The observation that a child has a limp is not a diagnosis, but rather a manifestation of an underlying problem. A limping child has altered gait, which may or may not also be antalgic. This is a commonly encountered phenomenon in pediatric medicine, and ~4% of all pediatric patient visits are related to acute onset of limp or refusal to ambulate. The causes of limp in childhood are many and span a broad range of etiologies including, but not limited to, congenital abnormalities, infection, trauma-related injury, neoplastic conditions, neuromuscular disease, and vascular insult. A proper clinical history and physical examination are crucial for narrowing down an otherwise extensive differential. Certain physical examination findings or maneuvers may assist in tailoring an appropriate differential diagnosis. For instance, observation of circumduction during gait suggests an ankle or foot problem. Similarly, absence of or decreased ability to internally rotate the hip raises concern for Legg-Calvé-Perthes (LCP) or slipped capital femoral epiphysis (SCFE). A Trendelenburg gait in which the pelvis tilts downward and away from the affected hip as a result of weakening of the contralateral gluteus medius muscle is associated with unilateral developmental hip dysplasia, SCFE, and LCP.
Despite having adequate clinical history and the aid of physical examination maneuvers, often a single cause cannot be isolated. The clinical history is not always easily elucidated from young children, and there may be overlapping or confounding clinical features. In many of these instances, imaging plays a crucial role in narrowing the differential diagnoses from a broad list of various entities to a more focused concern. This is important not only for arriving at the correct diagnosis but also for recognizing potential life- or limb-threatening entities that require immediate intervention.
What Imaging Modalities Are Useful for Working Up a Limp in a Pediatric Patient?
A variety of diagnostic imaging modalities may be useful for the assessment of the various causes of limp in a child. Imaging may be targeted to the lower extremities, pelvis, or spine depending on what is felt to be most contributing to the altered gait. Plain radiographs are generally the most frequent, initially used imaging modality. Plain radiographs are widely available, straightforward to perform, relatively low cost, and well suited to demonstrate many osseous abnormalities that cause a limp without need for further imaging. Sonography is another vital imaging tool in children, particularly when assessing for joint effusions. Magnetic resonance imaging (MRI), computed tomography (CT), and bone scintigraphy are imaging modalities that may be useful depending on the specific clinical features and differential diagnoses under consideration. The role of imaging should be to aid in diagnosis in the context of relevant history and physical examination findings, as well as to separate benign from more aggressive entities that require urgent attention. In addition, the radiologist should help guide appropriate imaging depending on the available clinical information with the primary goal of promoting patient safety by expediting a correct diagnosis while minimizing radiation exposure.
What Is the Utility of Radiographs?
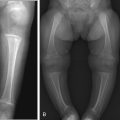
In most situations the initial imaging approach to the limping child will be to obtain plain radiographs of the area in question. Radiographs are most useful in screening for traumatic causative factors, such as fractures, to assess the overall anatomy, positioning and morphology of the bones, and to ensure normal growth and development. Focal bone lesions, periosteal new bone formation indicative of underlying fracture or lesion, areas of bone infection or neoplasm ( Fig. 10.1 ), and avascular necrosis are conditions that may be identified based on radiographic features alone. Radiographs may also detect large joint effusions, although they should not be relied on for screening ( Fig. 10.2 ). Occasionally soft tissue masses with or without calcification may be detected on radiographs because of obliteration of normal soft tissue planes ( Fig. 10.3 ).



When the limping child is able to identify a focal area of concern, at least two orthogonal views of the anatomic area should be obtained. These often include anteroposterior (AP) and lateral radiographs of the area of concern. Additional views may be necessary depending on the anatomic area or the initial findings. Mortise views in the setting of ankle pain or oblique views of the tibia in suspected toddlers’ fracture may increase diagnostic yield. In younger children (generally younger than 4 years) or in patients unable to localize the area of concern, initial radiographs can be focused on the tibia/fibula, because a toddler fracture is the most commonly seen abnormality (see American College of Radiology appropriateness criteria in Milla et al. [2012]). Comparative radiographs of the contralateral limb will increase radiation exposure and are usually not necessary in routine imaging. If radiographs are considered indeterminate or subtle findings are detected with unclear significance, imaging of the contralateral side may be helpful in select cases to rule out normal developmental variations ( Fig. 10.4 ).

Hips are the exception to the routine practice of unilateral imaging of the affected side. When hip pathologies are under consideration, AP and frog-leg lateral views are obtained of both hips together. The normal side may serve as a normal control with regard to the developmental ossification pattern of the acetabulum and proximal femur, and also to evaluate for other pelvic processes such as avulsion injuries ( Fig. 10.5 ) and sacroiliac joint disease that are made more conspicuous by the asymmetry with the unaffected side. Frog-leg lateral views are obtained with the limb flexed both at the knee and the hip approximately 30 to 40 degrees and with the hip externally rotated 45 degrees. The frog-leg views are more sensitive than AP views for detection of entities such as SCFE ( Fig. 10.6 ) and LCP ( Fig. 10.7 ). The initial AP film should include the entire pelvis without gonadal shielding to assess other pelvic anatomy, including the sacrum and sacroiliac joints. The frog-leg view should use gonadal shielding to minimize exposure to radiosensitive organs.



What Is the Utility of Sonography?
Sonography is a widely implemented imaging modality in pediatric imaging because of lack of ionizing radiation and capability for dynamic real-time imaging. Pediatric patients are particularly well suited to ultrasound because of their relatively small body habitus, which allows for improved image resolution. Images can also be acquired without the use of sedation by relying on methods of patient distraction to encourage cooperation during the examination. Although osseous structures with dense cortical bone are suboptimally assessed with ultrasound, the surrounding soft tissues are often depicted beautifully. In the neonatal period when the cartilaginous femoral head has not yet ossified, ultrasound is the imaging modality of choice for early diagnosis of developmental hip dysplasia ( Box 10.1 ; Fig. 10.8A–B ). After the age of 6 months, imaging diagnosis is typically made by radiography (see Fig. 10.8C ). Radiographs will show increased acetabular angle (typically greater than 30 degrees) and subluxed or dislocated hip. The proximal femoral epiphysis of the affected hip is typically smaller than the contralateral normal hip.
May develop before or after birth
Femoral head may migrate out of joint secondary to joint laxity or acetabular underdevelopment
Screening ultrasound in the United States indicated in setting of abnormal newborn physical examination or risk factor (family history, torticollis, breech delivery, clubfoot, twin)
Left hip more commonly affected
Sonographic evaluation consists of both static and dynamic maneuvers through a lateral imaging approach with coronal and transverse planes

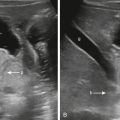
Ultrasound has much greater sensitivity compared with radiographs for detecting small fluid collections in the joints and soft tissues. Ultrasound is the study of choice for evaluation of joint effusions, particularly hip effusions, either in the setting of aseptic (transient synovitis) or septic arthritis ( Fig. 10.9 ). Synovial thickening and hyperemia can also be readily identified on ultrasound in the setting of synovitis. Ideally, assessment for a hip effusion should be performed with a high-frequency linear array transducer, oriented in a sagittal plane along the axis of the femoral neck anteriorly. Imaging of the contralateral hip is imperative to assess for bilateral involvement and for accentuation of unilateral effusion. Bilateral effusions may suggest systemic arthritic disease over septic arthritis. The adjacent soft tissue structures may also be interrogated with ultrasound to evaluate for myositis or soft tissue fluid collections such as abscess.

Some authors propose the use of ultrasound to follow disease in patients with known juvenile idiopathic arthritis (JIA). This will be discussed in further detail toward the end of the chapter.
Is There a Role for Bone Scans?
Bone scans may be used to isolate causes of limp in young children (younger than 5 years) especially in the setting of nonlocalizing symptoms on physical examinations. Perhaps one of the best implementations of bone scans in pediatric patients is in the evaluation of suspected stress fractures, especially involving the tarsal bones. Other fractures, such as the classic toddler fracture of the tibia, can also be seen with slightly increased sensitivity on bone scan compared with plain radiographs ( Fig. 10.10 ), although radiographs remain the initial first-line approach because of their lower cost and decreased radiation dose. In addition to their potential utility in the evaluation of stress fractures, bone scans have other applications, including identifying primary bone tumors and metastatic disease, separating cellulitis from osteomyelitis and prosthetic loosening in patients with orthopedic hardware, assessing for osteoid osteoma, and assessing bone viability (infarction versus avascular necrosis), to name a few.

Bone scans are considered second-line imaging studies in the setting of trauma when radiographs fail to demonstrate suspected fractures. Radiographically occult fractures are often visible on bone scintigraphy. Similarly, bone scans are more sensitive than radiographs for detecting osteomyelitis, diskitis, avascular necrosis, bone infarcts, and bone neoplasms.
Traditional bone scanning agents are technetium-labeled diphosphonates, namely 99m Tc-methylene diphosphonate (MDP). Diphosphonates are useful agents because these have rapid renal excretion and high target-to-nontarget ratios. Imaging may consist of only a single delayed skeletal phase or three-phase imaging, depending on the indication and concern. The three phases are generally performed in the setting of infection/inflammation and demonstrate an initial angiographic (blood flow) phase, blood pool (soft tissue) phase, and delayed (skeletal) phase with chemisorption of the agent on the bone. These various phases not only demonstrate bony abnormalities but can also detect pathology in the soft tissues, such as cellulitis.
A newer agent, 18 F sodium fluoride ( 18 F-NaF) is an analogue for hydroxyl ion in the bone matrix and is another useful bone-imaging agent due to its high initial extraction efficiency. An 18 F-NaF bone scan detects areas of altered osteogenic bone activity. With both rapid bone uptake and clearance, there is a high bone-to-background ratio much like traditional 99m Tc-MDP. However, this is coupled with higher imaging resolution of positron emission tomography (PET) scanners, which are used to detect 99m Tc tracer accumulation. As a compounded result, PET/CT 18 F-NaF bone scans have better anatomic and spatial resolution than the traditional MDP bone scans and are acquired over much shorter durations after tracer injections. These newer bone scans have not replaced traditional 99m Tc-MDP imaging, however, because of higher costs and increased radiation doses. In indications where higher-resolution imaging is beneficial, for example, evaluating adolescent back pain or in nonaccidental trauma with equivocal radiographs, 18 F-NaF is preferred over 99m Tc-MDP bone scans ( Fig. 10.11 ).

Is There a Role for Computed Tomography?
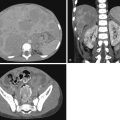
In general, CT scanning is performed uncommonly and judiciously in the limping child because of the potentially harmful effects of ionizing radiation. In the particular scenario of initial presentation of a child with a limp, CT has a limited role. If a complex fracture is present, CT may be beneficial in preoperative planning, especially if there are concerns for intraarticular extension of fracture lines or concerns for loose bodies within the joint. CT may also be beneficial in instances where osteoid osteoma is on the differential to assess for lucent nidus with central calcification ( Fig. 10.12 ; Box 10.2 ). CT scans may also show osteopenia early in the course of tibial stress fractures. In cases where limping is due to referred pain because of spinal or paraspinal processes, CT of the lumbosacral spine or pelvis may be beneficial to assess for psoas abscess or bony destruction in vertebral body osteomyelitis, or assess for raging appendicitis, which may lead secondarily to muscle spasms and contractures. Lastly, CT scans of the ankles are routinely performed in cases of altered gait and pes planus deformity to assess for underlying tarsal coalition as a mechanical cause.

Benign bone tumor less than 1.5 cm
Most common between age 4 and 25 years, and three times more common in males
Femur and tibia are the most common locations
Lesions do not grow, but incite large amount of surrounding reactive bone
Patients present with dull, aching pain unrelated to activity that can become severe at night
When to Consider Magnetic Resonance Imaging?
Like ultrasound, MRI does not require the use of ionizing radiation. MRI is superior to ultrasound at imaging osseous structures and also provides a more global evaluation of the area of concern. The variety of different imaging sequences in MRI allows for tailored protocols that address specific clinical questions and increase diagnostic certainty, making MRI an exceptional tool in evaluation of many pediatric conditions that cause a limp. The drawbacks of MRI are that it is expensive, relatively time consuming, and often difficult to perform in younger patients without the use of anesthesia. Contrast administration is usually not necessary but may be beneficial in certain conditions, such as the evaluation of infection, tumor, or synovitis.
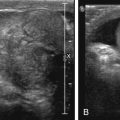
When osteomyelitis is high on the differential and precise anatomic localization is not possible, whole-body MRI using coronal fluid-sensitive fat-suppressed sequences may be considered to identify areas of abnormal bone marrow edema or soft tissue abnormalities. MRI can detect intraosseous, subperiosteal, or soft tissue abscesses, especially on contrast-enhanced sequences. Even with the presence of limp or localizable involvement, multifocal osteomyelitis is more likely to be detected by large initial field of view. In addition, less common causes of limp, such as diskitis and vertebral body osteomyelitis, may not be detected unless the field of view is expanded. A screening, wide-field-of-view MRI of the lower extremities may be beneficial in a variety of different clinical scenarios, particularly in a child who is cooperative and does not require anesthesia ( Fig. 10.13 ). For instance, a patient diagnosed with and undergoing treatment for septic arthritis of the hip who is not responding to antibiotics may have an associated osteomyelitis or soft tissue abscess. MRI may facilitate diagnosis in these patients and direct them toward more appropriate treatment. In addition, in patients with puzzling clinical presentations where fractures have been excluded on radiographs and infection is not considered likely based on clinical factors, other soft tissue injuries such as tendinosis or tendon tear, ligament injury, muscular strains, or articular cartilage damage are best assessed by MRI.

Despite increased sensitivity for detecting focal marrow lesions or areas of marrow edema, whole marrow infiltrative or replacement processes may be difficult to appreciate if the abnormality is diffuse and uniform in appearance. For this reason, it is important to take note of the marrow signal characteristics on individual imaging sequences to ensure that marrow signal is following the expected pattern. In most ambulatory or school-age patients undergoing MRI imaging, it would be reasonable to expect the diaphysis of the long bones to demonstrate fatty marrow signal, which is bright on T1-weighted sequences and dark when fat suppression techniques are applied. If the marrow appears dark on T1-weighted images or bright on fluid-sensitive sequences with fat suppression, a diffuse marrow process, such as a lymphoproliferative disorder, must be considered, for example, leukemia or lymphoma ( Box 10.3 ). Also, MRI lacks the fine spatial resolution of CT and may obscure tiny abnormalities, such as the nidus in an osteoid osteoma. Secondary signs of disease may be helpful in these patients, such as geographic marrow edema, cortical thickening, or synovitis (when the lesion is intraarticular).
Usually affects children between 2 and 10 years of age
Most common malignancy in children between 1 and 4 years of age
~40% of children with acute lymphoblastic leukemia present with bone pain confined to a single limb
May have nearly normal hematological values if bone pain is presenting symptom
Radiographic signs may include clear metaphyseal bands, lytic or sclerotic bone lesions, or periosteal elevation (although radiographs are often normal)
How Does the Patient’s Age Affect Imaging Workup?
Much like other pediatric disorders, patient age affects the diagnostic approach to the child with a limp. It may be helpful to categorize patients into one of three categories when determining which imaging studies will be most helpful in the workup of the limping child: young children (younger than 4 years), older children (older than 4 years but younger than 10 years), and adolescents (older than 10 years). A subcategory of young children includes infants, those younger than 1 year and not yet ambulating but who may present with altered morphology, decreased tone, or delayed developmental milestones that suggest and precede later onset of gait abnormalities. In neonates and infants, congenital, metabolic, and/or endocrine derangements may present in this manner, although infection, trauma (including nonaccidental injury; Box 10.4 ), and tumor also remain on the differential.
Radiographic skeletal survey for diagnosis of child abuse includes the following separate radiographs:
- ▪
AP and lateral all appendicular bones
- ▪
AP and lateral skull
- ▪
Lateral thoracic and lumbar spine
- ▪
Lateral cervical spine (separate)
- ▪
AP chest (+/− oblique ribs)
- ▪
AP abdomen
- ▪
AP pelvis
Coned-down views may be added at discretion of radiologist.
High-specificity injuries include:
- ▪
CMLs
- ▪
Multiple and posterior rib fracture
- ▪
Scapular fractures
- ▪
Sternal fractures
In select instances, whole-body 18 F-NaF PET bone scans may supplement (but never replace) initial skeletal survey. 18 F-NaF PET bone scans may be more sensitive for rib fractures but have lower sensitivity for CMLs.
Mimics of abuse include normal developmental variants, rickets, Menkes disease, and osteogenesis imperfecta.
In younger children the broad differential diagnosis for a limp includes trauma, toxic synovitis, osteomyelitis, septic arthritis, developmental hip dysplasia (DDH), leg-length discrepancy, and inflammatory arthritis (JIA) ( Box 10.5 ). In older children, trauma, toxic synovitis, osteomyelitis, and septic arthritis remain high on the differential, and LCP disease also becomes a serious consideration. In adolescents, trauma, sports-related injuries (stress fractures), osteomyelitis, septic arthritis, SCFE, chondromalacia, and neoplasm are higher on the differential. Infection and trauma are common processes that affect all patient populations regardless of age.