INFECTIOUS AND NONINFECTIOUS INFLAMMATORY DISEASES: LANGERHANS CELL HISTIOCYTOSIS
KEY POINTS
- Langerhans cell histiocytosis can be a localized or multisystem disease.
- Langerhans cell histiocytosis has important intracranial as well as extracranial manifestations, including presentations as an infiltrating leptomeningeal process.
GENERAL PATHOLOGY AND FORMS OF THE DISEASE
Langerhans cell histiocytosis (LCH) is a disease of antigen-presenting cell or dendritic cells that are present in the epidermis basal layers, bronchial mucosa, thymic epithelium, and lymph nodes.1
Due to recent advances in tumor and cell biology, the histiocytoses in general are now a better understood disease than just a decade or two ago. LCH is by far the most common of these uncommon diseases presenting in the head and neck region if the other rare dendritic cell and malignant histiocytoses that present mainly as adenopathy are excluded.
LCH presents itself in three general clinical settings that may overlap. These include (a) an acute, fulminating systemic disease in an infant or young child sometimes known as acute disseminated histiocytosis or Letterer-Siwe disease; (b) a chronic, disseminated, multifocal systemic disease in young children and occasionally adults that can result in organ dysfunction including diabetes insipidus, also known as Hand-Schüller-Christian disease or syndrome; and (c) a solitary focus of eosinophilic granuloma (EG) that presents as a lytic lesion of bone.1,2 There is some controversy as to whether these three entities represent a spectrum of the same disease.
There is definitely a pathologic spectrum of LCH that is linked to prognosis. Diffuse disease at presentation, decreased eosinophils in the histiocytic infiltrate, and visceral involvement are all linked to poor prognosis.3 The etiology of the disease is unknown. It is felt to be an aberrant immune response, probably to a viral antigen. It occurs in both immune-competent and immune-incompetent patients.
CLINICAL PRESENTATIONS
Head and neck manifestations of LCH are common at the time of presentation and are generally categorized into nodal and extranodal groups in addition to the localized, multifocal, and systemic disease with organ dysfunction categories just described.
Lymphadenopathy
As with other disease of the lymphoid/hematopoietic system, the disease will have nodal, extranodal, and medullary manifestations. Lymphadenopathy is a prominent component of LCH, especially in the acute disseminated cases.4 With that predominant or exclusive presentation, the disease must be distinguished histopathologically from the other much more common malignant and nonmalignant adenopathies.
Extranodal Disease
The extranodal manifestations of LCH are primarily of the bones of the skull and face and central nervous system (CNS).
Focal disease has a predilection for the temporal bone, especially the mastoid.5,6 As such, the presentation can mimic or be associated with chronic or subacute otomastoiditis, otitis externa, or a mastoid region mass (Figs. 19.1–19.4).7
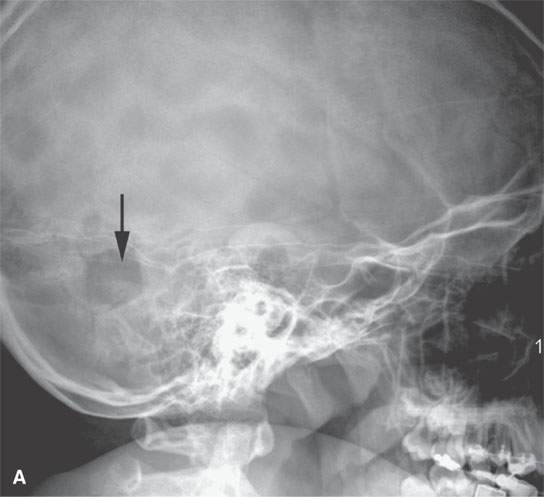
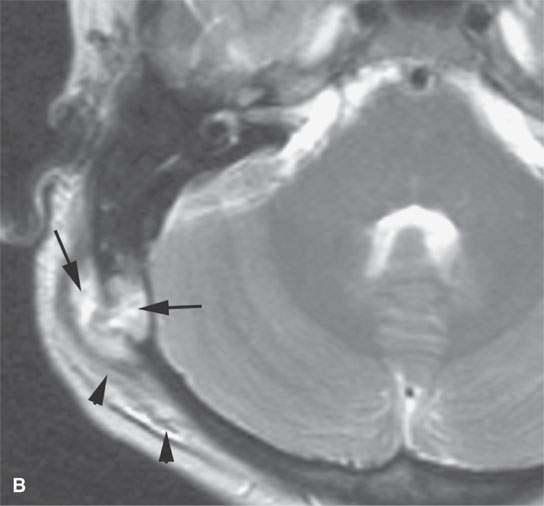
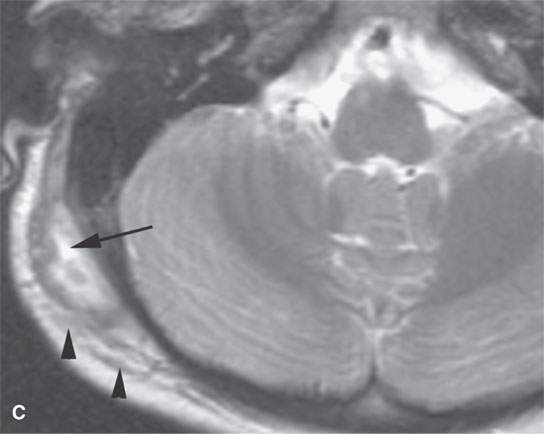
FIGURE 19.1. Eosinophilic granuloma of an early active lesion at the occipital mastoid suture presenting as a scalp mass the plain film in (A) showing it as a discreet solitary lytic lesion (arrow). T2-weighted images (B) and (C) show the lesion as high signal intensity relative to muscle and fat with spread to adjacent soft tissues and a moderate amount of surrounding edema (arrowheads).
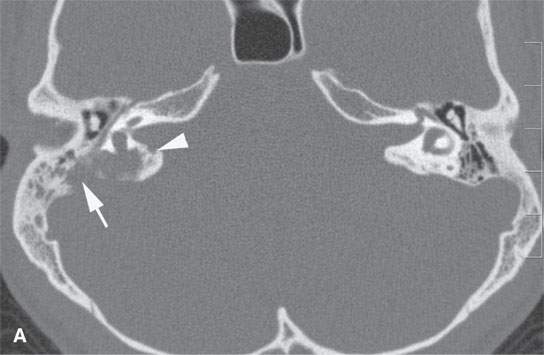

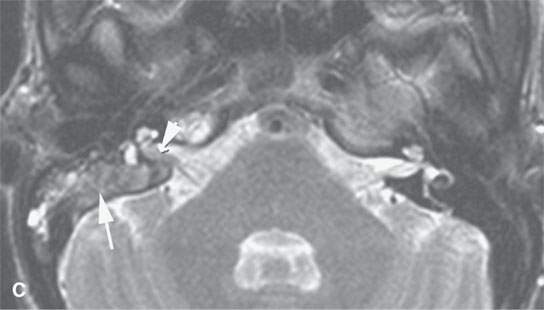

FIGURE 19.2. Eosinophilic granuloma (EG) of the petrous and mastoid portions of the temporal bone (arrows) filtering through the posterior wall of the internal auditory canal to involve the dura and encroach on the canal (arrowheads). A: Computed tomography shows the EG as purely lytic with sharp margins. B: Non–contrast-enhanced T1-weighted image shows the EG to be isointense to brain and muscle. C: T2-weighted image shows it to be intermediate to fat and muscle in signal intensity. D: Contrast-enhanced T1-weighted image shows it to enhance intensely.
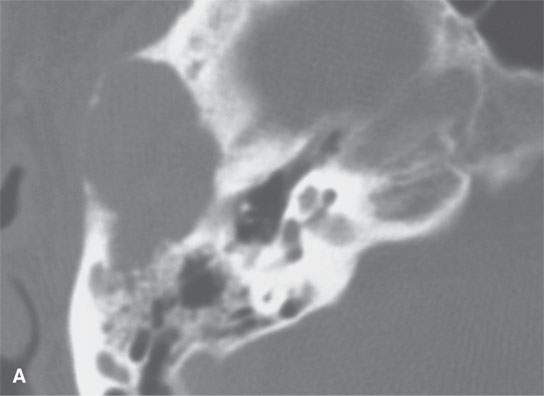
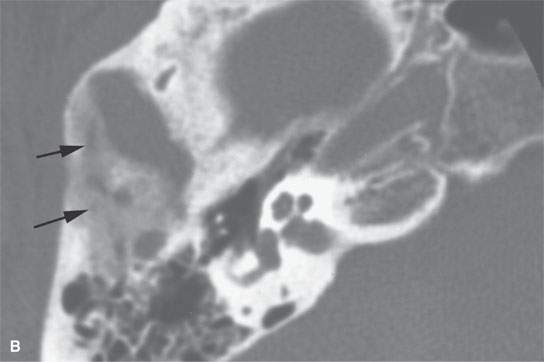
FIGURE 19.3. Eosinophilic granuloma of the temporal bone with computed tomography showing the early lytic lesion (A) and then evidence of healing with early reactive bone beginning to fill its more posterior aspect (arrows in B).

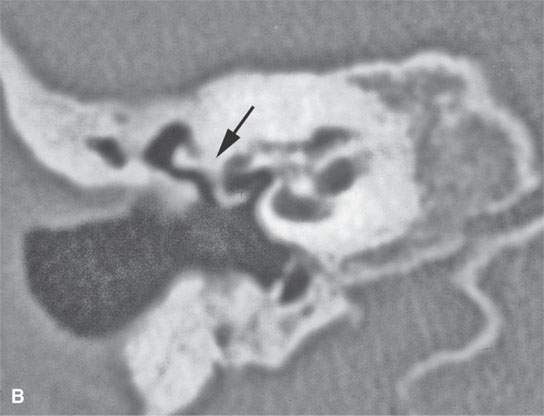
FIGURE 19.4. Healed eosinophilic granuloma with computed tomography showing general sclerosis of the temporal bone and resulting in ankylosis of the ossicles to the wall of the mesotympanum (arrows).
The mandible, orbits, cervical spine, and cranial vault are also frequent sites of involvement.8 A localized periorbital mass or one elsewhere of the face or calvarium is a very frequent presenting complaint most typically in the localized or multifocal forms of the disease (Figs. 19.5–19.7). Loose teeth and oral cavity subgingival or a mandibular mass is also a relatively frequent presentation.
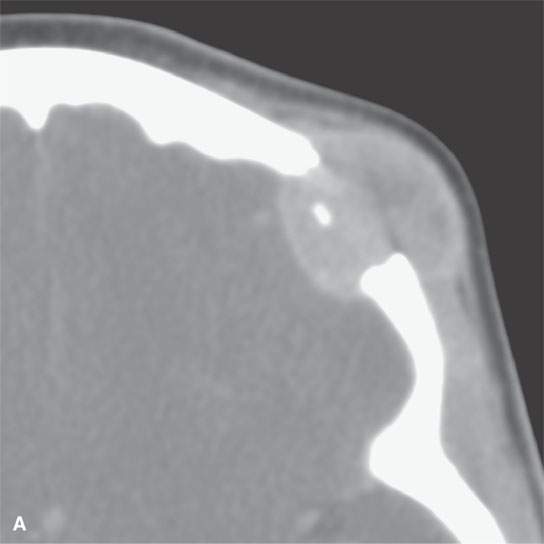
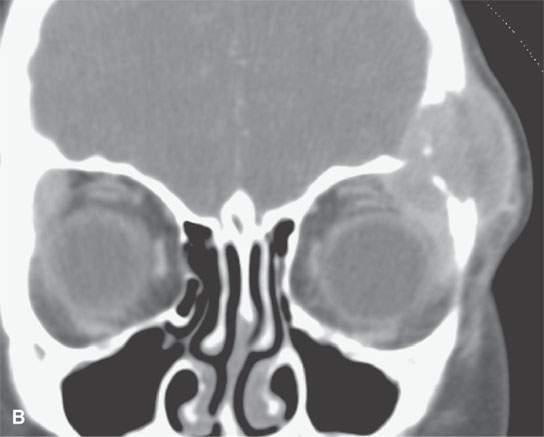
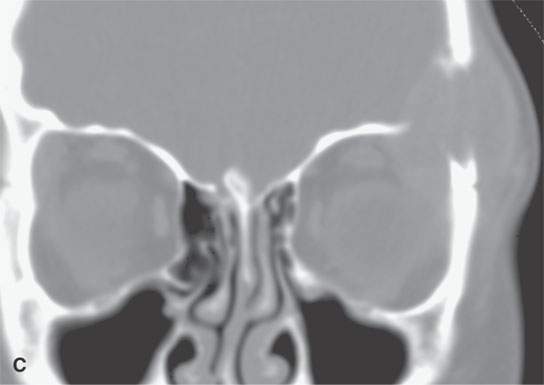
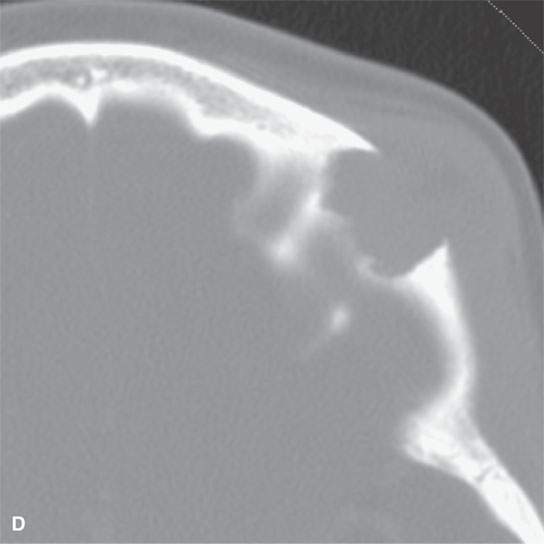

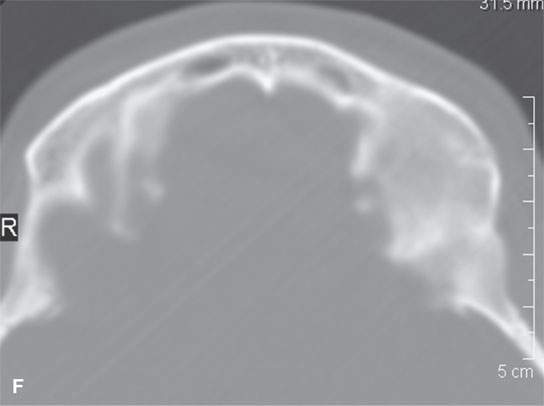
FIGURE 19.5. Eosinophilic granuloma of the frontal bone with (A), (B), (C), and (D) showing its lytic and enhancing properties, while (E) and (F) show it completely healed with residual sclerosis of the previously involved bone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








