Traditional evaluation of the small bowel involved small bowel follow-though (SBFT) or enteroclysis, which provide excellent survey of the small bowel but are insensitive for subtle bowel pathologic processes and extraluminal abdominal findings. Within the last decade, as a result of significant advances in technology there has been a paradigm shift in the imaging evaluation of the gastrointestinal tract. With the advent of multidetector computed tomography (MDCT) and advances in abdominal magnetic resonance imaging (MRI) along with administration of oral contrast media, it is now possible to effectively evaluate bowel wall thickening, enhancement, and extraluminal findings to detect and characterize small bowel pathologic processes. Although used less frequently in small bowel evaluation, ultrasound and nuclear medicine techniques have utility in the diagnosis of small bowel pathologic processes. A comparison of the various imaging modalities available for imaging the small bowel is presented in Table 24-1 .
| Modality | Pros | Cons |
|---|---|---|
| Small bowel follow through |
|
|
| Fluoroscopic enteroclysis |
|
|
| Abdomen/pelvis CT |
|
|
| CT enterography |
|
|
| CT enteroclysis |
|
|
| MR enterography |
|
|
| MR enteroclysis |
|
|
Fluoroscopic Small Bowel Imaging Techniques
Small Bowel Follow-Through
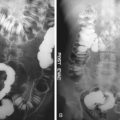
An SBFT examination involves ingestion of approximately 600 to 1200 mL of a low-density barium solution (30% to 50% weight/volume [w/v]). Patient preparation usually involves the patient having a nothing by mouth (NPO) status after midnight. After ingestion of the barium solution, overhead spot images of the abdomen ( Figure 24-1 ) are obtained at intervals of 15 to 60 minutes depending on small bowel motility. Fluoroscopic evaluation of the small bowel is performed to evaluate any potential pathologic processes identified on spot images or to delineate superimposed bowel loops. Particular fluoroscopic attention is paid to the terminal ileum ( Figure 24-2 ), a location at which numerous infectious and inflammatory conditions often manifest. The examination concludes when the contrast reaches the ascending colon. Small bowel transit time—the time it takes to reach the ascending colon after ingestion of contrast—should be reported, because it is a useful clinical indicator. For normal patients, typical transit times range from 1 to 3 hours, although in patients with ileus or bowel obstruction transit times can be significantly longer.


Fluoroscopic Enteroclysis
Fluoroscopic small bowel enteroclysis involves nasojejunal intubation followed by balloon inflation and brisk instillation of low-density barium (20% to 40% w/v) at an initial rate of 75 mL/min for a total volume of 600 to 1200 mL. Subsequently, water is instilled until the terminal ileum is reached ( Figure 24-3 ). Enteroclysis often allows excellent bowel distention because of the brisk rate of contrast instillation, although the procedure can be poorly tolerated by patients secondary to discomfort from nasojejunal tube placement, abdominal discomfort, distention from balloon inflation, and contrast instillation. The patient is made NPO after midnight before the examination with a clear liquid diet and/or osmotic cathartic the day before the examination. Metoclopramide is often administered 30 to 60 minutes (if administered orally) or 1 to 3 minutes (if administered intravenously) before the examination to relax the pyloric sphincter and increase duodenal contractions to ease the 8 to 13 French nasojejunal tube placement.

Small Bowel Computed Tomography Techniques
Abdominal and Pelvic Computed Tomography
Typical routine CT abdomen and pelvis protocols are optimized to evaluate both solid organs and bowel using positive oral contrast media. The technique can evaluate areas of bowel dilatation or narrowing and is especially helpful in distinguishing partial and complete small bowel obstructions, in which no distal oral contrast is identified in complete small bowel obstructions. Often, the transition point can be determined by change in bowel caliber coupled with distal bowel decompression in high-grade partial small bowel obstructions. The small bowel transit time is often increased in partial small bowel obstructions with associated dilutional effects in loops of bowel distal to the obstruction, secondary to mixing with increased fluid accumulated proximal to the obstruction. Thus, it may be helpful to increase the standard postingestion delay of 1 to 2 hours, to more accurately evaluate the entire small bowel in patients with clinical concern for bowel obstruction.
Although positive oral contrast media have the ability to readily distinguish bowel from adjacent structures, the inherent high density of the media makes it difficult to identify subtle bowel pathologic processes. Thus, the media rely on the structural changes in bowel, to recognize abnormalities. In addition, poor mixing of positive oral contrast and enteric debris can result in fillings defects that can manifests pseudolesions.
Computed Tomography Enterography
Neutral oral contrast is used in CT enterography, which is becoming the default modality for initial evaluation of the small bowel ( Figure 24-4 ). The technique allows for appreciation of bowel mucosal changes and ulceration, which are not readily appreciated on positive oral contrast examinations ( Figure 24-5 ). To optimally evaluate the bowel mucosal changes, the technique requires optimal bowel distention, neutral oral contrast, and appropriate phase(s) of contrast. Optimal bowel distention is achieved through slow administration of a large volume of a neutral oral contrast agent (1 to 2 L), including a 0.1% w/v barium sulfate solution (VoLumen, Bracco, Milan, Italy), water-methyl-cellulose solution, or polyethylene glycol. An optimal technique would require patients to abstain from solid foods for 4 hours before the examination, to prevent mistaking food debris from intraluminal pathologic processes. Many protocols split up the contrast bolus into thirds at 15- to 20-minute intervals with an additional 200 to 300 mL of water or neutral contrast ingested immediately before imaging. The bowel is imaged in the “enteric” phase at 45 to 50 seconds postcontrast with high-volume flow rate of intravenous iodinated contrast at 4 mL per second.

CT enterography can be performed as a single-phase or multiphase examination, depending on the indication. Single-phase examinations are often performed for evaluation of inflammatory bowel disease (IBD) at initial presentation and for acute exacerbations of IBD symptoms. Patients with IBD often present at a young age in the second or third decades of life and require multiple follow-up imaging examinations for evaluation of disease involvement, treatment response, acute or chronic symptoms, and complications. Thus, radiation dose is an important consideration for a population that often will be imaged early in life and continue to have numerous imaging examinations. Multiphasic CT enterography protocols often involve evaluation for mesenteric ischemia or occult gastrointestinal bleeding, both of which occur more often in older populations during acute events, for which multiple subsequent imaging evaluations are not often required. Mesenteric ischemia protocols are often performed in the arterial (25- to 30-second delay) and portal venous (65- to 70-second delay) phases, to evaluate the small bowel mesentery arterial and portal venous vasculature, respectively. Occult gastrointestinal bleeding protocols often image the bowel using a noncontrast phase to evaluate for hyperdense enteric contents that could be mistaken for blood products, followed by arterial, portal venous, and delayed (3 to 5 minutes postcontrast) phases, evaluation for intraluminal contrast that accumulates on delayed images.
Computed Tomography Enteroclysis
CT enteroclysis is the gold standard in CT of the small bowel. There are many indications, including low-grade small bowel obstruction, IBD, obscure gastrointestinal bleeding, and small bowel tumors. After nasojejunal intubation, a large volume of neutral enteric contrast medium is rapidly infused directly into the proximal jejunum by an infusion pump, followed by thin-section CT with intravenous contrast material. Compared with routine CT and CT enterography, the strength of this technique is the enteral volume challenge by nasojejunal intubation, which allows controlled rapid infusion of large volumes of enteric contrast material, thereby optimizing the degree and extent of small bowel distention ( Figure 24-6 ). It is also advantageous compared with capsule endoscopy because it allows evaluation of the entire abdomen and is not affected by small bowel obstruction, which is an absolute contraindication in capsule endoscopy. Because of the invasive nature of this examination, patients may require sedation. In addition to patient discomfort, there is a risk for bowel perforation with intubation, as well as the inherent risks of sedation. CT enteroclysis remains highly operator dependent and not widely available.
Small Bowel Computed Tomography Techniques
Abdominal and Pelvic Computed Tomography
Typical routine CT abdomen and pelvis protocols are optimized to evaluate both solid organs and bowel using positive oral contrast media. The technique can evaluate areas of bowel dilatation or narrowing and is especially helpful in distinguishing partial and complete small bowel obstructions, in which no distal oral contrast is identified in complete small bowel obstructions. Often, the transition point can be determined by change in bowel caliber coupled with distal bowel decompression in high-grade partial small bowel obstructions. The small bowel transit time is often increased in partial small bowel obstructions with associated dilutional effects in loops of bowel distal to the obstruction, secondary to mixing with increased fluid accumulated proximal to the obstruction. Thus, it may be helpful to increase the standard postingestion delay of 1 to 2 hours, to more accurately evaluate the entire small bowel in patients with clinical concern for bowel obstruction.
Although positive oral contrast media have the ability to readily distinguish bowel from adjacent structures, the inherent high density of the media makes it difficult to identify subtle bowel pathologic processes. Thus, the media rely on the structural changes in bowel, to recognize abnormalities. In addition, poor mixing of positive oral contrast and enteric debris can result in fillings defects that can manifests pseudolesions.
Computed Tomography Enterography
Neutral oral contrast is used in CT enterography, which is becoming the default modality for initial evaluation of the small bowel ( Figure 24-4 ). The technique allows for appreciation of bowel mucosal changes and ulceration, which are not readily appreciated on positive oral contrast examinations ( Figure 24-5 ). To optimally evaluate the bowel mucosal changes, the technique requires optimal bowel distention, neutral oral contrast, and appropriate phase(s) of contrast. Optimal bowel distention is achieved through slow administration of a large volume of a neutral oral contrast agent (1 to 2 L), including a 0.1% w/v barium sulfate solution (VoLumen, Bracco, Milan, Italy), water-methyl-cellulose solution, or polyethylene glycol. An optimal technique would require patients to abstain from solid foods for 4 hours before the examination, to prevent mistaking food debris from intraluminal pathologic processes. Many protocols split up the contrast bolus into thirds at 15- to 20-minute intervals with an additional 200 to 300 mL of water or neutral contrast ingested immediately before imaging. The bowel is imaged in the “enteric” phase at 45 to 50 seconds postcontrast with high-volume flow rate of intravenous iodinated contrast at 4 mL per second.
CT enterography can be performed as a single-phase or multiphase examination, depending on the indication. Single-phase examinations are often performed for evaluation of inflammatory bowel disease (IBD) at initial presentation and for acute exacerbations of IBD symptoms. Patients with IBD often present at a young age in the second or third decades of life and require multiple follow-up imaging examinations for evaluation of disease involvement, treatment response, acute or chronic symptoms, and complications. Thus, radiation dose is an important consideration for a population that often will be imaged early in life and continue to have numerous imaging examinations. Multiphasic CT enterography protocols often involve evaluation for mesenteric ischemia or occult gastrointestinal bleeding, both of which occur more often in older populations during acute events, for which multiple subsequent imaging evaluations are not often required. Mesenteric ischemia protocols are often performed in the arterial (25- to 30-second delay) and portal venous (65- to 70-second delay) phases, to evaluate the small bowel mesentery arterial and portal venous vasculature, respectively. Occult gastrointestinal bleeding protocols often image the bowel using a noncontrast phase to evaluate for hyperdense enteric contents that could be mistaken for blood products, followed by arterial, portal venous, and delayed (3 to 5 minutes postcontrast) phases, evaluation for intraluminal contrast that accumulates on delayed images.
Computed Tomography Enteroclysis
CT enteroclysis is the gold standard in CT of the small bowel. There are many indications, including low-grade small bowel obstruction, IBD, obscure gastrointestinal bleeding, and small bowel tumors. After nasojejunal intubation, a large volume of neutral enteric contrast medium is rapidly infused directly into the proximal jejunum by an infusion pump, followed by thin-section CT with intravenous contrast material. Compared with routine CT and CT enterography, the strength of this technique is the enteral volume challenge by nasojejunal intubation, which allows controlled rapid infusion of large volumes of enteric contrast material, thereby optimizing the degree and extent of small bowel distention ( Figure 24-6 ). It is also advantageous compared with capsule endoscopy because it allows evaluation of the entire abdomen and is not affected by small bowel obstruction, which is an absolute contraindication in capsule endoscopy. Because of the invasive nature of this examination, patients may require sedation. In addition to patient discomfort, there is a risk for bowel perforation with intubation, as well as the inherent risks of sedation. CT enteroclysis remains highly operator dependent and not widely available.