▪
Introduction
Thoracic injury is a common sequela of acute trauma and is the third most common injury in trauma patients, after head and extremity injuries. The overall mortality rate approaches 25%, with acute aortic, tracheobronchial, and cardiac injuries often having an even worse prognosis. Given the high mortality rate and the impact on clinical management, rapid and accurate assessment of thoracic trauma imaging is imperative.
▪
Appropriateness of Imaging Modalities and Technique
When CT Should Be Performed
There are conflicting data in the literature on whether routine chest CT should be performed in all cases of thoracic trauma. Chest CT is much more accurate than chest radiography in evaluating thoracic trauma, with at least 50% of pneumothoraces, rib fractures, and pulmonary contusions missed on routine anteroposterior chest radiographs. Some studies have shown that CT changes management in a significant proportion of patients, and potentially fatal injuries such as aortic laceration could be missed. Other studies have shown that with appropriate clinical assessment and use of other radiographic and demographic data, patients can be selected for whom chest CT would be more likely to identify injuries, thus saving cost and radiation. The American College of Radiology Appropriateness Criteria for blunt thoracic trauma in 2014 have suggested that CT should be strongly considered in patients with “high-mechanism injury, abnormal chest radiographs, altered mental status, distracting injuries, or clinically suspected thoracic injuries. CT angiogra[phy] should be routinely used in patients with suspected acute aortic laceration.”
Appropriate Imaging Protocol
Unless contraindicated due to allergy or renal failure, contrast should be used in all CT scans of thoracic trauma. This allows for much more accurate assessment of vascular injury, which is a significant cause of morbidity and mortality in thoracic trauma. In most cases, precontrast images are not necessary. It is also important to choose a reconstruction algorithm with some degree of overlap. This allows for high-quality multiplanar reconstructions, which can be very helpful in the detection of certain types of thoracic injury.
▪
Abnormal Gas and Fluid Collections
In the setting of trauma, gas and fluid can accumulate in different thoracic spaces, with different causes and clinical significance. It is important to be aware of each of these to direct the appropriate management of the trauma patient.
Pneumothorax
Incidence of Pneumothorax in Trauma; Occult Pneumothorax
Pneumothorax or air within the pleural space occurs in up to 20% to 40% of blunt trauma patients presenting to the emergency department. Up to 50% of pneumothoraces may be missed with portable radiography ( Fig. 43.1A ). These are termed occult pneumothoraces and are rarely symptomatic. However, in the setting of positive end-expiratory pressure mechanical ventilation, they can significantly enlarge, and therefore are often drained with a chest tube.



Pitfalls in Diagnosis
On a chest radiograph, one should be careful not to mistake a skin fold for a pneumothorax. The pleural line in a pneumothorax is seen as a thin white line, with no lung markings beyond it, whereas a skin fold is often less dense, has lung markings beyond it, and can be seen projecting into the soft tissues. Mach bands, which are due to an optical illusion resulting in incorrect perception of density at the borders, of varying shades of gray, can also simulate pneumothorax on chest radiograph. On chest CT, use of a sharp kernel such as with a bone algorithm can result in an artifact mimicking pneumothorax.
Determining if There Is Tension Physiology
One of the most important findings to assess is whether there are signs of tension physiology because this can be lethal to the patient. Signs of tension in the pleural space from pneumothorax or hemothorax include contralateral mediastinal shift, flattening or inversion of the ipsilateral hemidiaphragm, and a hyperexpanded ipsilateral chest (see Fig. 43.1B and C ). If these signs are seen, emergent decompression is warranted because cardiovascular collapse can occur.
Associated Injuries
Rib fractures are commonly associated with pneumothorax, and careful attention should be given to the ribs when a pneumothorax is seen in the setting of trauma. Multiple contiguous segmental rib fractures are termed flail chest, which has a high (≈50%) association with injuries requiring surgical treatment and prolonged mechanical ventilation.
Pneumomediastinum
Cause of Pneumomediastinum in the Traumatic Setting
Most cases of pneumomediastinum in blunt thoracic trauma are due to the Macklin effect, which is alveolar rupture resulting in gas dissecting along the bronchovascular sheath into the mediastinum ( Fig. 43.2 ). This is typically due either to barotrauma or increased pressure against a closed glottis.




Associated Injuries
In the setting of trauma, one should always carefully assess the esophagus and tracheobronchial tree because direct injury to these structures can result in pneumomediastinum.
Pneumopericardium
Importance of Pneumopericardium and Associated Injuries
Pneumopericardium, or air within the pericardial space, implies a defect in the pericardium and is unusual after blunt thoracic trauma. Pneumopericardium in the setting of penetrating trauma, however, can be enough to warrant surgical exploration to assess for cardiac injury. When encountered, one should carefully assess for any pericardial defect and look for signs of cardiac injury. CT cannot exclude cardiac injury because the right ventricular free wall, the most anterior portion of the heart, is only 2 to 3 mm thick, and lacerations are often not seen.
Hemothorax
Signs of Hemothorax
Hemothorax is blood within the pleural space. In the setting of trauma, one should always measure the attenuation of fluid in any space including the pleura, because this can direct management ( Fig. 43.3A ). Blood generally measures between 30 and 70 Hounsfield units. One should also assess for any focal areas of high attenuation close to a blood pool, which may represent pseudoaneurysm or active extravasation, because these may require surgical or intravascular treatment (see Fig. 43.3B ). Most hemothoraces will require chest tube placement to prevent the development of constrictive fibrothorax.



Massive Hemothorax
Drainage can also help guide management. This is because a massive hemothorax (initial drainage >1 L, or rapid drainage, 100 mL/h for 5 hours) can indicate the need for surgical exploration.
Hemopericardium
Signs of Hemopericardium and Associated Injuries
Hemopericardium is blood within the pericardial space. If fluid is seen in the pericardial space, it is important to measure the attenuation of the fluid, especially in the setting of trauma. In the setting of penetrating trauma, like pneumopericardium, hemopericardium can be enough to warrant surgical exploration. If hemopericardium is seen, always carefully assess the heart, aorta, and great vessels to look for a potential source. Often a source cannot be readily determined.
Extrapleural Hematoma
Signs of Extrapleural Hematoma and Associated Injuries
The extrapleural space is the potential space that exists between the parietal pleura and the body wall, diaphragm, and mediastinum. When blood accumulates in this space, it is known as extrapleural hematoma. This is relatively uncommon in the setting of trauma occurring in approximately 7% of cases; however, if seen, it is almost always associated with rib fractures and commonly associated with hemothorax (see Fig. 43.3C ). The morphology of the hematoma can help guide management because biconvex hematomas are thought to be due to the higher pressure of arterial bleeding and require surgical decompression more often.
Localizing Abnormal Gas Collections on Chest Radiography and CT
Pneumothorax and pneumopericardium are caused by air within true potential spaces, whereas pneumomediastinum is air within a false space. Because of this, on chest radiography, if the patient changes position, pneumothorax and pneumopericardium will change location to the most nondependent area, whereas pneumomediastinum will generally not move. On chest CT, one can differentiate these entities because pneumomediastinum, being within a false space, will have multiple webs interspersed between the air collection, as opposed to pneumopericardium and pneumothorax, which generally do not.
Determining Signs of Tamponade
Cardiac tamponade refers to a clinical syndrome caused by the accumulation of air or fluid in the pericardial space resulting in hemodynamic compromise. Signs of cardiac tamponade on imaging include collapse of the heart chambers, flattening of the anterior border of the heart, and distention of the inferior vena cava on CT. On frontal chest radiograph, what is known as the small heart sign has been described when there is a sudden decrease in the size of the cardiac silhouette.
▪
Lung Parenchymal Injury
Contusion
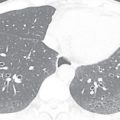
Imaging Appearance of Pulmonary Contusion
Pulmonary contusion is the most common lung injury occurring in blunt thoracic trauma. It is due to traumatic alveolar hemorrhage, but without significant alveolar injury. It can occur at the site of injury or sometimes opposite the site of injury in a contrecoup pattern. CT signs include nonsegmental patchy air space opacity and consolidation. Subpleural sparing may also be observed because this can mimic centrilobular nodules. Pulmonary contusions often do not respect normal anatomic borders and can cross fissures ( Fig. 43.4A and B ).