The most common indication for pediatric cervical spine (C-spine) imaging is trauma. Although cervical spinal injuries are rare in children, the result can be devastating. The role of the radiologist is crucial in the early detection of cervical spinal injury (CSI) that may require immediate clinical attention. Imaging interpretation of the C-spine is particularly challenging and requires a thorough knowledge of its unique anatomic characteristics as the spine continues to develop and mature during childhood, reaching adult features at approximately 12 years of age. Knowledge of developmental changes allows differentiation of normal age-related anatomy from traumatic injury. Pediatric CSI results in extensive variability of injury patterns, closely related to age and mechanism of trauma. This chapter includes a review of the normal C-spine anatomy and common variants, a systematic approach for radiological interpretation, and illustrations of the most common traumatic injuries of the pediatric C-spine. The concept of “clearance” of the pediatric C-spine in the emergency department setting will also be discussed.
Epidemiology
Trauma leads as the most common cause of pediatric morbidity and mortality. Spinal injury occurs in 5% of trauma cases, and the region most frequently affected in children is the C-spine (60%–80% of cases). The incidence rate of CSI in pediatric blunt trauma is 1% to 1.5%, occurring more often in boys. CSI tends to increase with age and peaks at 9 to 12 years of age. Although CSI is rare, it can result in devastating outcomes, such as significant neurological injury or even death. The anatomy and biomechanics of the immature pediatric spine predispose to specific patterns of injury that are different from the adult spine. A study recently published by evaluated a large, multicenter cohort of patients, including from 17 PECARN (Pediatric Emergency Care Applied Research Network) sites. This study retrospectively classified CSI in 540 patients and demonstrated that patterns of CSI with blunt trauma are closely related to age and mechanism of trauma , as has been also supported by other publications.
Mechanism of Trauma
Assessment by age subgroups shows that motor vehicle collision (MVC) and falls are the most common mechanisms of injury in both the youngest children (<2 years of age) and children aged 2 to 7 years. Pedestrian struck by motor vehicle is also a common mechanism in children aged 2 to 7 years. In the group ≥8 years of age, sports injuries and MVC are more frequent. CSI related to sports accounts for a quarter of ER visits of children. A multicenter retrospective case control study in children younger than 16 by showed that football was the sport most frequently related to CSI, as well as diving, gymnastics/cheer, and hockey. CSI was also prevalent in unorganized activities such as trampolining, rough play or falls.
Patterns of Cervical Spinal Injury
Patterns of CSI are closely related to age and mechanism of trauma. Injuries from the atlantooccipital articulation to the C2 level, known as axial injuries , are more often seen in children ≤3 years of age. Factors that contribute to this pattern of injury include a large head relative to the C-spine with a fulcrum of motion at the C2/C3 level, underdeveloped neck musculature, lax ligamentous structures, vertebral body morphology, and the presence of vertebral synchondroses. Axial injuries include C1 and C2 fractures, as well as atlantooccipital dislocation (AOD) and atlantoaxial rotary subluxation (AARS). Increased morbidity and mortality is seen with AOD and may result in death. Cord injury is also more common in the young age group and can lead to severe neurological deficits. In children younger than 8 years, the bony spinal column allows significant stretching without tearing, while the spinal cord is much less stretchable and can result in shear injury.
Subaxial injuries , from the level of C3 to C7, occur more often in children older than 8 years and can frequently present with ligamentous injury and/or vertebral body fractures. At this age the fulcrum of motion is at the C5/C6 level, the neck muscles are more developed, and most of the vertebral synchondroses are fused. CSI in the teenager is similar to the adult.
Multilevel injuries are extremely rare in pediatric CSI. Injury to other organ systems is common in high-energy trauma and contributes to unfavorable outcome. Head trauma is the most common associated injury.
SCIWORA (spinal cord injury without radiographic abnormality) is a term that was first used by to describe radiographically normal cases in patients with neurological abnormality. Historically, this term refers to spinal cord injury in the absence of findings on plain radiographs. However, with the advent of new imaging modalities to evaluate the spine, such as computed tomography (CT) and magnetic resonance imaging (MRI), this term has become confusing over time. Several authors have recently proposed the redefinition of this term, suggesting that “real-SCIWORA” should refer only to spinal cord injury with negative neuroimaging findings on all modalities, including plain radiographs, CT, and MRI. The incidence rate of SCIWORA in pediatric CSI ranges from 5% to 67%; this wide range may be in part related to differences in the use of this term among clinicians. The lack of MRI studies at the time of diagnosis may result in higher reports of SCIWORA by pediatricians and emergency department physicians, although it is often used less by neurosurgeons and orthopedic surgeons, who usually have magnetic resonance (MR) studies available at the time of diagnosis.
Cervical Spine Developmental Anatomy and Normal Variants
The radiologist must be aware of the normal developmental changes and anatomic variants of the pediatric C-spine on radiological studies to detect pathology and avoid misinterpretation. These include changes in vertebral morphology during the first decade of life, as well as the presence of synchondroses, apophyses, and secondary centers of ossification. Pitfalls may result from technically inadequate plain radiographs related to head positioning.
Vertebral Body Shape Developmental Changes
The shape of the vertebral bodies changes from birth until approximately the first decade of life. In infants, cervical vertebral bodies are oval shaped, whereas at around age 2 to 3 years, these appear relatively flattened. From 3 to 8 years of age, vertebral bodies demonstrate mild anterior wedging, especially C3 through C5, and should not be mistaken for compression fractures. At about 10 years of age, the cervical vertebrae acquire a more rectangular or square shape, similar to the adult spine. Other unique findings in the young child include shallow articular joints with slightly uncovered appearance of the facets and underdeveloped spinous processes with mild upward orientation ( Figs. 28.1 and 28.2 ). Uncovertebral joints form during adolescence (see Fig. 28.2 ).


Ossification Patterns of the Cervical Spine Vertebrae
C1 (Atlas)
C1 is formed from three primary ossification centers ( Box 28.1 ): the anterior arch and two neural (posterior) arches ( Fig. 28.3 ). C1 is a ring structure and does not have a body. The anterior arch is mainly cartilaginous at birth, but some degree of ossification may be present in 20% of newborns. Otherwise, ossification of the anterior arch is expected to be visible at around 12 months of age but can be delayed until 24 months of age. The C1 anterior arch can also form from multiple ossification centers (2–4) in 25% of children. The most common variant is two ossification centers in 18% of the population ( Fig. 28.4 ). Occasionally the anterior arch can be absent, and the neural arches may fuse anteriorly.
C1
Anterior Arch
Ossification: present at birth (20%), visible by 12 months
Fusion: 6–8 years
Posterior Arch
Ossification: begins at seventh week of fetal life
Fusion: 3–5 years
C2
Body, Neural Arches, and Odontoid
Ossification: present at birth
Fusion
Odontocentral synchondrosis: begins at 3–6 years, complete by 11–12 years
Odontoneural and neurocentral synchondroses: 3–6 years
Posterior arches: 2–3 years
Os Terminale
Ossification: appears by 3–6 years
Fusion: 10–12 years
C3–C7
Body and Neural Arches
Ossification: present at birth
Fusion: neurocentral synchondroses: 2–3 years
Posterior arches: 3–6 years


The posterior arches begin to ossify in the seventh week of fetal life. The neurocentral synchondroses are between the anterior arch and posterior arches (see Fig. 28.3 ). A completely ossified anterior arch with fused neurocentral synchondroses usually occurs by 6 to 8 years of age. The posterior arches usually fuse by 3 to 5 years of age (see Fig. 28.3 ). Although rare, incomplete fusion of the posterior arches or a midline cleft may be seen in children ≤8 years of age. Another anatomic variant includes unilateral or bilateral paramedian clefts (see Fig. 28.4C ).
C2 (Axis)
C2 is formed by four primary ossification centers that are present at birth: the body, two neural arches, and the odontoid process ( Fig. 28.5 ). A single secondary ossification center, the os terminale (tip of the odontoid process), appears between 3 and 6 years of age (see Fig. 28.5C ). C2 synchondroses can be seen until approximately 8 years of age and should not be mistaken for fractures. The subdental (odontocentral) synchondrosis ( Figs. 28.6 and 28.7 ), located between the odontoid process and the body, begins to close around age 3 to 6 years of age and usually fuses around 11 to 12 years of age. Bilateral neurocentral synchondroses separate the body from each neural arch, while bilateral odontoneural synchondroses separate the odontoid process from each neural arch; these fuse between 3 and 6 years of age (see Figs. 28.6 and 28.7 ). The tip of the odontoid process (os terminale) fuses at approximately 12 years of age. Because the odontoid process forms from two ossification centers in utero, a vertical remnant synchondrosis can occasionally be seen. The posterior arches fuse around 2 to 3 years of age.



C3–C7 Vertebrae
C3–C7 vertebrae each form from three ossification centers: the body and two neural arches. The neural arches fuse posteriorly at around 2 to 3 years of age, while the body and neural arches fuse between 3 and 6 years of age. C7 has the longest spinous process and C3 to C7 commonly have bifid spinous processes ( Fig. 28.8 ).

Secondary ossification centers of C3–C7 include ring and spinous process apophyses. A ring apophysis is a wedge-shaped ossification center along the anterior and inferior aspect of the vertebral body and may be present at multiple levels. Ring apophyses ossify around 10 years of age and fuse between 18 and 25 years of age. The apophysis of the tip of the spinous process is seen more often at the C6 and C7 levels ( Fig. 28.9 ).

Craniocervical Junction and Ligaments
The craniocervical junction (CCJ) is composed of the atlantooccipital and atlantoaxial joints, which are responsible for preserving stability, mobility, and rotation of the CCJ. The atlantooccipital joint allows for flexion and extension (F/E) movements and mainly depends on bony structures (the occipital condyles over the C1 sockets). The atlantoaxial joint allows for rotational movements and mostly depends on ligamentous structures. The major ligaments of the CCJ include the transverse ligament (major component of the cruciate ligament), alar ligaments, apical ligament, tectorial membrane (continuation of the posterior longitudinal ligament), anterior atlantooccipital (AAO) membrane and atlantoaxial ligament (continuation of the anterior longitudinal ligament), and posterior atlantooccipital (PAO) membrane (continuation of the ligamentum flavum) ( Fig. 28.10 ).

Additional ligamentous complex of the posterior C-spine includes the ligamentum flavum and interspinous ligaments (continues cephalad as the ligamentum nuchae).
Transverse Ligament
The transverse ligament is the thickest and strongest of the CCJ and is a major component of the cruciform ligament, serving as the major stabilizing ligament of the atlantoaxial joint ( Fig. 28.11 ). The superior and inferior limbs of the cruciform ligament are small and do not provide significant CCJ stability. The transverse ligament courses posterior to the odontoid process of C2 and attaches to each lateral tubercle of C1, keeping the odontoid process anteriorly against the posterior aspect of the anterior C1 arch. The spinal cord is located posterior to this ligament. The transverse ligament allows for atlantoaxial rotation up to approximately 47 degrees, whereas the alar ligaments limit excessive rotation. Rupture of the transverse ligament results in C1/C2 subluxation.

Alar Ligament
The alar ligament attaches to the odontoid process and skull base. This ligament limits excessive rotation and lateral bending of the neck. It also stabilizes the atlantoaxial joint, preventing C1/C2 subluxation. The alar ligament may have a cranial caudal or horizontal orientation, and its shape is variable: tubular, round, elliptical, rectangular, or wing-shaped.
Apical Ligament
The apical ligament attaches to the tip of the odontoid process and basion and courses posterior to the alar ligament. Some have suggested the lack of function of this ligament. A study in cadavers demonstrated the absence of the apical ligament in 20% of specimens.
Tectorial Membrane
The tectorial membrane is a thin structure, formed by two to three layers that fuse at the posterior longitudinal ligament, and courses posterior to the cruciform ligament. The middle and thickest layer attaches from the clivus to the body of C2 ( Fig. 28.11 ). Nerves and vessels are present between its layers. The tectorial membrane’s function is controversial; some suggest it restricts flexion, whereas others consider it a CCJ stabilizer that resists extension.
Anterior Atlantooccipital Membranes
The AAO membrane is a continuation of the anterior longitudinal ligament and attaches to the anterior aspect of C1 and to the anterior rim of the foramen magnum ( Fig. 28.10 ). This membrane courses posterior to the prevertebral neck muscles. The AAO membrane forms the anterior wall of the supraodontoid space, which contains fat and veins and the alar, apical, and Barkow ligaments.
Posterior Atlantooccipital Membrane
The PAO membrane attaches to the C1 posterior arch and to the posterior rim of the foramen magnum. The AAO and PAO membranes are considered stabilizers of the CCJ.
Clearance of the Cervical Spine
Suspected CSI in the setting of blunt trauma requires proper clinical evaluation in order to provide adequate management and prevent catastrophic outcomes such as death, quadriplegia or other serious neurologic sequelae. The purpose of a pediatric cervical spine protocol is to detect clinically significant CSI in children who have sustained blunt trauma, to identify all significant injuries, to decrease unnecessary radiation exposure, and permit the removal of a rigid cervical collar that is no longer necessary. Pediatric clearance of the C-spine is the process to evaluate clinically a child with suspected CSI (history and physical examination), who may require diagnostic imaging evaluation, in order to determine that CSI has not occurred. The clinical history should also include the mechanism of injury such as diving, axial load, “clothes-lining”, or a high-risk motor vehicle collision. Cervical spine clearance is the responsibility of physicians with expertise in evaluating a child with suspected CSI; this includes ED physicians, general and trauma surgeons, neurosurgeons, and orthopedic surgeons. Less than 50% of level-I pediatric trauma centers, until recently, had a written protocol for c-spine clearance. The Pediatric Cervical Spine Clearance Working Group (PCSCWG), a subgroup of the Pediatric Cervical Spine Study Group, recognized the need for a consensus on comprehensive standardized guidelines for pediatric c-spine clearance. This multidisciplinary group of experts in pediatric c-spine clearance just recently developed an algorithm to guide institutional protocols for c-spine clearance ( ). By consensus, this group created three pathways according to the Glasgow Coma Scale (GCS) score and its pediatric modification. Pathway 1: patient with a GCS score of 14 or 15; pathway 2: patient with a GSC score of ≤8, and pathway 3: patient with a GCS of 9 to 13. These pathways determine the imaging modality indicated. Most children that undergo blunt trauma have a GSC score of 14 or 15. If the children in this group cannot be cleared clinically, conventional radiography is the next step recommended, which consists of a high-quality lateral radiograph. CT is indicated in children who have suffered blunt trauma and have a GCS score of ≤8. MRI is an excellent modality in all age groups, and indicated for the evaluation of CSI in the obtunded child when rapid neurologic recovery is not expected. Patients with GCS score of 9-13 require spinal immobilization and radiographic imaging. In this group, CT is done when radiographs are abnormal, or if an abnormal physical finding is detected. Children with congenital vertebral anomalies such as Klippel-Feil syndrome, spinal canal stenosis as seen in achondroplasia, os odontoideum and atlanto-axial instability in children with Down syndrome, are at increased risk for CSI. Further evaluation with CT or MRI is usually indicated in children with predisposing conditions ( Box 28.2 ).
Three pathways:
- •
Pathway 1: patient with a ∗
∗ GCS = Glasgow Coma Scale
GCS score of 14 or 15
- •
Pathway 2: patient with a GCS score of ≤ 8
- •
Pathway 3: patient with a GCS score of 9-13
Children with congenital vertebral anomalies, such as Klippel-Feil syndrome (KFS), spinal canal stenosis as seen in achondroplasia, os odontoideum, and atlantoaxial instability (AAI) in children with Down syndrome, are at increased risk for CSI. Further evaluation with CT or MRI is indicated in patients with these predisposing conditions.
Clinical Presentation of CSI
Symptoms of CSI may include localized neck tenderness, muscle spasm, decreased range of neck motion, and torticollis. Spinal cord injury may manifest as sensory loss (paresthesias, dysesthesias, etc.) or motor loss (weakness), or even respiratory arrest when injury occurs at the C5 level or higher.
Diagnostic Imaging of CSI
The choice of imaging modality for evaluation of CSI depends on the patient’s clinical status. Reducing radiation exposure in children should always be considered as well, given the potential risk for radiation-induced cancer, particularly thyroid cancer when imaging the C-spine. For instance, the estimated amount of ionizing radiation exposure is 30-fold higher for C-spine CT (approximate radiation dose: 6 mSv) versus plain radiography (approximate radiation dose: 0.2 mSv). The role and indication of plain radiographs, CT, and/or MRI in pediatric CSI will be subsequently reviewed.
Plain Radiography
Plain radiographs have high sensitivity in suspected pediatric CSI and are accepted as the imaging modality of choice in the initial evaluation of a child with a history of blunt trauma. For example, reported a sensitivity of 90% (95% confidence interval [CI], 85%–94%) when using two or more radiographic views to detect CSI. In this study, radiographs in children with normal neurological examinations missed a small number of injuries; however, none required neurosurgical intervention. Furthermore, the Appropriateness Criteria of the American College of Radiology indicate radiography as the imaging method of choice for children younger than 16 years for evaluation of suspected CSI.
In the alert patient ≥5 years of age, with normal neurological examination, a three-view C-spine series (lateral, anteroposterior [AP] and open-mouth odontoid views) is recommended. In children younger than 5 years, only the lateral and AP views are done. The odontoid view is not indicated in this age group because of its technical difficulty and low yield. The lateral view is always obtained first while the patient is wearing a cervical collar. It is important to identify children at risk for CSI that will need further evaluation with CT and/or MRI to avoid missing clinically important injuries. In the critical patient a cross-table lateral film is done initially.
Flexion and Extension Lateral Views
F/E lateral views are not performed to clear the C-spine in the acute setting in children. These views are usually done on a follow-up visit in patients who report persistent cervical tenderness and have negative plain films or CT. F/E views are useful in detecting vertebral subluxation, which can be seen with ligamentous injury. Technically adequate F/E views are defined as 30 degrees of change from neutral position and should include the C7-T1 junction. F/E views are accepted as standard for evaluation of ligamentous injury.
Normal Parameters of C-Spine Radiographs
Lateral Radiograph
A technically adequate lateral radiograph includes the skull base through the C7-T1 disk space and should be obtained in neutral position. Loss of the cervical lordosis (straightening of the C-spine) is often a normal finding in children, usually as a result of mild head flexion. It is frequently seen in the child wearing a cervical collar or may be occasionally caused by muscle spasm.
Appropriate vertebral alignment should be assessed on the lateral radiograph ( Fig. 28.12 ). Three curved lines demonstrate the alignment of the vertebral bodies and the spinal canal. Disruption of these lines may indicate subluxation in the presence of ligamentous injury or displaced fracture fragments. A fourth line can be drawn at the tips of the spinous process to also highlight any offset. The C1–C2 interspinous distance (measured from the inferior aspect of the C1 spinous process to the superior aspect of the C2 spinous process) should measure less than 12 mm. Increased interspinous distance suggests possible posterior ligamentous injury.
- 1.
Anterior vertebral line: Demarcates the anterior margin of the vertebral bodies.
- 2.
Posterior vertebral line: Demarcates the posterior margin of the vertebral bodies.
- 3.
Spinolaminar or posterior cervical line (Swischuk line): This line demarcates the posterior margin of the spinal canal. The posterior cervical line is measured from the anterior aspect of the spinous process of C1 to the anterior aspect of the spinous process of C3. This line should overlap the anterior aspect of the spinous process of C2 or measure less than 2 mm from it ( Fig. 28.13A ). A distance of greater than 2 mm indicates true subluxation (see Fig. 28.13B ).

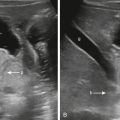
Fig. 28.13
Posterior cervical (Swischuk) or spinolaminar line.
This line is useful to differentiate pseudosubluxation from true subluxation. Lateral radiographs show the posterior cervical line measured from the anterior aspect of the C1 spinous process to the anterior aspect of the C3 spinous process (A, yellow line ; B, orange line ). This line should overlap the anterior aspect of the spinous process of C2 or measure <2 mm from it. (A) There is minimal anterolisthesis of C2 on C3 ( light blue line ) with a normal posterior cervical line ( yellow line ), consistent with pseudosubluxation. (B) The posterior cervical line ( orange line ) shows a distance ≥2 mm to the sclerotic spinous process of C2, consistent with true subluxation in this child with a C2 fracture.
- 4.
Posterior spinous line: Follows the tip of the spinous processes.