Fig. 16.1
Graphical representation illustrating the availability of the imaging modality (number of people per device) versus the cost of purchasing the imaging scanner (in US dollars)
Thoracic Radiography
Plain film radiography is the most widely used imaging modality. One of the most common applications for radiographic imaging is in the diagnosis and monitoring of thoracic infectious disease, particularly pneumonia. Worldwide, pneumonia is a leading cause of death and hospitalization, particularly among children and the elderly [7]. In many instances the specific appearance or distribution of abnormalities on the chest radiograph due to infection can aid in identification of the involved pathogen, informing treatment and identifying complications and/or treatment response. Lobar consolidation, cavitation, and effusions often suggest a bacterial etiology (Fig. 16.2), but also can be seen in polymicrobial (i.e., multiple pathogens at once) infections in addition to fungal and mycobacterial etiologies; in the case of consolidation, pyogenic bacteria are commonly diagnosed [8]. Diffuse bilateral involvement may also be a presentation of bacterial pneumonia, but more often suggest an atypical infection, such as Mycoplasma, Pneumocystis jiroveci, Legionella, or a primary viral illness [8]. A chest radiographic appearance more severe than suggested by the clinical examination has been described in both viral and mycoplasma pneumonias [8]. Although specific pathogen diagnosis is often not possible by radiography given the overlapping imaging features of these diseases, radiography is important for (1) localizing the site of infection at diagnosis, (2) monitoring progression versus regression, (3) estimating severity, and (4) diagnosing complications such as pneumothorax and atelectasis (lung collapse). Therefore radiography is a vital tool for managing lung infections even when the specific pathogen is not identified, particularly since many antibiotic therapies can cover a wide range of the possible pathogens.


Fig. 16.2
Frontal chest radiograph demonstrating left lower lobe airspace opacities in a patient with community acquired pneumonia
Pneumatoceles (cavities filled with air) may be seen in pneumonia caused by Staphylococcus aureus, Klebsiella pneumoniae, Haemophilus influenzae, and Streptococcus pneumoniae [8]. Streaky peri-hilar shadowing can be an early stage of Pneumocystis jirovecii pneumonia (PCP), most often seen in HIV-infected patients [9]. In more advanced stages, PCP presents with a butterfly-shaped appearance or diffuse ground-glass opacities [10]. Other less common patterns have been reported, including lobar infiltrates, pulmonary nodules, pneumatoceles, and other cystic changes [10]. These diverse features of PCP are important to recognize in imaging because this is a common infection in HIV-infected patients and the treatment is different and longer term than the therapies for other lung infections.
An empyema is the term used to describe an infected fluid collection in the pleural space. This can occur primarily, but most commonly is attributable to a complication of pneumonia, previous surgery, or trauma [11]. The chest radiograph will classically demonstrate a large, lentiform (lens-shaped) pleural opacification [12] (Fig. 16.3). Pulmonary abscess, in contrast to an empyema, describes an infected collection in the lung parenchyma, and is often a complication of suppurative pneumonia that destroys lung parenchyma. The result is a pus-filled cavity, often demonstrating an air-fluid level on chest radiographs (Fig. 16.4) [13]. Similarly, Echinococcus granulosus, a cyst-forming tapeworm especially prevalent in parts of Asia, north and east Africa, Australia, and South America, can also present as a cavitary lung lesion, often containing smaller collections referred to as “daughter cysts” [12, 14]; Echinococcus infection also is seen to affect other areas of the body, most commonly the liver, as is discussed later in this chapter.



Fig. 16.3
Frontal chest radiograph demonstrating a large, lens-shaped opacity in a patient with an empyema as complication of community acquired pneumonia

Fig. 16.4
Frontal chest radiograph reveals a localized, walled cavity, with an air-fluid level in the left mid-lung compatible with an abscess
Another endemic parasitic infection commonly diagnosed on chest radiographs, Paragonimiasis, also leads to the formation of aggregate pulmonary cystic lesions. The disease is most prevalent in populations of Asia (Korea, Japan, Taiwan, central and southern China, and the Philippines) as well as Mexico and South America (Brazil, Costa Rica, Honduras) [15]. Since 2001, the number of new cases of paragonimiasis has alarmingly increased in much of coastal Asia and Japan, and has emerged as a significant public health issue [16]. Some of those with Paragonimus infections are symptom free and unaware of their infection, others develop a chronic cough and chest pain, classically describing “chocolate-colored” sputum [15]. Hemoptysis can often occur irregularly and continue for years. The chest radiographic appearance has been shown to vary with the stage of infection, however most commonly demonstrates focal mass-like consolidation containing aggregated thin-walled cysts (Fig. 16.5). The radiographic appearance can make differentiation of pleuropulmonary Paragonimus and TB difficult in areas of the world where both infections are endemic; differentiation may require sputum or lesion tissue pathologic examination [17]. The lifecycle of this species of trematode predicates maturation to adulthood in snails and other shellfish and subsequently infects humans via ingestion due to poor water sanitation or undercooked seafood. The eggs hatch in the gastrointestinal tract and larvae migrate throughout the body, mainly to the lungs and pleural cavity to continue the life cycle.
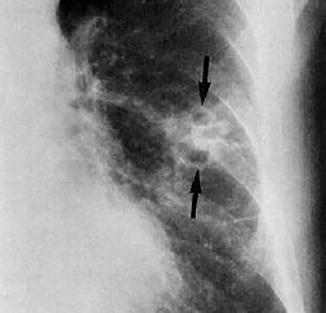
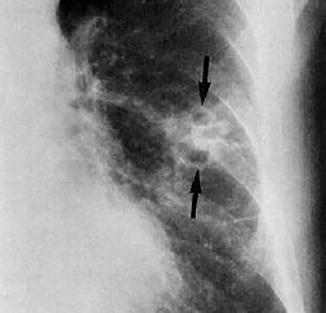
Fig. 16.5
Focal view of a left mid-lobe lesion demonstrating multiple small aggregated cysts in a patient with Paragonimus (arrows)
Of all the infectious diseases, Mycobacterium tuberculosis deserves special mention due to the widespread nature of the infection, communicability, increasing resistance to treatment, and its long-term morbidity/mortality. According to the World Health Organization, one third of the world’s population is thought to have been infected with M. tuberculosis (latent infection), with new infections occurring in about 1 % of the population each year [18]. According to the 2013 WHO report on tuberculosis (TB), there were an estimated 8.6 million new cases of active TB and 1.3 million deaths, mostly occurring in developing countries [18]. There are increasing rates of TB in Africa and Eastern Europe, and it is currently the leading cause of death in HIV-infected patients. Diagnosis of active TB relies on imaging, as well as microscopic examination and microbiological culture of body fluids, while the diagnosis of latent TB relies on the tuberculin skin test (TST) and/or blood tests. Unfortunately, the acid-fast bacilli are found in the sputum in a limited number of patients with active pulmonary TB. Therefore the imaging diagnosis provides rapid diagnosis for appropriate therapy before the definitive diagnosis by bacteriology. It is thought that more than 50 % of infected patients remain undiagnosed, and lack of access to medical care, particularly medical imaging such as chest radiography, presents a significant barrier to diagnosis and disease monitoring [19]. Treatment is difficult and requires administration of multiple antibiotics, many of which are expensive, over a long period of time (i.e., greater than 6 months). Antibiotic resistance is a growing problem in multi-drug resistant TB (MDR-TB) infections.
TB can have a wide variety of radiographic appearances and thus has been termed “the great imitator.” There are three classic appearances of pulmonary TB on chest radiographs: primary, reactivation (or secondary), and miliary. Primary TB occurs most commonly in children but is being seen with increasing frequency in adults and presents with lymph node enlargement, often unilateral hilar nodes, seen in 90–95 % of cases [20]. Other imaging findings in primary pulmonary TB range from a simple pleural effusion to poorly defined opacification in the peripheral lung fields [21]. In contrast, the most common radiographic manifestation of reactivation pulmonary TB is focal or patchy heterogeneous consolidation involving the apical and posterior segments of the upper lobes and the superior segments of the lower lobes. Another common finding is the presence of poorly defined nodules and linear opacities, which are seen in approximately 25 % of patients [20]. Cavities, the radiologic hallmark of reactivation TB, are evident radiographically in 20–45 % of patients (Fig. 16.6) [19]. Finally, in cases of miliary TB, the chest radiograph may demonstrate characteristic innumerable 1- to 3-mm diameter nodules randomly distributed throughout both lungs; thickening of interlobular septa is also frequently present [15, 20] (Fig. 16.7).



Fig. 16.6
Frontal chest radiograph demonstrating bilateral upper lobe asymmetrical cavitation. Note that the presence of pulmonary cavitation is evidence of necrosis, which is part of the natural history of disease

Fig. 16.7
Frontal chest radiograph demonstrating diffuse bilateral reticulonodular opacities in a patient with miliary pattern of TB infection
Melioidosis, a deadly gram-negative bacterial infection found primarily in Southeast Asia, can also cause a TB-like pattern of disease [15]. Pulmonary involvement is reported to be the most common form of melioidosis, accounting for >50 % of cases. Melioidosis is often first noted on chest radiographs [22, 23] and can be easily confused with TB. A high index of suspicion is therefore required to make this diagnosis. In acute, nonsepticemic, pneumonic melioidosis, the most common radiographic pattern is focal consolidation with or without cavitation. As might be seen in primary TB, melioidosis typically begins in the upper lobes, often quickly spreading to other lobes and forms nodules or patchy densities. Compared to TB, rapid clinical and radiographic progression with early cavitation favors melioidosis; hilar adenopathy is rarely seen in melioidosis [15].
Plain film radiography is most frequently utilized to examine the chest/lungs, but is also often used to examine the airway and soft tissues of the neck. Epiglottitis, a potentially life-threatening condition of inflammation, edema, and obstruction of the epiglottis and surrounding structures that classically occur in children aged 3–7 years, has a characteristic appearance on lateral radiographs of the neck known as the “thumb sign”—an enlarged epiglottis that protrudes from the anterior wall of the hypopharynx (Fig. 16.8) [11], thereby causing obstruction of the airway (either partially or entirely). Like epiglottitis, retropharyngeal abscess is also a potentially life-threatening condition due to the risk of compromising the airway [8], and carries significant morbidity and mortality if not managed properly [24]. Because of the deep location within the neck, this condition is difficult, if not impossible, to evaluate on clinical examination [25], which is why imaging techniques are critical. A lateral soft-tissue radiograph of the neck (during inspiration and with the neck in normal extension) may show widening of the prevertebral tissue [8].


Fig. 16.8
Lateral cervical radiograph demonstrates a markedly thickened epiglottis (arrow) in a patient with epiglottitis
Abdominal Radiography
Just as radiography is invaluable in the evaluation and diagnosis of thoracic infectious diseases, it can also be an excellent tool, for intraabdominal infections. In general, abdominal radiographs are particularly useful for demonstrating bowel obstruction or ileus, pneumatosis (air in the bowel wall), free intraperitoneal air, abscesses, etc. [26]. At times, severe gastrointestinal infections, caused by bacterial, viral, or parasitic disease can lead to dilation, ischemia, and perforation of the gastrointestinal tract; these complications are often readily demonstrated on abdominal radiography. Abdominal radiographs may also demonstrate the sequela of severe cholecystitis by demonstrating air within the lumen or wall (though ultimately for hepatobiliary examination ultrasound remains the initial study of choice) [14]. Finally, calcified processes in the abdomen, in particular the genitourinary and hepatobiliary system, can also be evaluated by plain film radiography.
In general, a large number of endemic infectious and parasitic diseases can lead to findings on abdominal radiography and may be useful in settings where more advanced imaging such as CT or ultrasound are not available. One of the most common and insidious endemic infectious diseases throughout Southeastern Asia, Coastal South America, and Africa is Schistosomiasis; which has a characteristic imaging appearance on abdominal radiography. In endemic areas, children are usually exposed early in life and in fact in some areas childhood infection is almost universal. For instance, in Niger (West Africa) over 80 % of children are infected and in rural Zambia the rate is nearly 70 % [15]. The abdominal radiographic findings involve the genitourinary (GU) system where calcification within the bladder and ureters are seen (Fig. 16.9); in severe infections the calcified eggs can be visualized in the soft tissues. In general, the kidneys are uncommonly calcified, and even in advanced disease, will be calcified out of proportion to the ureters and bladder [27].


Fig. 16.9
AP radiograph of the pelvis demonstrating thick circumferential calcification of the bladder and distal ureters, which are dilated in a patient with longstanding Schistosomiasis infection. A large calcified bladder stone is also present
TB, which can be found in nearly every part of the body, can also be identified on abdominal radiographs. As in other endemic infections, the GU tract is commonly involved. Differentiation from other causes of calcification, such as in Schistosomiasis, is often possible only in the later stages of the disease(s). For example, in Schistosomiasis calcification is first seen in the lower end of the ureters and the bladder and then extends up the ureters. In TB, the calcification extends down the ureters and the bladder, affecting the kidney much more often (Fig. 16.10) [28].


Fig. 16.10
AP radiograph of the pelvis demonstrating multiple dense calcifications replacing much of the right kidney as a result of late stage renal tuberculosis infection. This appearance is also referred to colloquially as “putty kidney”
Radiographs, in combination with administration of oral contrast agents (such as barium sulfate) can be used to evaluate the entire gastrointestinal tract. Drawbacks of these imaging examinations are that both availability and relatively high cost associated with contrast agents may be limiting in many parts of the world. Further, although CT would be the modality of choice in regions of the developed world, the limited availability of CT and the limited number of trained radiology professionals creates barriers to diagnosing infectious diseases with these techniques. As a result, radiographic and fluoroscopic examinations may still be useful in settings where resources for advanced imaging, such as CT, are limited.
Enterography, including barium esophagram, can identify complications of infections such as Chagas’ disease (American trypanosomiasis) which can present with severe esophageal dysfunction [29]; Trypomastogotes, the differentiated offspring of the parasite, tend to invade the esophagus and give rise to a megaoesophagus and/or achalasia (Fig. 16.11), which can be visualized with a lateral radiograph during a barium contrast esophagram [29]. Interestingly, Chagas’ disease can also cause dilation of other segments of the gastrointestinal tract, particularly the proximal small bowel and the colon in severe cases, and can also be diagnosed with barium contrast enterography [29].


Fig. 16.11
Lateral two view barium esophogram demonstrating marked esophageal dilation with characteristic “beaked” appearance near the gastroesophageal junction in a patient with Chagas’ disease
Intestinal parasitic infections with roundworms are exceedingly common in many parts of the world. In fact, it is thought that a considerable percentage of the world’s population (perhaps as high as 23 %) harbor various species of roundworms [15, 30]. Infection due to Ascaris (termed Ascariasis) is acquired by ingesting contaminated water or food that contains embryonated eggs. Numerous investigators have observed that the highest rate of infection with Ascaris is in children between 1 and 15 years of age. In hot and humid areas of rural Africa, Asia, and Latin America, up to 93 % of all inhabitants in some villages may be infected [15, 18, 28]. While the diagnosis is mainly dependent on examination of stool samples barium contrast agents are helpful in evaluating the presence of roundworm infection in the gastrointestinal tract (Fig. 16.12). in heavily infested patients, large collections of ascarids can frequently be identified on abdominal radiography without oral contrast [15, 27, 30]. In fact, large masses of worms in the bowel are best seen as a tangled group of thick cords and sometimes produce a “whirlpool” effect (Fig. 16.13). It is important to keep in mind the epidemiology of the region, as the differential diagnosis for an intraluminal worm identified by imaging is relatively nonspecific, and can also represent a variety of other parasitic worm infections or non-infectious etiologies. note that other worm infections, such as hookworms (A. duodenale and/or N. americanus), whipworms (T. trichiura), and capillariasis (C. philippinensis), are typically characterized on enterography by the inflammation or other changes in the bowel rather than direct visualization of the worms themselves due to their small size (10 mm on average in the case of A. duodenale). Stool examination and evaluation for worms and/or ova are diagnostic.



Fig. 16.12
Barium examination of the stomach clearly demonstrates the outlines of individual ascarids (worms) as elongated radiolucent filling defects within the barium column

Fig. 16.13
AP abdominal radiograph demonstrates a large bolus of worms in the cecum causing intestinal obstruction, manifest as thick tangles of cords within the air-filled large bowel
Extremity Radiography
Radiographs are invaluable in the workup of skeletal abnormalities. Even in the setting of advanced imaging such as CT and MRI, radiographs of the affected bone are a useful first step that may reveal other diagnoses, such as metastases, fractures, or other metabolic and systemic bone diseases. In the setting of osteomyelitis, radiography usually does not demonstrate significant abnormalities until roughly 50 % of the bone mineral content has been lost due to the infection [31]. The most common pathogens in osteomyelitis depend on the patient’s age; however, Staphylococcus aureus is the most common cause of acute and chronic pyogenic hematogenous osteomyelitis in both adults and children. Atypical endemic infections can also involve the musculoskeletal system and, in certain cases, have characteristic imaging appearances which aid in making the correct diagnosis.
One of the most notorious, and stigmatized, infections in the developing world is leprosy, a chronic and debilitating infection caused by Mycobacterium leprae, which often in late stages dramatically manifests as skeletal changes. There are an estimated one million patients with leprosy in the world, and while radiology is not often necessary for an initial diagnosis, imaging does play a vital role in assessing the activity and extent of the disease, and in helping to plan surgery and rehabilitation [15, 32]. The highest prevalence is in India and tropical Africa and South America; it also still occurs frequently in Southeast Asia, the Philippines, southern China and southern Malaysia, Indonesia, and some of the South Pacific islands [15, 32]. Leprosy presents in many different ways, both clinically and pathologically, but generally is divided into two different types: tuberculoid leprosy and lepromatous leprosy. Primary skeletal changes are most frequent in lepromatous leprosy, and the bone findings are essentially destructive patterns with very little surrounding bone reaction or sclerosis until healing occurs [15, 32] (Fig. 16.14). The disease is often diagnosed clinically (symptoms, physical exam, and history), and radiographs are most commonly utilized to monitor complications of the infection, including secondary pyogenic osteomyelitis due to the ulceration and neuromuscular changes of the infection in the extremities.


Fig. 16.14
Lateral radiograph of the foot demonstrates the final stages of leprosy characterized by the large areas of bone absorption. As the talus disintegrates, with weight-bearing, there is complete disruption of the foot, leaving the patient vulnerable to secondary infections which, in combination, leaves little normal anatomy or function
Musculoskeletal involvement of Taenia solium (cysticercosis) infection can be readily diagnosed with radiography because the appearance is pathognomonic. Cysticercosis is acquired by ingesting food, water, or feces containing eggs of T. solium. The oncospheres (larvae) are released from their shells in the gut and invade throughout the body, developing into cysticerci, most commonly in the skeletal muscles and brain [15, 33]. calcified lesions have been demonstrated in up to 97 % of patients examined 5 or more years after infection and can be easily demonstrated by soft-tissue radiography of the extremities [15] (Fig. 16.15).
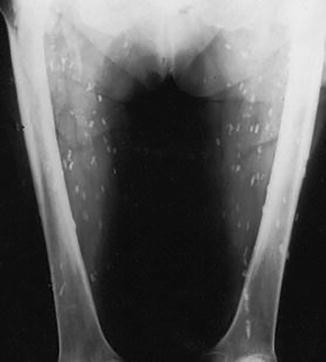
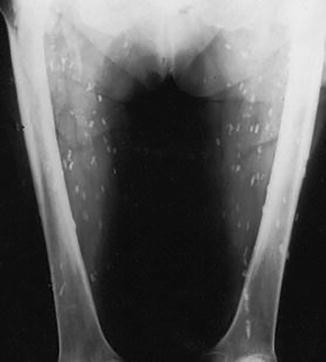
Fig. 16.15
Plain film AP radiography of the bilateral femurs. Cysticercosis infection manifesting as calcifications in the soft tissues and muscles of the lower extremities. The calcified cysticerci are aligned with their long axes in the plane of the muscle bundles of the legs
Another common and longstanding musculoskeletal endemic infection is Guinea Worm (Dracunculias medinensis); the infection by this nematode and the primitive treatment have been described as far back as 1550 bc, referenced first in the Ebers papyrus, and still retains significant cultural and mythical significance. For example, it is believed that the caduceus, the symbol of the medical profession, is derived from the guinea worm, since the worm was for centuries removed from subcutaneous tissues by winding it around a small stick, twisted slightly more each day until the entire worm was removed. In the mid-twentieth century it was estimated that over 48 million people in Africa, India, Arabia, the Middle East, and parts of Asia were infected [15, 34]. After 2000, it is thought that most areas of infection are in tropical Africa due to the success of the massively scaled multinational and multiorganization initiative (including WHO, UNICEF, CDC, and the Carter Center’s Global 2000 Program) to eradicate the infection [34]. The live guinea worm will not be identified radiologically as it lies near the skin surface and is radiopaque. After its death, however, the guinea worm often calcifies, particularly when entrapped within the subcutaneous tissues or muscle, and can be readily identified on radiographs of the extremities (the typical locations in the lower extremities) as a long serpiginous calcification [15] (Fig. 16.16).


Fig. 16.16
AP radiograph of the right femur demonstrating several calcified worms in the overlying soft tissues. This is the classic type of calcification seen in guinea worms in the extremities
Cardiac Ultrasound
Like radiography, ultrasound imaging is less expensive with higher availability in comparison to CT and MRI. Additionally, ultrasound does not use ionizing radiation. It is especially useful in diagnosing the complications of various cardiac, hepatobiliary, renal, and gonadal infections. Ultrasound is also extensively used to evaluate the neonatal brain and often useful in the diagnosis of ventriculitis [29, 35].
Ultrasound imaging of the heart (or “echocardiography”) is an essential tool to assess the heart and blood vessels and can provide both anatomic as well as functional information such as cardiac function and blood flow. [36]. We devote a separate chapter to cardiac imaging in this text, but cover some infectious disease issues in this section. For example, Endocarditis is an infection of the endocardium, which lines the inner surface of the heart and has varying etiologies, and heart valves [37]. When available, transoesophageal echocardiography (TEE) is the study of choice because of higher sensitivity compared with the transthoracic route (TTE) [38]. Echocardiography is also very useful in assessing rheumatic heart disease—a disease still prevalent in the developing world. It is triggered by certain strains of group A β-haemolytic streptococci, typically after a bout of pharyngitis and affect children, adolescents, and young people during their most productive years [39, 40]. Echocardiography typically shows mitral or aortic valve regurgitation [39]. Unlike endocarditis, the cause of myocarditis is not identified in most cases [41]. While viruses are the most common causes in the developed world, a broader range of pathogens are involved in developing countries; these include parasitic infections, such as Trypanosoma cruzi (Chagas’ disease) in South America, and disseminated infections in immunocompromised patients, such as Toxoplasma, Aspergillus, and Cryptococcus spp. [41]. Although unable to delineate the etiology, echocardiography is able to demonstrate cardiac function and can be used to track the progression of disease [41]. Similarly, echocardiography is useful to assess pericardial effusions (Fig. 16.17) and pericarditis [29] which can be viral, bacterial, or due to TB.
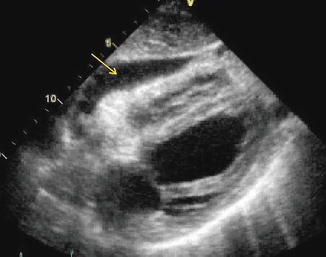
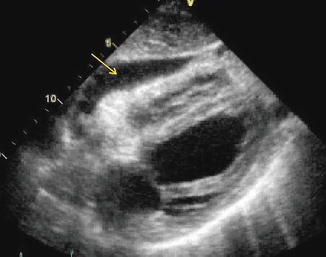
Fig. 16.17
Transthoracic echocardiogram image demonstrates hypoechoic pericardial fluid in a patient with a pericardial effusion due to TB (arrow)
Abdominal Ultrasound
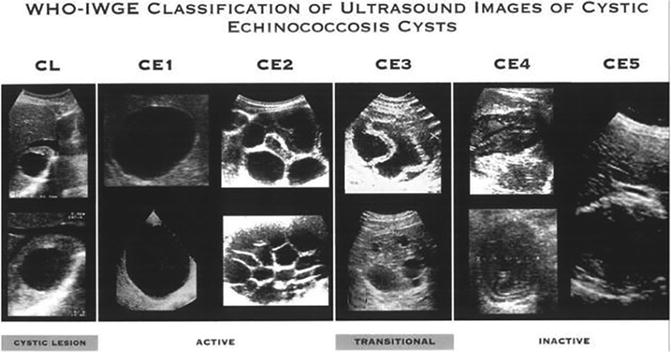
Ultrasound imaging is an excellent modality for assessing abdominal organs, especially the liver and hepatobiliary system. One of the most common hepatobiliary infections in the world is Echinococcosis or hydatid disease (most commonly E. granulosus), which is a small tapeworm whose lifecycle involves dogs as definitive hosts and sheeps, pigs, goats, horses as intermediate hosts; humans become inadvertant intermediate hosts after ingestion of the eggs excreted by infected dogs. The hatched larvae travel to the liver where they form fluid filled hydatid cysts. Over time daughter cysts may develop. In addition, an inflammatory granulomatous and/or fibrotic reaction may also occur [42]. The infection is endemic worldwide, with the highest prevalence in sheep-raising communities. Becasue of the wide prevalance, hydatid liver disease must be considered in the differential diagnosis of a cyst or mass in virtually any patient who is residing in, or has traveled through, an endemic area [15]. Ultrasound is highly helpful in the diagnosis/classification of hydatid liver disease and a grading scale has been developed by the WHO [43] (Fig. 16.18). While MRI is increasingly being used in the advanced health systems, ultrasound of the liver remains the most cost-effective and available in the developing world. However, ultrasonography is not always able to differentiate hydatid cysts from tumors or liver abscesses and additional imaging, such as CT or MRI, may be required.