 Technical Guidelines and Normal Anatomy
Technical Guidelines and Normal Anatomy
Ultrasound of the knee requires a high-frequency linear array transducer. The knee can conveniently be considered as having four separate quadrants: anterior, posterior, lateral, and medial. Ultrasound examinations are usually targeted and directed at one or two quadrants to answer specific clinical questions. It is unusual to perform an examination that looks at all four quadrants.
The anterior knee structures include, from superior to inferior, the quadriceps muscle, quadriceps tendon, patella, and patellar tendon (Fig. 5.1). The suprapatellar recess lies deep to the quadriceps tendon and patella and the infrapatellar fat deep to the patellar tendon. Examination of the anterior knee is performed with the patient supine. The hip should be extended. The knee should be slightly flexed. This is best achieved and most comfortable for the patient if a small pad or roll of paper towels is placed under the knee.
The deepest of the quadriceps muscles is the vastus intermedius muscle (Fig. 5.2). It lies in the midline immediately anterior to the femur. The rectus femoris muscle is midline and is superficial to vastus intermedius. The vastus medialis and vastus lateralis muscles are also superficial to vastus intermedius and lie on the medial and lateral aspects, respectively, of the rectus femoris muscle. Distally, the quadriceps muscles narrow, form tendons, and contribute to the quadriceps tendon. The rectus femoris tendon forms relatively proximally followed by the vastus intermedius tendon whereas the vastus medialis and vastus lateralis muscles extend more distally before forming their tendons, which run obliquely. The quadriceps tendon inserts into the upper pole of the patella. The patella has an echogenic, slightly convex anterior surface. Variable, frequently negligible, amounts of tendon run superficial to the patella in continuity with the quadriceps and patellar tendons. The retinacula are thin and hypoechoic and run medially and laterally from the patella on transverse images.
The patellar tendon extends from the lower pole of the patella to the tibial tuberosity (Fig. 5.1). The patellar tendon has a generally uniform caliber and texture, but the ends are slightly expanded and tendon narrows at the medial and lateral margins, which are convex (Fig. 5.3). The ends of the patellar tendon may appear slightly hypoechoic on long axis scans due to anisotropy, but this can be corrected by altering the angulation of the transducer or by beam-steering and confirmed by performing short axis scans. The normal patellar tendon is 10 to 15 mm wide and 3 to 6 mm deep.
The suprapatellar recess extends proximal to the patella and is deep to the quadriceps tendon (Fig. 5.1). The normal recess is dry or contains a small amount of fluid. A dry recess appears as a thin echogenic line.
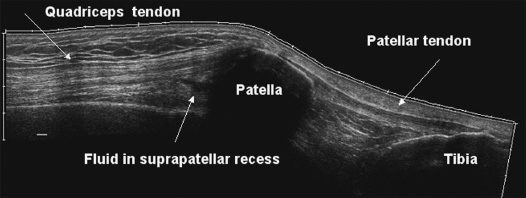
Fig. 5.1 Extended field of view long axis ultrasound scan of extensor mechanism.
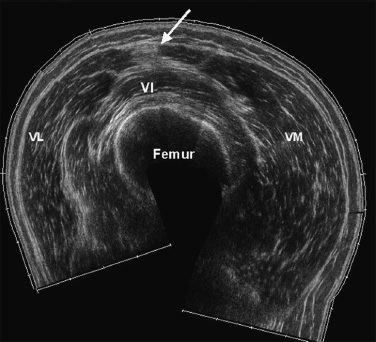
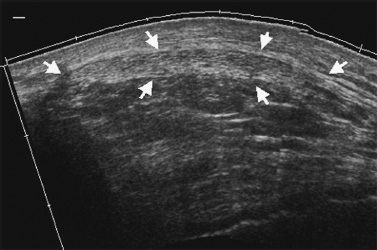
Fig. 5.3 Transverse ultrasound scan of patellar tendon (arrows). The tendon is echogenic and is uniform in texture and size. It tapers at the edges.
The infrapatellar fat lies deep to the patellar tendon and has a heterogeneous appearance, although fluid-filled cysts or bursae may be present.
If the knee is fully flexed the patellar sulcus or trochlea can be examined. The articular cartilage is thick and hypoechoic and immediately superficial to the cortical bone (Fig. 5.4).
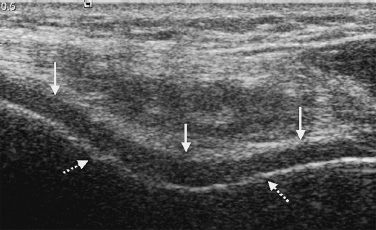
Fig. 5.4 Transverse ultrasound scan of patellar sulcus of distal femur with knee flexed. The hypoechoic articular cartilage (solid arrows) is superficial to the cortex of the femur (broken arrows).
The posterior knee and popliteal fossa are examined with the patient prone. The knee should be minimally flexed or extended. The gastrocnemius muscle has separate heads that originate from the medial and lateral femoral epicondyles. The popliteal neurovascular bundle lies between the medial and lateral heads of gastrocnemius. The popliteal artery is the deepest structure. The popliteal vein lies between the popliteal artery and the more superficial tibial nerve. The common peroneal nerve comes off the tibial nerve and extends distally on the lateral border of the lateral head of gastrocnemius, to run laterally around the neck of the fibula. On the other side of the posterior knee, the semimembranosus and semitendinosus tendons lie on the medial aspect of the medial head of gastrocnemius (Fig. 5.5). Semitendinosus is superficial to semimembranosus. Both tendons appear hypoechoic if the transducer is not perpendicular to the tendons and may be mistaken for cysts. Altering transducer angulation or employing beam-steering will correct this artifact.
The medial knee is examined with the patient supine, the hip extended, the knee extended or slightly flexed and the leg slightly externally rotated. The medial collateral ligament runs between the medial femoral epicondyle and the medial surface of the proximal tibia and has uniform texture (Fig. 5.6). The distal ligament is slightly expanded. A small bursa is sometimes seen between the deep and superficial layers of the ligament. The medial meniscus lies immediately deep to the medial collateral ligament. The pes anserinus tendons, from anterior to posterior, sartorius, gracilis, and semitendinosus lay posteromedial to the medial collateral ligament and insert on the proximal tibia.
The lateral structures are examined with the patient supine, the hip extended, the knee slightly flexed, and the leg slightly internally rotated. The most anterior structure is the iliotibial band, which inserts on the Gerdy tubercle on the anterolateral aspect of the proximal tibia. The lateral collateral ligament lies posteriorly and runs obliquely from the lateral femoral epicondyle to the fibular head. It forms a conjoined tendon with biceps femoris, which has a more vertical orientation and is the most posterior of the lateral structures.
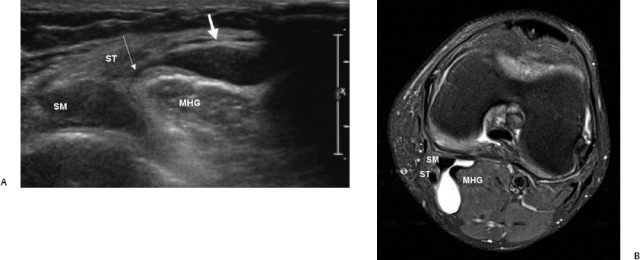
Fig. 5.5 (A) Transverse ultrasound scan of popliteal fossa showing small, anechoic Baker cyst (wide arrow). Its narrow stalk (narrow arrow) emerges between the medial head of gastrocnemius (MHG) and the semimembranosus (SM) and semitendinosus (ST) tendons. The tendons are hypoechoic due to anisotropy. (B) Axial fat-saturated proton-density-weighted magnetic resonance image showing small Baker cyst. Its stalk lies between the medial head of gastrocnemius (MHG) and the semimembranosus (SM) and semitendinosus (ST) tendons.
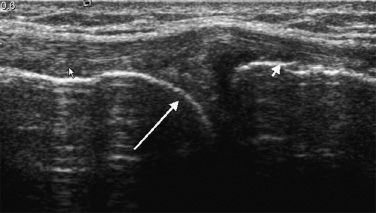
Fig. 5.6 Long axis ultrasound scan of medial collateral ligament (short arrows). The triangular, echogenic medial meniscus (long arrow) lies immediately deep to the ligament.
 Pathologies
Pathologies
Anterior Knee
Tears of Quadriceps and Patellar Tendons and Quadriceps Muscle
Quadriceps tendon tears are relatively uncommon. They are caused by a sudden contraction of the extensor mechanism. Most patients are middle-aged or older. Systemic diseases such as chronic renal failure, gout, systemic lupus erythematosus, diabetes mellitus, rheumatoid arthritis, and hyperparathyroidism may predispose to quadriceps tears. The patient typically presents with swelling and an inability to extend the knee following injury. The diagnosis of a quadriceps muscle or tendon tear is usually clinically obvious, particularly if there is a palpable defect in the quadriceps muscle (Fig. 5.7), but a tense joint effusion or a prepatellar hematoma without tendon damage may have a similar clinical presentation. Straight leg raising may be possible with partial tears.
Quadriceps tears are usually incomplete and mostly affect the rectus femoris component of the tendon. Tears occur either in the distal 1 to 2 cm of the tendon or at its insertion into the patella. Ultrasound examination identifies a gap in the tendon fibers. The gap is more conspicuous when filled by hematoma, which is hypoechoic. The blood may extend between layers of muscle and tendon and also into subcutaneous tissues. Retraction of the proximal edge of the tendon may be made more obvious by passively flexing the knee.
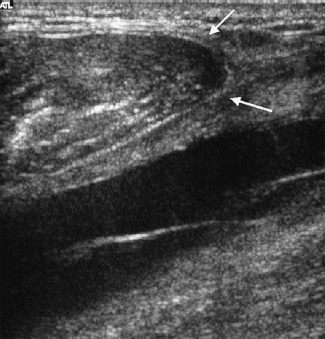
Fig. 5.7 Long axis ultrasound scan of complete tear of rectus femoris muscle. It has a convex inferior margin (arrows). There is a large anechoic hematoma deep to the tear.
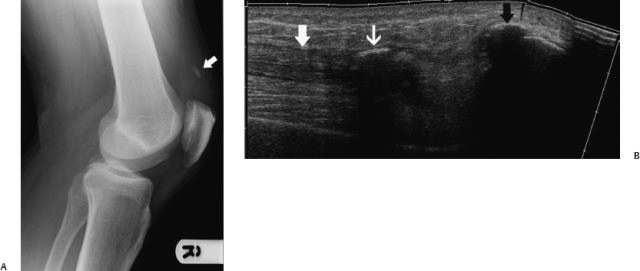
Fig. 5.8 (A) Lateral radiograph of knee showing avulsed proximal pole of patella (arrow). (B) Extended field of view ultrasound scan showing that the quadriceps tendon (broad white arrow) is still attached to the avulsed proximal pole of patella (narrow white arrow). There is hematoma in the gap between the avulsed fragment and the patella (black arrow).
The distal quadriceps tendon is also involved in complete tears. The tear involves all layers of the tendon. The torn tendon edges are swollen and irregular and the gap is occupied by hypoechoic hematoma that may extend into surrounding soft tissues. Traction on the patella helps to improve conspicuity of the tendon defect and to differentiate complete from incomplete tears. Occasionally, the proximal pole of the patella is avulsed with the tendon still attached (Fig. 5.8).
The sensitivity of ultrasound is 100% for partial and complete quadriceps tendon tears and the specificity is 100% for complete tears. Ultrasound is therefore an excellent way to confirm the diagnosis.
Rupture of the patellar tendon involves the proximal tendon. Patellar tendon tears are less frequent than quadriceps tears. They usually occur in younger patients due to sporting injuries, although preexisting tendinosis may be present. Patients present with pain, swelling, and an inability to extend the knee. Proximal retraction of the patella may be obvious on radiographs. Ultrasound shows a defect in the tendon that is occupied by hypoechoic hematoma (Fig. 5.9). The distal patellar tendon may have an irregular, redundant appearance. Flexing the knee may make the tear more obvious.
Sometimes, patients present with a clinically obvious tear of the extensor mechanism,but the clinician is uncertain of the level of the tear or if it is complete or incomplete. Ultrasound is an accurate method of confirming the diagnosis, the extent of damage, and the precise site of the tendon injury. It helps to mark the skin at the site of the tear.
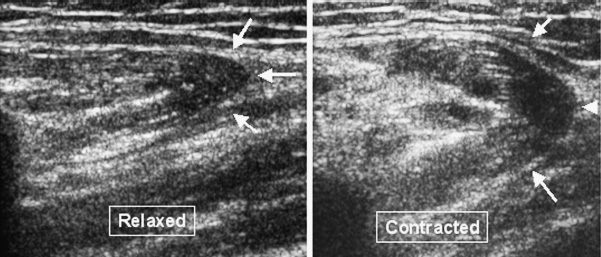
Tears of the quadriceps muscles are usually diagnosed clinically at the time of injury and heal spontaneously. Occasionally, patients present with an apparent mass lesion in the anterior thigh due to an unrecognized, chronic quadriceps muscle tear, usually of rectus femoris. The typical presentation is of an anterior thigh mass that enlarges when the quadriceps muscle is contracted. A mass can be palpated and there may be a focal depression distal to the mass. Long axis ultrasound examination shows that the proximal edge of the torn muscle has a convex inferior margin (Fig. 5.10). The fibroadipose septae may converge or lie parallel to the tear margin. As the muscle contracts the convex margin, and with it the fibroadipose septae, becomes rounder and retracts making the apparent mass more prominent. On short axis scans, a tear can be recognized because the muscle suddenly disappears instead of incrementally becoming smaller (Fig. 5.11). Patients are frequently concerned that the mass is a tumor. They readily understand the real nature of the mass and are reassured when the ultrasound appearances are explained. It is particularly helpful to demonstrate the changes during contraction and relaxation of the muscle.
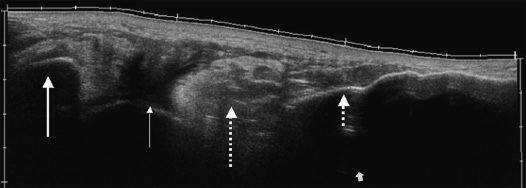
Fig. 5.9 Long axis ultrasound scan of complete midsubstance tear of patellar tendon. Residual tendon is attached to the patella (large solid arrow) and the tibial tuberosity (small broken arrow). The gap is occupied by liquid hematoma (small solid arrow) and echogenic thrombus (large broken arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






