Author
N
Setting
Response
PET response
TTP
OS
Comments
Bester
224
Refractory
NA
NA
NA
11.9 m
Comparative retrospective cohort study with BSC. Reduction of 43 % in the hazard of death for patients receiving RE. Overall incidence of RILD; 34 %
Martin
24
After a median of 3 prior lines of therapy
0 %
NA
3.9 m
8.9 m
54 % extrahepatic disease
67 % bilobar liver involvement
Gulec
15
Refractory
47 %
NA
NA
NA
Tumor response correlated with higher tumor flow ratio as measured by Tc-99m MAA imaging
Kennedy
208
87 % had received 3 lines of systemic therapy
35.5 % (SD; 55 %)
85 %
NA
10.5 m (vs. 4.5 m in nonresponders)
Table 2
Summary of studies with radioembolization as monotherapy in CRCLM
Author | N | Setting | Response | PET response | TTP | OS | Comments |
|---|---|---|---|---|---|---|---|
Mulcahy | 72 | Salvage | 40.3 % (SD; 44.5 %) | 77 % | 15 m | 14.5 m | Median dose delivered; 118 Gy. Liver replacement, ECOG, and extrahepatic disease correlated with outcome |
Sato | 51 | Salvage | 42.8 % (SD; 47 %) | 90 % | NA | 457 days | 90Y-glass microspheres. ECOG, tumor burden, number of liver metastases, and hypervascularity correlated with OS. Heterogeneous population |
Seidensticker | 29 | Refractory to L-OHP and CPT-11 | 41.4 % (SD; 17.2 %) | NA | 5.5 m | 8.3 m | Matched-pair comparison. RE increases median survival compared to BSC (8.3 vs. 3.5 months) |
Cosimelli | 50 | Refractory to L-OHP and CPT-11. 22 % prior bevacizumab | 24 % (SD; 24 %) | NA | 3.7 m | 12.6 m (2-year OS; 19.6 %) | 76 % > 4 lines of therapy, 58 % > 4 liver mets, 60 % >25–50 % of liver replacement. QoL not adversely affected by RE |
The proportion of patients alive at 12 months also varied from one study to another, ranging from 37 to 59 %. Progression-free survival also ranged from 3.9 to 9.2 months. These results suggest that up to 50 % of patients with CRCLM treated with 90Y-RE in the salvage setting are alive at 12 months after therapy. When survival data are compared for 90Y-RE as monotherapy, the shortest overall survival was reported by Seidensticker et al. (8.3 months), and the longest overall survival was reported by Sato et al. (15.2 months). However, comparison of these two trials is hard since one used resin-based spheres and the other glass-based spheres. There is also a lack of information regarding the median administered activity and the inclusion of a relatively large percentage of patients with extrahepatic disease (Cianni et al. 2009; Townsend et al. 2009; Nace et al. 2011).
From the previously outlined trials, it seems clear that great heterogeneity between different studies exist. Thus, the amount of extrahepatic disease and the acceptable tumor burden allowed to entry into the trials do not seem to be clearly outlined. The patients’ performance status (only reported in 50 % of the published articles) and the prognostic impact of previous systemic treatments (most studies on 90Y-RE as monotherapy include patients with a median of 3 or more prior lines) should also be further detailed. Finally, tumor response rate varies widely in these trials. This may be explained in part by differences in methodology for response assessment. Several trials do not specify whether RECIST criteria have been followed. Tumor response should be differentiated in target lesions, liver, and overall response. Moreover, in order to improve interpretability of overall response rates, studies should indicate whether patients have baseline evidence of extrahepatic disease (Rosenbaum et al. 2013).
3 Salvage Therapy Available Options in CRC Patients
Currently, a broad variety of trials and retrospective analysis in metastatic colorectal cancer patients have provided insight into the selection and duration of treatment, the role of targeted agents, and the best way to tailor therapy according to clinical and molecular parameters. Nevertheless, there remains a high medical need for effective treatments for patients with unresectable CRC liver metastases who have failed conventional chemotherapy regimens.
At present, 90Y radioembolization as monotherapy is provided mainly to patients with progressive disease after first- or second-line chemotherapy. In this setting of refractory disease other therapeutic alternatives have been tested. More specifically, three-targeted agents have provided a survival advantage over BSC.
Van Cutsem et al. (2007) compared the activity of panitumumab (a fully human monoclonal antibody directed against the epidermal growth factor receptor (EGFR) plus best supportive care (BSC) to that of BSC alone in 463 patients with metastatic colorectal cancer who had progressed after standard chemotherapy. Panitumumab significantly prolonged PFS. Objective response rates also favored panitumumab over BSC (10 % for panitumumab and 0 % for BSC). No difference was observed in OS, although cross-over was allowed.
Junker et al. (2007) randomized 572 patients who had colorectal cancer expressing immunohistochemically detectable EGFR and who had been previously treated with a fluoropyrimidine, irinotecan, and oxaliplatin to Cetuximab, an IgG1 chimeric monoclonal antibody against EGFR plus best supportive care (287 patients) or best supportive care alone (285 patients). Cetuximab treatment was associated with a significant improvement in overall survival (hazard ratio for death, 0.77) and in progression-free survival (hazard ratio for disease progression or death, 0.68). The median overall survival was 6.1 months in the cetuximab group and 4.6 months in the group assigned to supportive care alone. Partial responses for the cetuximab and BSC groups were 8.0 and 0 %, respectively. Quality of life was also better preserved in the cetuximab group, with less deterioration in physical function and global health status.
Finally, Grothey et al. (2013) randomized 760 CRC patients to receive placebo or regorafenib, an oral multikinase inhibitor that blocks the activity of several protein kinases such as VEGFR 1-3, Raf, Kit, and Ret. Median overall survival was 6.4 months in the regorafenib arm versus 5.0 months in the placebo group (p = 0.005), with an overall survival rate at 9 months of 38.2 and 30.8 %, respectively. Included patients in these trials were similar to those deemed eligible for 90Y radioembolization, withstanding their potential extrahepatic disease load. This suggests that in the appropriately selected patients (liver-dominant disease, acceptable disease burden, preserved hepatic function, and performance status) a longer overall survival may be expected form RE compared to current standard third-line treatment options. Nevertheless, prospective comparative studies evaluating survival, tumor response, and quality of life after 90Y-RE are warranted.
4 Predictive Factors of Outcome After 90Y-RE
Given the wide variety in tumor response rates and survival times, great effort is put into optimal patient selection through the identification of prognostic and predictive factors for 90Y-RE. Further on, availability of early information on the efficacy of the therapy during the first days after RE application would be highly appreciated as therapy may be intensified by means of further systemic therapy or combined locoregional approaches. This is particularly appealing since the regular staging of the patients by imaging is usually performed about 3 months after RE application. Unfortunately, so far, data on predictive factors for RE outcome are scarce.
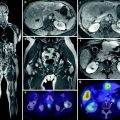
4.1 Imaging Predictive Factors
Dunfee et al. (2010) reported that the degree of radiological response, based on World Health Organization criteria, 1 month after radioembolization was a favorable prognostic marker. More recently, diffusion-weighted imaging was found to predict therapy response as soon as 2 days after RE application in a small study on 21 patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree