 Clinical Indications
Clinical Indications
 Inflammatory and degenerative diseases—De Quervain disease, distal intersection syndrome, tenosynovitis, Inflammatory arthritis (rheumatoid arthritis [RA], crystal-related arthritis)
Inflammatory and degenerative diseases—De Quervain disease, distal intersection syndrome, tenosynovitis, Inflammatory arthritis (rheumatoid arthritis [RA], crystal-related arthritis)
 Traumatic lesions of extensor and flexor tendons, nerves, vessels, and occult fractures of the carpal bones
Traumatic lesions of extensor and flexor tendons, nerves, vessels, and occult fractures of the carpal bones
 Entrapment neuropathies—tunnel syndromes (carpal and Guyon)
Entrapment neuropathies—tunnel syndromes (carpal and Guyon)
 Space-occupying lesions—dorsal or ventral ganglia, neurogenic tumors, lipomatous tumors, presence of accessory muscles
Space-occupying lesions—dorsal or ventral ganglia, neurogenic tumors, lipomatous tumors, presence of accessory muscles
 Technical Guidelines
Technical Guidelines
For an ultrasound of the wrist, the patient rests the wrist in his or her lap and is seated in front of the examiner. Alternatively, the patient may be seated at an examination table with both hands resting on the table. The screening on ultrasound examination includes transverse and longitudinal views of the local structures at rest or after dynamic testing positions. In addition, oblique approaches or a heel-toe maneuver (to increase the pressure on one side of the probe) can be helpful to remove anisotropy artifacts. For the examination of the volar aspect of the wrist, the hand is positioned palm up with mild extension and radial or ulnar deviation; for examination of the dorsal aspect of the wrist, the hands are moved into a palm down position. Maneuvers of gentle flexion and/or extension of the digits can help identify the different tendons. These flexo-extension maneuvers are performed along a longitudinal sonographic axis; this dynamic study shows the normal and gentle movement of the tendons and can be helpful in the detection of tendon entrapments or for the identification of the median nerve inside the carpal tunnel that does not show any movement.
 Normal Anatomy
Normal Anatomy
The wrist can be subdivided into four segments: the volar, dorsal, medial, and lateral aspects (Figs. 3.1 and 3.2).
The volar aspect comprises a roof made by the flexor retinaculum, which is a fibrous band best identified on transverse view as a hyperechoic band. Deeper in this aspect is the carpal tunnel that contains the superficial and deep hand flexor tendons (flexor digitorum superficialis and profundus of the second to fifth finger) and their surrounding single synovial sheath, as well as the flexor pollicis longus tendon surrounded by its sheath. On ultrasound, all these tendinous structures show a hyperechoic fibrillar pattern. Above the flexor tendons and below the flexor retinaculum is the median nerve. The median nerve, a hyperechoic structure that contains small hypoechoic dots representing the neuronal fascicles; these are best shown on transverse ultrasound view. The bone margins of the tunnel, going from lateral to medial and proximal to distal are the scaphoid tubercle and pisiform bone and more distally, the ridge of the trapezium and the hook of the hamate; all these bone margins are hyperechoic. Outside the carpal tunnel are the tendons for the flexor carpi radialis, flexor carpi ulnaris and the palmaris longus. The palmaris longus tendon may be absent in up to 16% of the population as a normal variant. It may also vary in shape presenting different types of muscular and tendinous components as anatomic variants.
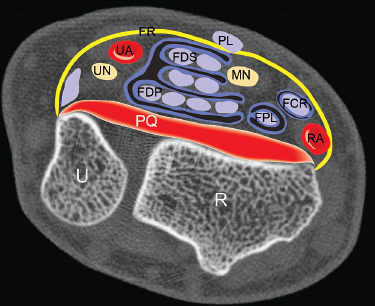
Fig. 3.1 Volar aspect of the wrist, axial ultrasound view. FR, flexor retinaculum; FDS, flexor digitorum superficialis tendons; FDP, flexor digitorum profundus tendons; MN, median nerve; UN, ulnar nerve; FCR, flexor carpi radialis tendon; FPL, flexor pollicis longus tendon; RA, radial artery; UA, ulnar artery; PQ, pronator quadratus muscle; R, radius; U, ulna; PL, palmaris longus tendon; R, radius; U, ulna.
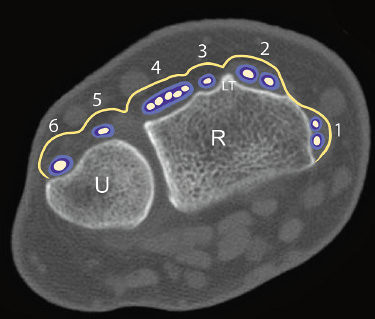
Fig. 3.2 Dorsal aspect of the wrist, axial ultrasound view. Extensor tendons compartments of the wrist (1 through 6, from lateral to medial): (1) abductor pollicis longus and extensor pollicis brevis tendons; (2) extensor carpi radialis longus and brevis tendons; (3) extensor pollicis longus tendon; (4) common extensor tendons (extensor digitorum longus and extensor indicis proprius); (5) extensor digiti minimi tendon; (6) extensor carpi ulnaris tendon. R, radius; U, ulna; LT, Lister tubercle
The Guyon canal is a triangular space lateral to the pisiform bone and medial to the hamate that contains the ulnar nerve and ulnar artery. The ulnar nerve is smaller than the median nerve but has similar echostructure. More commonly, the ulnar artery is located lateral to the nerve and shows flow signals on color Doppler. Proximal to the carpal tunnel and deeper to the flexor tendons is the pronator quadratus muscle, a square-shaped muscle that lies above the distal ends of the radius and ulna.
The dorsal aspect has a transverse hyperechoic fibrous band, the extensor retinaculum, that holds the six extensor tendon compartments. The first compartment contains the tendons for the abductor pollicis longus and extensor pollicis brevis, each having its own synovial sheath. The second compartment contains the tendons for the extensor radialis longus and brevis, sharing a common synovial sheath. The Lister tubercle is a bony prominence that serves as a landmark separating the second from the third extensor compartments. The third compartment contains only one structure, the tendon for the extensor pollicis longus with its synovial sheath. The fourth extensor compartment contains the common extensor tendons (common extensor digitorum longus tendons and extensor indicis proprius tendon) that share a common synovial sheath. The fifth extensor compartment contains the tendon for the extensor digiti minimi. Last, the sixth extensor compartment contains the tendon for the extensor carpi ulnaris; both fifth and six compartments have separate synovial sheaths.
The lateral aspect houses the radial artery and the tendon for the extensor carpi radialis; and the medial aspect contains the tendon for the extensor carpi ulnaris and the triangular fibrocartilage complex (TFCC), which is located deep to the extensor carpi ulnaris tendon, between the distal segment of the ulna and the triquetrum. The TFCC comprises a meniscus homologue, the triangular fibrocartilage, an articular disk, the ulnar collateral ligament, the dorsal and volar radioulnar ligaments, and the extensor carpi ulnaris tendon and sheath. TFCC separates the carpal bones from the radius and ulna and serves as a major stabilizer of the radioulnar joint as well as a cushion for ulnar axial loads. On ultrasound, TFCC appears as a triangular hypoechoic and slightly heterogeneous structure in the medial aspect of the wrist. Because the components of TFCC cannot be defined clearly by sonography, when a lesion is suspected it is suggested that magnetic resonance imaging (MRI) be obtained for confirmation.
 Pathologies
Pathologies
Inflammatory
Tenosynovitis
Inflammation of the tendons and/or their synovial sheaths is one of the most common disorders of the wrist. The main causes are repetitive motion at work, pregnancy, inflammatory arthropathies, and diabetes. Sonographically, there is enlargement of the tendons and their synovial sheath; more chronic cases may be associated with peritendinous anechoic cysts or small hypoechoic nodules in the synovial sheath. Color Doppler ultrasound may detect increased vascularity in the synovial sheath or intratendinous (in more advanced stages) (Fig. 3.3).
De Quervain Tenosynovitis
De Quervain tenosynovitis is a common tenosynovitis of the wrist and affects the first extensor compartment, composed of the tendons for the abductor pollicis longus and the extensor pollicis brevis muscles. Symptoms include chronic pain, tenderness or swelling in the thumb side of the wrist as well as limitation of movement. Sonographic thickening of the first extensor compartment is seen on ultrasound, which also helps in severe cases when it is necessary to rule out the presence of accessory tendons, or septa in the synovial sheaths (Figs. 3.4, 3.5, 3.6, 3.7). In the postsurgical follow-up of patients with De Quervain tenosynovitis, an ultrasound examination can rule out the development of neuromas of the terminal branches of the radial nerve (Fig. 3.8).
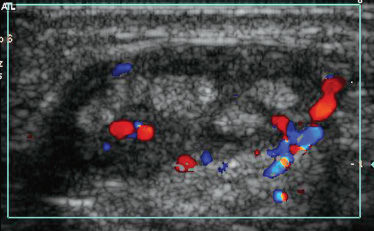
Fig. 3.3 Tenosynovitis. Color Doppler ultrasound transverse view: the common extensor tendons compartment is swollen, and the synovial sheath thickened with enhanced color Doppler ultrasound signals.
Distal Intersection Syndrome
Distal intersection syndrome, also called crossover syndrome, is a tenosynovitis at the intersection between the second (extensor carpi radialis longus and brevis) and third (extensor pollicis longus) compartments. It is caused by repetitive prono-supination or flexo-extension movements and commonly presents with pain and tenderness proximal to the Lister tubercle in the distal forearm. The most affected tendon is the extensor pollicis longus that develops tendon swelling and thickening of the sheath that may be associated with synovial sheath fluid (Fig. 3.9). There is also another less common crossing syndrome that represents a proximal intersection syndrome; this affects the distal forearm at the level of the musculotendinous junction of the first extensor compartment with the second extensor compartment tendons (radialis longus and brevis tendons). This syndrome is seen in patients with repetitive prono-supination movements and overload.
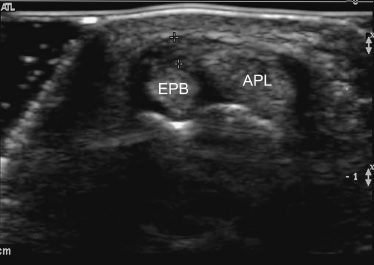
Fig. 3.4 De Quervain tenosynovitis. Transverse ultrasound view shows an abnormal swollen first extensor compartment and its synovial sheath (between markers). APL, abductor pollicis longus; EPB, extensor pollicis brevis.
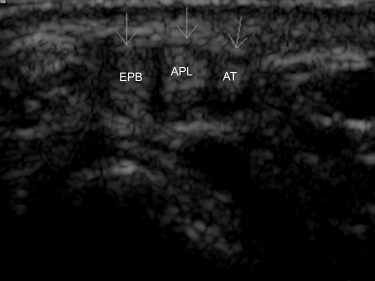
Fig. 3.5 De Quervain tenosynovitis variant, with accessory tendon. Transverse ultrasound view demonstrates enlargement of the tendons in the first extensor compartment including an accessory tendon (AT; arrows). APL, abductor pollicis longus; EPB, extensor pollicis brevis.
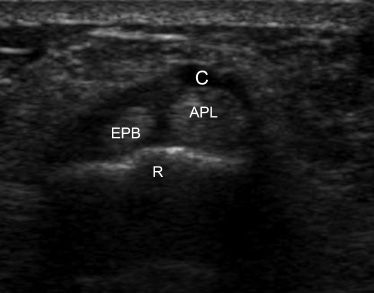
Fig. 3.6 De Quervain tenosynovitis variant, with ganglia. Transverse ultrasound view: swelling of structures as in Figs. 3.4 and 3.5, and a small ganglia cyst (C) attached to the abductor pollicis longus tendon. APL, abductor pollicis longus; EPB, extensor pollicis brevis; R, Radius.
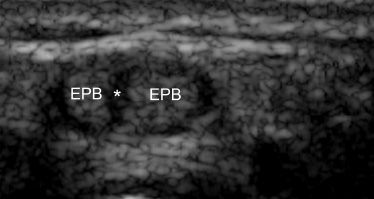
Fig. 3.7 De Quervain tenosynovitis, with a septa variant. Transverse ultrasound view shows a septa (*) dividing the swollen extensor pollicis brevis tendon (EPB) in two separate fascicles.
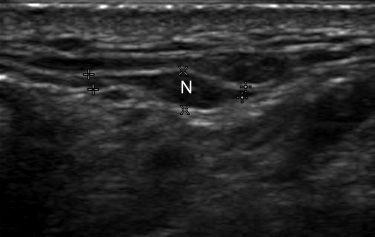
Fig. 3.8 Postoperative complication of De Quervain tenosynovitis. Longitudinal ultrasound view demonstrates a neuroma (N) of a distal branch of the radial nerve. A hypoechoic fusiform structure with connecting neurogenic tracts to the mass (between markers) is identified.
Pronator Quadratus Syndrome
The pronator quadratus syndrome, as its name indicates, affects the pronator quadratus muscle, a square-shaped muscle, located in the anterior aspect of the distal forearm, overlying the interosseus membrane. This muscle is supplied by the anterior interosseus artery and may become inflamed during maintained forced dorsiflexion of the wrist as for example, when carrying a heavy tray for a prolonged period. The muscle becomes enlarged and hyperechoic and an early diagnosis is necessary to avoid development of a full-fledged compartment syndrome (Figs. 3.10 and 3.11).
Carpometacarpal Boss
Carpometacarpal boss, also known as carpal boss, is a bony protuberance that develops at the base of the second and/or third carpometacarpal joint close to the capitate and trapezoid bones. It may represent a degenerate osteophyte and/ or an os styloideum (an accessory ossification center). Clinically, patients may report pain and limitation of movement in the affected hand, likely due to an overlying ganglion cyst, or an extensor tendon that may be slipping over the bony protuberance. On ultrasound, it is possible to detect the hyperechoic bony abnormality and/or the anechoic round or oval shaped ganglion cyst, and a dynamic study can detect the slipping tendon movement (Figs. 3.12, 3.13, 3.14).
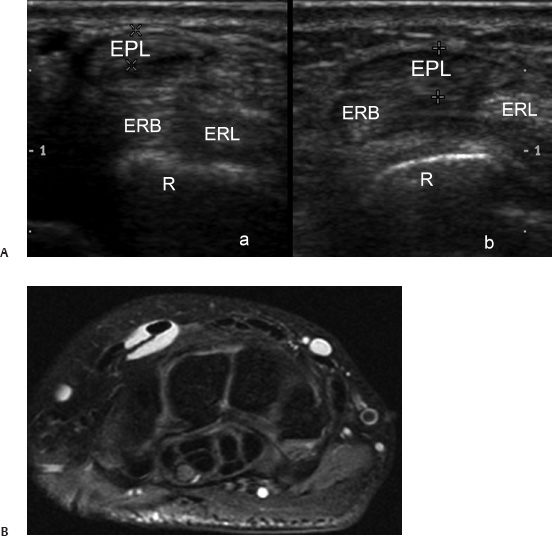
Fig. 3.9 (A) Distal intersection syndrome. Transverse comparative ultrasound views show swelling of the extensor pollicis longus tendon (EPL; between calipers) at the crossing with the second extensor compartment tendons (extensor carpi radialis longus [ERL] and brevis [ERB] tendons) in the proximal (a) and distal (b) segments of the wrist. R, radius. (B) Patient with tenosynovitis of the EPL. Axial fat-suppressed fast spin echo (FSE) T2-weighted magnetic resonance image showing fluid around the second dorsal compartment compatible with tenosynovitis.
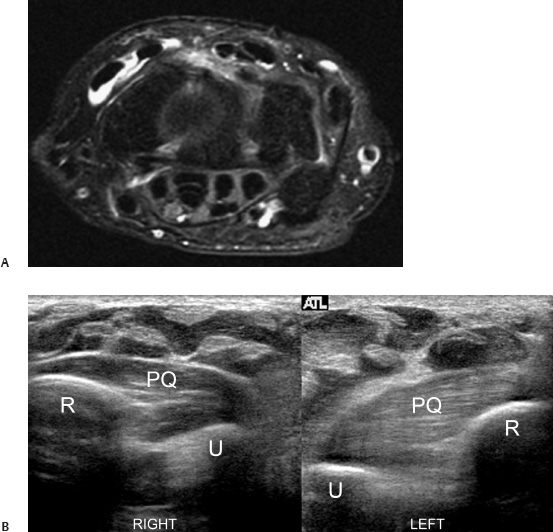
Fig. 3.10 (A) Normal pronator quadratus muscle. Axial proton density (PD) magnetic resonance image showing pronator quadratus muscle in the distal forearm attaching to the radius and ulna. (B) Pronator quadratus muscle syndrome. Transverse comparative views show swelling and hyperechogenicity of the pronator quadratus muscle (PQ) in the affected side (LEFT). The normal side is marked RIGHT. R, radius; U, ulna.
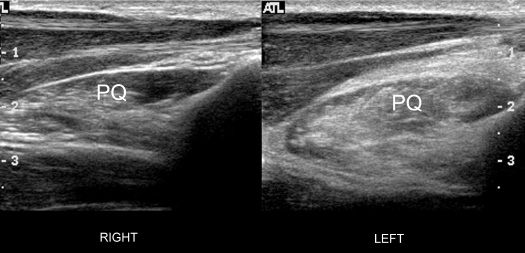
Fig. 3.11 Pronator quadratus muscle syndrome. Longitudinal comparative ultrasound views demonstrate enlargement and hyperechogenicity of the pronator quadratus muscle (PQ) in the affected side (LEFT). In contrast, the normal side (RIGHT) presents a normal hypoechoic muscular pattern in the same muscle.
Extensor Carpi Ulnaris Tenosynovitis
The extensor carpi ulnaris (ECU) inserts into the midportion of the fifth metacarpal. Tenosynovitis of the ECU can be caused by the persistent ulnar deviation of RA and may be associated with a ganglion cyst. On ultrasound, there is enlargement of the tendon and its synovial sheath (Figs. 3.15 and 3.16); in RA patients, synovial pannus is an important cause for thickening of the synovial sheath.
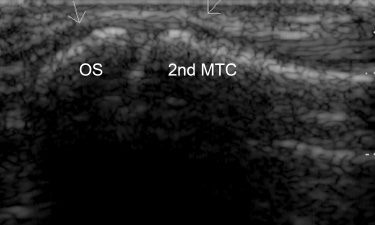
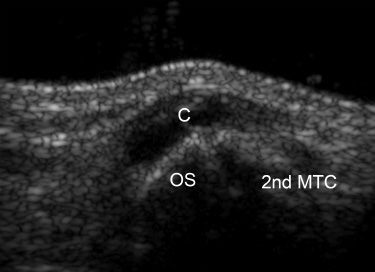
Fig. 3.13 Carpal boss and ganglia cyst. Longitudinal ultrasound view presents a round anechoic cyst (C) above the dorsum of the os styloideum (OS) at the base of the second metacarpal bone (2nd MTC).

Fig. 3.14 Carpal boss. X-ray projection (lateral view) shows bony prominences with degenerative osteophytes (arrows).
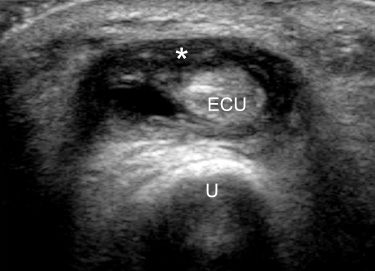
Fig. 3.15 Extensor carpi ulnaris tendon (ECU) tenosynovitis. Transverse ultrasound view demonstrates swelling of the tendon as well as thickening and fluid in the synovial sheath (*). U, ulna.
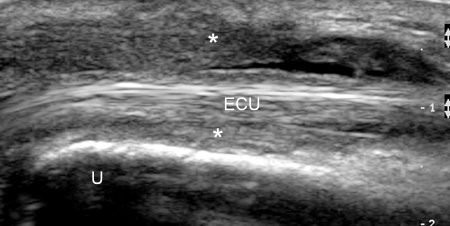
Fig. 3.16 Extensor carpi ulnaris tendon (ECU) tenosynovitis in longitudinal ultrasound view demonstrates an important thickening of the synovial sheath (*). U, ulna.
Flexor Carpi Ulnaris Tendinitis
Flexor carpi ulnaris (FCU) tendinitis is a common problem in players of racquet sports, due to the chronic repetitive trauma associated with forced wrist flexion or ulnar deviation. Symptoms are pain along the tendon or in its distal insertion around the pisiform; the FCU tendon does not have synovial sheath covering. Pain in FCU tendinitis may also arise from arthrosis of the pisotriquetral joint or instability of the pisiform. Because calcific tendinitis of the FCU has been reported in relation to trauma, its primary mechanism may be local hypoxia from mechanical causes or vascular abnormalities.
Flexor Carpi Radialis Tendinitis
Flexor carpi radialis (FCR) tendinitis is seen less frequently than FCU tendinitis and is also associated with repetitive trauma. The flexor carpi radialis tendon passes through a separate compartment of the transverse ligament apart from the rest of the flexor tendons and overlies the scaphoid tubercle and trapezial crest. Adhesions in the tunnel or constriction of the distal tendon secondary to trauma or arthrosis may trigger the typical pain. The close relationship between the FCR and the median nerve may occasionally generate secondary irritation of the nerve.
Inflammatory Arthropathies
Ultrasound is a sensitive imaging technique for the evaluation of joint fluid, synovitis, erosions, cartilage destruction, or calcifications. Rheumatoid arthritis and crystal disease are common causes of inflammatory diseases affecting the wrist.
Rheumatoid Arthritis
Rheumatoid arthritis is characterized by proliferative and hypervascularized synovitis, bone erosion, cartilage damage, joint destruction, and long-term disability. Proliferative synovitis (i.e., rheumatoid pannus) is the earliest pathologic abnormality in RA and may be associated with small amounts of fluid in the joint. Doppler color imaging shows synovial thickening and high signals in the synovial sheath that together suggest proliferative, hypervascularized pannus tissue that can be quantified and subsequently monitored (Figs. 3.17 and 3.18). Furthermore, use of micro-bubbles sonographic contrast agents may enhance detection of synovial vascularization, a marker of disease activity. The data generated can be applied to a scoring system developed by EULAR (European League Against Rheumatism) used to assess and standardize RA and its complications. Tenosynovitis is a common finding in RA. It is usually bilateral and affects mainly the tendons for the flexor digitorum, extensor digitorum longus, and extensor carpi ulnaris. Bone erosions are detected on ultrasound as intraarticular discontinuities of the bone surface visible on two planes perpendicular to each other. Most commonly, bone erosions affect the capitate, triquetrum and lunate in the carpal region, and the ulnar styloid process (Fig. 3.18b).
Crystal-Related Arthritis
Crystal-related arthritis is a group of disorders characterized by deposition of microcrystals in the joints resulting in acute or chronic arthritis or periarthritis. Disease-producing crystal deposits are mostly monosodium urates, causing gout, and calcium pyrophosphate dihydrate (CPPD) causing pseudogout.
Gout
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





