanges (Fig. 4.5). There are five annular pulleys designated A1 to A5 and three cruciate pulleys designated C1 to C3, from proximal to distal. The pulleys serve to restrain the flexor tendon, holding it against the phalanges, to prevent bow-stringing on flexion of the finger.
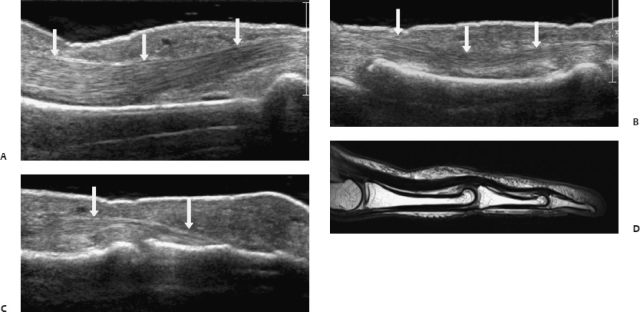
Fig. 4.4 Longitudinal ultrasound (A–C) images and corresponding magnetic resonance (D) image of the normal flexor tendon in the finger (white arrows).
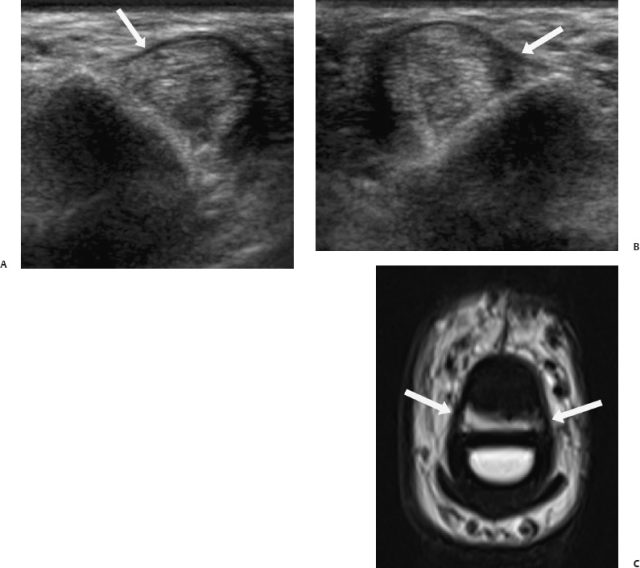
Fig. 4.5 Transverse ultrasound images showing the radial (A) and ulnar (B) aspects of the A2 pulley of the middle finger, with corresponding magnetic resonance (C) image (white arrows). Due to the oblique orientation of the pulleys, it is difficult to image both the radial and ulnar arms on the same ultrasound image.
The A1, A3, and A5 pulleys are sited at the metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints, respectively. The A2 and A4 pulleys are at the level of the midshafts of the proximal and middle phalanges, respectively. The A2 and A4 pulleys are biomechanically the most important, while pathology at the level of the A1 pulley is a common cause of trigger finger.
The course of the flexor tendons are also divided into five zones, which are based on anatomic considerations for tendon injury and repair. The zones are numbered from 1 to 5, from distal to proximal. Zone 1 consists only of the flexor digitorum profundus tendon, at the point distal to the insertion of the flexor digitorum superficialis tendons on the middle phalanx.
Zone 2 extends from the A1 pulley to the level of the middle phalanx, and tendon injury in this region may predispose to formation of adhesions due to the restricted soft tissue space through which the tendons pass. Zone 3 extends from the distal edge of the carpal tunnel to the A1 pulley, and the lumbrical muscles lie in this zone.
Zone 4 includes the carpal tunnel from its proximal to distal boundaries, and zone 5 is from the tendon origins in the distal forearm and wrist until they pass into the carpal tunnel.
The dorsal extensor tendon to each finger is significantly smaller in size than the corresponding flexor tendon (Fig. 4.6). Only the central slip inserts on the base of the middle phalanx, while the two lateral bands pass on either side of the central slip and insert onto the base of the distal phalanx. In the index and little fingers, there are also contributions to the extensor tendon by the extensor indicis proprius and extensor digiti minimi tendons as well.
In the thumb, there are corresponding dorsal and volar tendons that perform extension and flexion. The single long tendon arising above the level of the wrist on the volar side is the flexor pollicis longus (FPL) tendon, which passes within the thenar eminence between the two heads of the flexor pollicis brevis muscle, and inserts into the volar aspect of the base of the distal phalanx (Fig. 4.7).
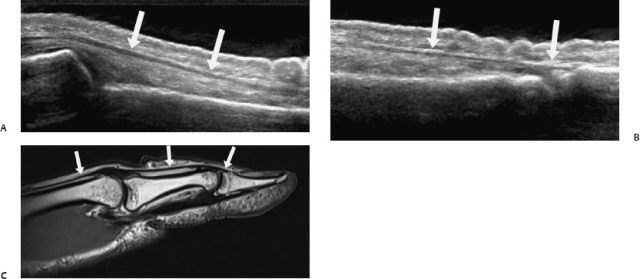
Fig. 4.6 Longitudinal ultrasound (A,B) images and corresponding magnetic resonance (C) image of the normal extensor tendon (white arrows) to its distal insertion on the distal phalanx.
The three long tendons on the dorsal aspect of the thumb (from radial to ulnar at the level of the wrist) are the abductor pollicis longus (APL), extensor pollicis brevis (EPB), and extensor pollicis longus (EPL) tendons. The APL and EPB lie within the first dorsal compartment at the wrist, pass over a groove on the radial styloid process, and insert on to the base of the first metacarpal (APL) and base of the proximal phalanx (EPB) (Fig. 4.8A). These two tendons form the radial margin of the anatomic snuff box at the dorsum of the hand.
The extensor pollicis longus tendon lies in the third dorsal compartment of the wrist (Fig. 4.8B). As it passes distally, it hooks around the Lister tubercle on the dorsal surface of the distal radius, runs superficial to the extensor carpi radialis longus and extensor carpi radialis brevis tendons in the second dorsal compartment. It provides the ulnar margin for the anatomic snuff box, and inserts onto the base of the distal phalanx of the thumb.
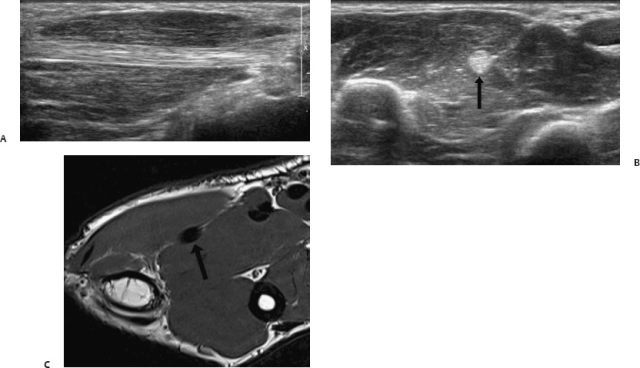
Fig. 4.7 Longitudinal (A) and transverse (B) ultrasound images and magnetic resonance (C) image of the flexor pollicis tendon (black arrow) in the thenar eminence.
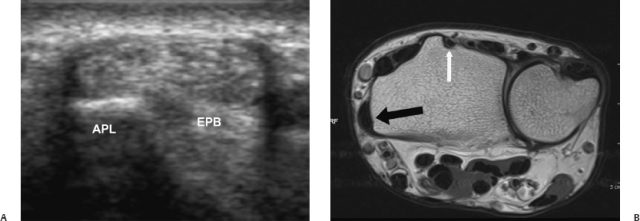
Fig. 4.8 Transver se ultrasound image (A) of the first dorsal compartment at the wrist containing the abductor pollicis longus (APL) and extensor pollicis brevis (EPB) tendons. Corresponding magnetic resonance image (B) shows these two tendons in the first dorsal compartment (thick black arrow) as well as the extensor pollicis longus (EPL) in the third dorsal compartment (thin white arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





