Fig. 1
Endorectal balloon filled with 40 ml air (left) and deflated (right)
QLrad B.V.®, Netherland: is made of silicon, filled with 80 cc of air resulting in a diameter up to 6 cm. The balloon is 3 cm long and fixed on a 20 cm shaft with stopper
E-Z-EM®, USA: is made of silicon, filled with 60–100 cc of air resulting in a diameter of up to 6 cm. The balloon is 4–5 cm long and fixed on a 15 cm shaft
Medrad®, USA: is made of latex, filled with 60–100 cc of air resulting in a diameter up to 4 cm. The balloon is 9 cm long and fixed on a 33 cm shaft.
2.2 Application and Patient’s Tolerance
The erB is enveloped with a condom sheath and the condom is lubricated, the ensheathed erB is carefully inserted into the anorectum and then inflated with air for the daily treatment. In case of proton therapy the balloon is filled with water. The balloon catheter is then pulled back, such that the balloon seats itself against the anorectal junction to ensure reproducible position and, in case a stopper is available, the stopper is adjusted. To minimize patients discomfort during erB application local anaestetic gel might be used. After radiotherapy is finished the erB is deflated and gently removed. The whole workload needs about 2–3 min setup time (Van Lin et al. 2005; Patel et al. 2003) per fractionation.
Within an Austrian–German multicenter trial, patients acceptance of the erB was analyzed in 429 patients. No major complaints were reported in 79 % of the patients and erB application had to be stopped due to pain in 4 % of patients only. Patients reporting acute rectal side effects experienced significantly more erB discomfort (Goldner et al. 2006). In another study, the number of treatments in which the erB was tolerated was recorded. 3,561 patients received proton irradiation of the prostate and seminal vesicles with or without X-ray treatment of the pelvis. Only 2.4 % of patients refused the erB for 1 or more treatments. A significant tolerance advantage (99.5 % vs. 95.7 %.) in those who received protons alone (= local) compared with combination treatment (local + pelvic) could be detected (Ronson et al. 2006).
2.3 Immobilization
It is expected that erBs reduce intrafraction and interfraction motion of the prostate and as a consequence CTV—PTV margins might be minimized. Intrafraction motion was investigated by (Wang et al. 2012) measuring real-time prostate motion in 29 non-erB patients and 30 erB patients. Large motion up to 1 cm was only detected in the non-erB group. Prostate motion increased as a function of treatment time for displacements >2–8 mm for the non-erB group and >2–4 mm for the erB-group. The symmetrical internal margin could be reduced from 5 to 3 mm for 6 min treatment time and beyond 6 min treatment time this margin could be reduced from 9 to 5 mm. They concluded that the erB reduced internal margin in almost all directions, especially in the anterior-posterior direction. Likewise (Smeenk et al. 2012) observed a significant treatment time-related reduction of intrafraction motion with the erB. Prostate motion for 15 patients with erB was tracked in real time using an electronic tracking system and compared to 15 patients without erB. Within the first 2.5 min prostate displacements were negligible. After 10-min treatment time, intrafraction motion of >5 and >7 mm was found in 0.7 and 0.3 % in the erB-group compared to 4.6 and 1.4 % in the non-erB-group. Again the largest reduction of displacement was found in the anterior-posterior direction. Analyzing repeated CT-images with one minute intervals (D’Amico et al. 2001) found a reduced maximum prostate displacement in any direction from 4 to ≤1 mm by the use of a erB. With regard to interfractional motion Wachter et al. (2002) were able to demonstrate that maximum displacements of the prostate larger than 5 mm in the anterior-posterior direction was reduced from 80 to 20 % by the use of an erB. However, other studies were not able to confirm that interfraction motion can be reduced by the application of an erB (Van Lin et al. 2005; El-Bassiouni et al. 2006). Van Lin et al. (2005) found no differences in systematic and random prostate motion and concluded that erB application did not reduce interfraction prostate motion.
2.4 Reproducibility
Several reports addressed the question of the reproducibility of the erB position and its impact on the dose distribution within the treatment volume as well as the organs at risk. During radiation therapy for the treatment of prostate cancer erB position and the impact position interventions was investigated. Manual adjustment of the erB based on information of cone-beam CT resulted in increased dose coverage (D95) from 94 to 98 % and increased the similarity in shape of the prostate to the radiotherapy plan (Jones et al. 2012). The authors concluded that image-guided interventions in erB volume and/or position during prostate radiotherapy are necessary to ensure the delivery of the dose distribution as planned (Jones et al. 2012). High variations in erB position are found mainly in the superior—inferior direction (Ahmad et al. 2005; Ciernik et al. 2003). Using an erB with a stopper on the shaft might minimize this setup variations. Due to potential setup variations reduced dose at the prostate and or seminal vesicles might be caused. Image guidance (Cone-beam CT or portal imaging verification) should be performed to verify and if necessary adjust erB position. In case erB application has to be stopped a new treatment plan has to be performed.
2.5 Radioprotection of the Rectum/Rectal Wall
Beside immobilization the erB might as well serve for radioprotection of the rectum. Within external beam radiotherapy, dose reduction up to 15 % at 1–2 mm depth might be produced due to the tissue–air interface (The et al. 2005, 2002) and as a consequence dose at the rectal wall might decrease. (Van Lin et al. 2007) were able to demonstrate that the rectal mucosal regions receiving a dose >40 Gy showed less severe teleangiectasia when an erB was applied. This might be caused due to the tissue–air interface and/or due to hypoxia within the rectal wall caused by stretching and therefore resulting in radioresistance. The dosimetric consequences and rectal wall sparing effect of an erB in prostate cancer radiotherapy was investigated in several studies. The anterior part of the rectal wall, adjacent the peripheral zone of the prostate, will inevitably be in the high-dose region due to the safety margin needed regardless of treatment technique. However due to distension of the rectum, at least the posterior part of the rectal wall can be pushed away from the prostate and the high-dose region (Figs. 2, 3). A comparative study of three types of erBs was performed by van (Van Lin et al. 2005). A significant reduction of rectal wall volumes exposed to >50 Gy and >70 Gy could be detected with all types of erBs in case of 3D-CRT (four-field-box technique). The larger the volume of the balloon, the more reduction of rectal wall exposure could be achieved. However, in case of the use of IMRT technique no significant difference could be detected. A significant reduction of relative rectal wall volume at the posterior wall could also be detected by Wachter et al. using a 40 cc air filled balloon (Wachter et al. 2002) within patients treated by a four-field box technique for localized prostate cancer. Whereas, no statistically significant difference was observed at the anterior rectum wall, and in case the PTV included also the seminal vesicles the advantage of posterior rectal wall sparing was lost. Using a 60 cc air filled balloon, a significant reduction of rectal wall volume exposed to >60 Gy was also found by Patel et al. including the seminal vesicles into the CTV (Patel et al. 2003). Patel et al. analyzed dose-volume histograms with an inflated or deflated balloon with both three-dimensional (3D)-conformal and intensity-modulated radiation therapy. The erB resulted in a mean fractional high-dose rectal sparing of 39 %. In addition they could demonstrate that the use of an erB with a 3D-CRT plan produced about as much rectal dose sparing as an image-guided IMRT plan without a balloon, and inclusion of a balloon with IMRT produced further rectal sparing (treatment plans with an erB in place are shown in Figs. 2, 3).
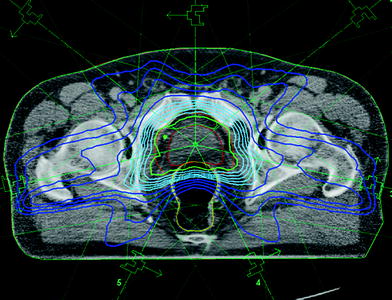
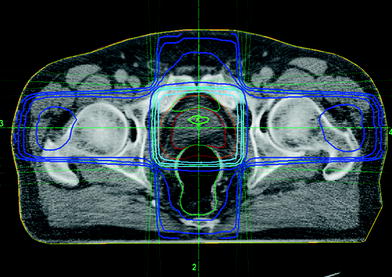
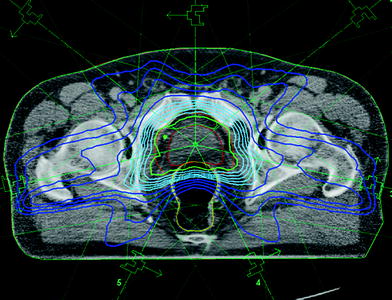
Fig. 2
Treatment plan: IMRT with endorectal balloon
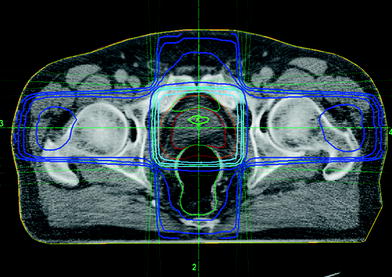
Fig. 3
Treatment plan: four-field box technique with endorectal balloon
2.6 Impact on Rectal Toxicity
Only one comparative study evaluating the impact of erB in regard of toxicity has been performed until now. Analyzing toxicity rates and endoscopic verified mucosal changes of the rectum (Van Lin et al. 2007) compared 24 patients with erB to 24 patients without erB within a prospective study treating patients up to 67,5 Gy. The acute urinary and rectal side effects were similar for the erB and non-erB group. Late urinary toxicity in both groups was mild with no Grade ≥3 and was comparable for both groups. Late rectal toxicity (Grade ≥1) was significantly higher for the non-erB group (5/24 vs 14/24 patients; p = 0.003) and rectal bleeding was detected in 13 % in the erB group compared to 33 % in the non-erB group (p = 0.17). A total of 146 endoscopies and 2,336 mucosal areas were investigated. Significantly, less high-grade telangiectasia was observed in the erB group at the lateral and posterior part of the rectal wall. However, Van Lin et al. concluded that longer follow-up and more comparative studies are necessary.
Toxicity data on dose escalation for localized prostate cancer patients compared 66–70 Gy and 74 Gy within one single institution. All patients were treated by four-field box technique using an erB. Including a total of 398 patients they reported on low rates of grade 3 rectal and urogenital toxicity (1, 5 and 3, 3 %) after a median follow-up of 64 months (Goldner et al. 2009). The same group reported on 178 primary prostate cancer patients treated within an Austrian–German multicenter trial by three-dimensional radiotherapy up to a local dose of 70 Gy or 74 Gy using an erB. After a median follow-up of 74 months the 5-year actuarial incidence rates for GI/GU grade ≥2 side effects were 19 and 23 % (Schmid et al. 2012).
2.7 Summary
The erB is used within daily prostate cancer radiotherapy in various departments. Intrafractional prostate motion seems to be reduced by the use of an erB. With regard to interfractional prostate motion not all reports were able to confirm a displacement reduction. However, position verification and correction protocols have still to be performed to avoid large variations. Radioprotection is discussed due to distension of the rectum, due to stretching of the rectal wall leading to hypoxia and due to the tissue–air interface. Endorectal balloons may therefore lead to reduced rectal toxicity. But further clinical comparative studies are necessary to confirm this hypothesis.
3 Rectal Spacer: Hyaluronic Acid (HA), Space OAR Gel, Biodegradable Balloon
Within the last years, different tools have been tested and implemented to reduce radiation of the rectum by increasing the spatial separation toward the prostate in order to reduce radiation dose even at the anterior rectal wall and as a consequence rectal toxicity. Morancy et al. reported within a small pilot study including three patients about injection of patient’s blood between the rectum and the prostate. However, only moderate separation was achieved and stability of distance lasted just for one week (Morancy et al. 2008). Hyaluronic acid, Space OAR gel, or biodegradable balloons are used to create a longer lasting protective distance to the rectal wall resulting in lower doses applied during the whole treatment course within external radiotherapy. The number of reports is limited but steadily rising. Most of these articles are dealing about applicability, stability, reduction of rectal dose-volume exposure, and impact on acute toxicity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree