Infected Hip Prosthesis
Lana M. Rivers
Daniel B. Nissman
CLINICAL HISTORY
Patient with hip arthroplasty presents with ipsilateral hip pain, swelling, erythema, and fever.
FINDINGS
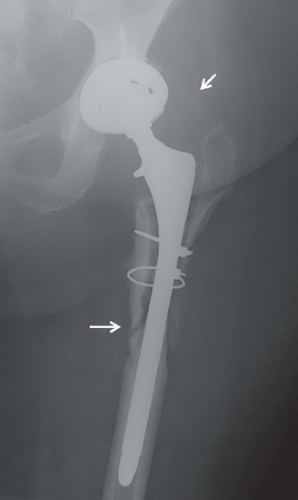
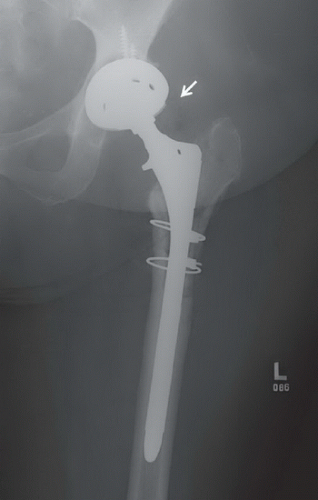
Anteroposterior (AP) view of the left hip (Fig. 12A) reveals a left total hip prosthesis with extensive lucency around the superior half of the femoral stem with an associated pathologic periprosthetic fracture (long arrow). AP view of the left hip from 1 year prior (Fig. 12B) reveals the same prosthesis with essentially normal supporting bone. Also note the large region of soft tissue density consistent with an effusion about the left hip in Figure 12A compared with Figure 12B (short arrow). (Images courtesy of Jordan Renner, MD, University of North Carolina, Chapel Hill, NC.)
DIFFERENTIAL DIAGNOSIS
Particle disease, Prosthetic loosening, Osteomyelitis/septic joint, subchondral cyst, lytic tumor.
DIAGNOSIS
Infected hip prosthesis.
DISCUSSION
Instability, aseptic loosening, and infection are the most common reasons for hip pain after arthroplasty leading to revision. Infection occurs in approximately 1% to 2%1 of first-time hip arthroplasties, and accounts for approximately 14.8%2 of all revision arthroplasties. Infection may occur through direct spread from adjacent soft tissue infection, surgical wound, or hematogenously from distant infection or transient bacteremia. Findings such as the presence of a sinus tract from the skin and elevated blood markers such as CRP, ESR, and WBC may aid the diagnosis. Patients most commonly present with pain in the hip region, including buttock, lateral hip, groin, or thigh pain. Fever, induration, or discharge may also be present. Infection around a hip arthroplasty is difficult to treat because the arthroplasty acts as a foreign body nidus upon which organisms can grow and disperse. In addition, prostheses have no blood supply and are impenetrable by antibiotics, as opposed to a native hip infection in which debridement/washout and intravenous antibiotics are able to contain an infection. It is therefore critical to recognize periprosthetic infection early to avoid undue bone loss and joint damage. Infection of a revision arthroplasty occurs at a higher rate, approximately 3.2% to 13%3, and findings are less predictable postrevision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree