Infection and Inflammation
Parenchymal Abscess
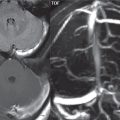
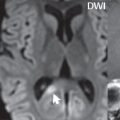
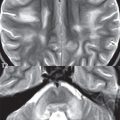
The typical appearance on MR and CT of a brain abscess is that of a round mass lesion with central necrosis, demonstrating a distinctive uniform thin rim of contrast enhancement. On T2-weighted scans, the abscess capsule may also demonstrate slight low signal intensity. There will be prominent accompanying vasogenic edema. The area of central necrosis may be heterogeneous. Although not entirely specific for an abscess (this finding can also be seen, rarely, in brain metastases), restricted diffusion on MR of the central fluid collection is characteristic for an abscess ( Fig. 1.90 ). The most common location is at the gray–white matter junction. Differential diagnostic considerations include a glioblastoma and a solitary necrotic metastasis. Glioblastomas, however, are typically much larger lesions, with the rim of contrast enhancement notable for its irregularity and of varying thickness.

Early in bacterial infection, prior to the formation of a distinct abscess, cerebritis will be present, with a somewhat nonspecific imaging appearance on MR. There will be focal vasogenic edema, with or without patchy contrast enhancement. Secondary findings may provide important clues to the diagnosis, including meningitis and lesion location (e.g., with the area of cerebritis adjacent to an infected frontal or mastoid sinus) ( Fig. 1.91 ).

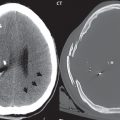
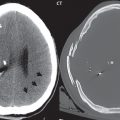
Epidural and Subdural Abscesses
MR is superior to CT for identification and definition of epidural and subdural abscesses, due both to its soft tissue sensitivity and the lack of artifact from the calvarium. In epidural lesions, close inspection should also be made of the adjacent bone for possible disease extension (osteomyelitis). On FLAIR, infected fluid collections, regardless of location, will have increased signal intensity, distinct from normal CSF (with very low SI). The displaced dura may be recognizable in epidural abscesses as a low signal intensity interface on a T2-weighted scan ( Fig. 1.92 ).

As with brain abscesses, DWI is invaluable, permitting differentiation of infected (with restricted diffusion) and sterile fluid collections. Abnormal contrast enhancement of the lesion margins will be seen, increasing conspicuity, but not entirely specific for infection. Use of fat saturation with post-contrast scans can markedly improve lesion depiction, and recognition of abnormal contrast enhancement, due to the suppression of high signal intensity in the fat of the diploic space and extracranial soft tissues. Recognition of adjacent osteomyelitis, accompanying an epidural abscess, is also markedly improved by the use of fat suppression, both on precontrast T2-weighted scans, and post-contrast. Depending on the location of a lesion, imaging planes other than the axial may markedly improve visualization of the lesion (e.g., coronal images in a lesion near the vertex), due to less partial volume imaging.
Meningitis
Common organisms responsible for bacterial meningitis in the general adult population include Streptococcus pneumoniae, group B Streptococcus, and Neisseria meningitidis. In the neonate, the common organisms are Escherichia coli, other gram-negative rods, and group B Streptococcus. Bacterial meningitis is rapidly lethal without treatment and, despite treatment, often complicated by infarction, sensorineural hearing loss, epilepsy, and intellectual impairment. CT is very insensitive to meningitis. On MR, FLAIR may demonstrate hyperintense signal, in areas of involvement, within sulci and cisterns, with this finding however nonspecific. Abnormal contrast enhancement occurs within the leptomeninges and any accompanying purulent exudate. Such an exudate may be present covering the cerebral hemispheres, along the base of the brain, and around the intracisternal segments of the cranial nerves. Imaging findings correlate with the severity of involvement. Mild cases of meningitis may have no abnormality on MR. Subdural empyemas can also be seen (with Streptococcus pneumoniae typically the organism), but are not common. Epidural empyemas are even less common. Diagnostic clues for a subdural or epidural empyema include restricted diffusion within the fluid collection and an enhancing rim. Sterile subdural effusions are also associated with meningitis. These however follow CSF on all MR pulse sequences.
Viral meningitis has no specific treatment, with most patients recovering on their own by 7 to 10 days. As with milder cases of bacterial meningitis, findings on MR may be subtle or the scan may be normal. Findings include mild leptomeningeal enhancement and loss of cortical sulci due to generalized mild brain swelling.
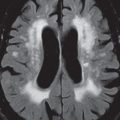
Ventriculitis
Ventriculitis is inflammation of the ependymal lining of a ventricle, and can be seen as a complication of meningitis, following surgery, or due to contiguous extension of infection. As with meningitis, findings on MR may be subtle or not present. CT is rarely abnormal. Two findings are characteristic for ventriculitis on MR: increased signal intensity within the immediate periventricular white matter on FLAIR and enhancement of the ependymal lining. Ependymal spread of neoplastic disease is the primary differential diagnosis, with nodularity (if present) favoring tumor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree