Fig. 5.1
The development of erosive disease and synovitis in rheumatoid arthritis
The advent of new treatments for RA (termed “biologics”) in the late 1990s along with a more intensive approach to control of inflammation – the so-called treat-to-target approach – has revolutionised the management of RA, and outcomes continue to improve with fewer erosions, less deformity and improved functional ability.
The 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) classification criteria describe the diagnosis of definite RA based on joint involvement, including pattern and duration of swollen or tender joints (which may be confirmed by imaging evidence of synovitis), inflammatory markers, and RF and ACPA serological tests (Table 5.1).
Table 5.1
ACR/EULAR 2010 classification criteria
Target population: Patients who have at least 1 joint with definite clinical synovitis; with synovitis not better explained by another disease | |
Classification criteria | Score |
Joint involvement (any swollen or tender) | |
1 large joint | 0 |
2–10 large joints | 1 |
1–3 small joints | 2 |
4–10 small joints | 3 |
>10 joints (at least one small) | 5 |
Serology | |
Negative RF and negative ACPA | 0 |
Low-positive RF or low-positive ACPA | 2 |
High-positive RF or high-positive ACPA | 3 |
Acute phase reactants | |
Normal ESR and normal CRP | 0 |
Abnormal ESR or abnormal CRP | 1 |
Duration of symptoms | |
<6 weeks | 0 |
>6 weeks | 1 |
Score ≥6 = definite RA | |
Presentation
RA has a propensity for women with a female–male ratio of 3:1, with women particularly affected in their 40–60s. There is a genetic component with a modest familial predisposition to the disease – for example, in monozygotic twins, there is a concordance of around 7 %. Up to 70 % of Caucasian patients with RA have the gene encoding for HLA-DR4 or DR1 (the so-called shared epitope). In addition, environmental factors associated with the development of RA include cigarette smoking, obesity and exposure to silica dust and air pollution increasing the risk, while alcohol and the use of the oral contraceptive pill seem to reduce the risk. The small joints of the hands and feet are particularly commonly affected, but any synovial joint can become involved.
Symptoms at onset include the following:
Pain and swelling in the synovial joints
Morning stiffness lasting more than 1 hour
Fatigue
Diagnosis depends on a combination of factors including more than 6 weeks of tender or swollen joints (a homunculus is a convenient method of documenting tender and swollen joint counts; Fig. 5.2), a raised inflammatory response and a positive rheumatoid factor or anti-CCP (or ACPA) antibody test (Table 5.1).
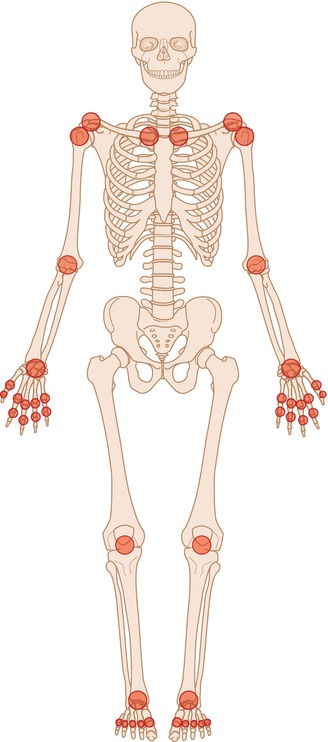
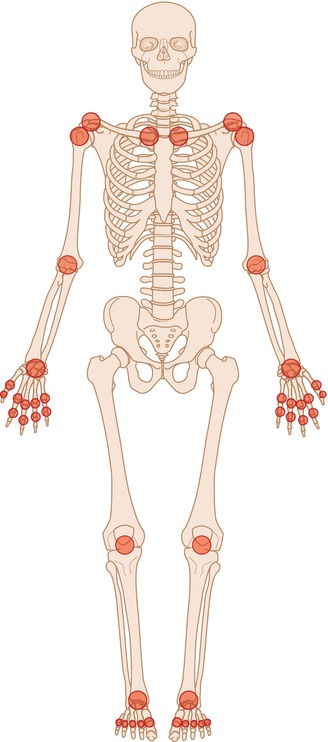
Fig. 5.2
Homunculus used to depict location of swollen and/or tender joints. The affected joints are marked off – usually two are used, one for swollen joints and one for tender joints
Imaging changes are not part of these initial classification criteria, although plain radiographs are usually performed at baseline to aid with diagnosis, assess radiographic severity of the disease and serve as a useful baseline for comparison with follow-up studies. Furthermore, both MRI and US are often used to delineate synovitis, effusion and erosions in a patient with questionable swollen joints on clinical examination at presentation.
A plain chest radiograph is essential prior to commencing pulmonary toxic drugs like methotrexate and prior to commencing biologic drugs as these have a propensity to reactivate covert mycobacterial infections.
In addition to baseline assessments, plain radiographs of the affected joints, US and/or MRI, can be used to monitor the progression of disease and response to treatment.
A recent position statement has been published from EULAR with recommendations for imaging in RA. The recommendations include evidence for imaging in diagnosis, comparison with clinical examination alone, detection of damage, prediction of therapeutic responses and monitoring disease activity and progression and remission. These recommendations are summarised in Table 5.2. They particularly address the additional utility of MRI and US:
Table 5.2
EULAR recommendations for the use of imaging in rheumatoid arthritis
Recommendation | Strength of recommendation (0–10 scale –0 = not recommended; 10 = highly recommended) | Level of evidence |
|---|---|---|
1. When there is diagnostic doubt, CR, US or MRI can be used to improve certainty of diagnosis | 9.1 | III |
2. Inflammation seen on US or MRI can be used to predict progression to clinical RA from undifferentiated inflammatory arthritis | 7.9 | III |
3. US and MRI are superior to clinical examination in detecting joint inflammation | 8.7 | III |
4. US and or MRI should be considered if CR does not show damage and may detect damage at an earlier time point – especially in early RA | 9.0 | IV |
5. BME on MRI is a strong independent predictor of subsequent radiographic progression in early RA. Synovitis on MRI or US, and erosions detected by CR, MRI or US could be used as prognostic indicators | 8.4 | III |
6. Inflammation on imaging may be more predictive of a therapeutic response than clinical features | 7.8 | III–IV |
7. US and MRI may be useful in monitoring disease activity, as they allow improved detection of inflammation | 8.3 | III |
8. CR should be considered periodically to evaluate joint damage. MRI (and possibly US) is more responsive to change in joint damage and can monitor disease progression | 7.8 | III |
9. CR (in flexion and neutral) should be used to monitor instability of the C–spine. MRI should be performed if CR positive or if specific neurological findings | 9.4 | III |
10. In clinical remission, MRI and US can detect persistent inflammation | 8.8 | III |
In the detection of subclinical inflammation
As a more accurate assessment of inflamed joints than clinical examination alone
In monitoring disease activity
In determination of remission
In prognosis
RA is a systemic disease with several possible extra-articular features including pulmonary nodules and interstitial lung disease, systemic vasculitis, renal failure, pyoderma gangrenosum, scleritis, arrhythmias and coronary artery disease. Several imaging modalities could be employed to assess these features. The MSK features, rather than the extra-articular features, of RA will be the focus of this text.
Imaging Features
Radiographs
Radiographs are an essential component of any imaging algorithm in the assessment of structural damage in RA. They have several advantages over other imaging modalities: multiple joints can be assessed at the same time (most frequently hands, wrists and feet are requested); radiographs are accessible to most practitioners; well validated methods of interpreting radiographs are established and several pathological features can be identified such as:
Soft tissue swelling
Effusions
Erosions
Osteopenia
Cartilage loss
Furthermore, radiographs are affordable and can detect early osteopenia which neither MRI nor US can visualise. However, plain radiographs are a two-dimensional representation of a three-dimensional structure. This is resolved in part by the addition of tomosynthesis that may represent a more sensitive tool for detecting structural changes (see Chap. 1). In addition, radiographs have low sensitivity particularly early in the course of the disease prior to the development of erosions. This is particularly relevant currently, as there is a clinical drive to detect and treat the disease early in its course to prevent irreversible structural damage and to maintain function, hence the increasing use of ultrasound and MRI in early disease (Table 5.3). Initial radiographic assessment should include posterior-anterior, oblique and lateral projections of the hands and feet. Radiographs are advised even if asymptomatic due to high yield of erosions.
Table 5.3
Imaging and clinical features of the different stages of rheumatoid arthritis with radiographs, ultrasound and MRI
Different stages of RA in hands | |||
|---|---|---|---|
Early | Intermediate | Late | |
Imaging modality | Ultrasound or MRI best for imaging synovitis, effusions and tenosynovitis. MRI can also identify pre-erosive disease. Plain radiographs for periarticular osteopenia | Plain radiographs visualise destructive changes. MRI and US can additionally visualise active inflammatory changes | |
Imaging features | Soft tissue swelling | Soft tissue swelling including tenosynovitis | Soft tissue damage resulting in ulnar deviation and finger drop |
Periarticular osteopenia | Osteopenia | Osteopenia | |
Possible marginal erosions | Marginal erosions progressing to larger erosions | Progression of destructive erosive disease, subluxations and deformities | |
Joint space widening secondary to effusion and synovitis | Joint space narrowing | Joint space narrowing, ankylosis | |
Characteristic clinical features | Soft tissue swelling – particularly MCPJs, PIPJs and wrists | Possible finger drop due to tendon rupture ulnar deviation | MCP subluxation, swan neck and boutonniere’s deformities. Ulnar deviation |
Soft tissue swelling is often the first sign of synovitis and may be secondary to synovial proliferation, effusion or tenosynovitis. This can be visualised as loss of the fat planes and as fusiform swelling around the joints (Fig. 5.3). Soft tissue swelling can be subtle and careful review of the periarticular soft tissues of the same joints is required to identify early changes, i.e. assess and compare the periarticular soft tissues at the MCPJs separately from the PIPJs.
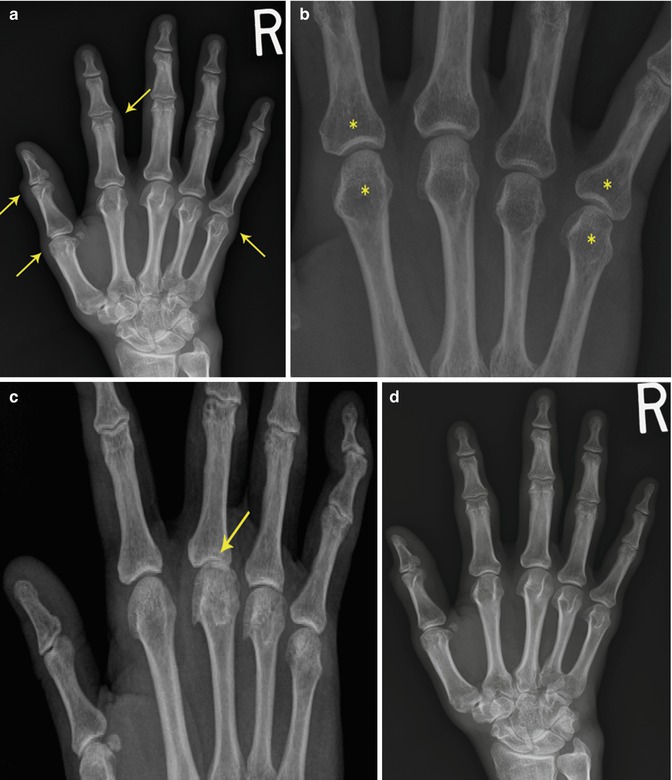
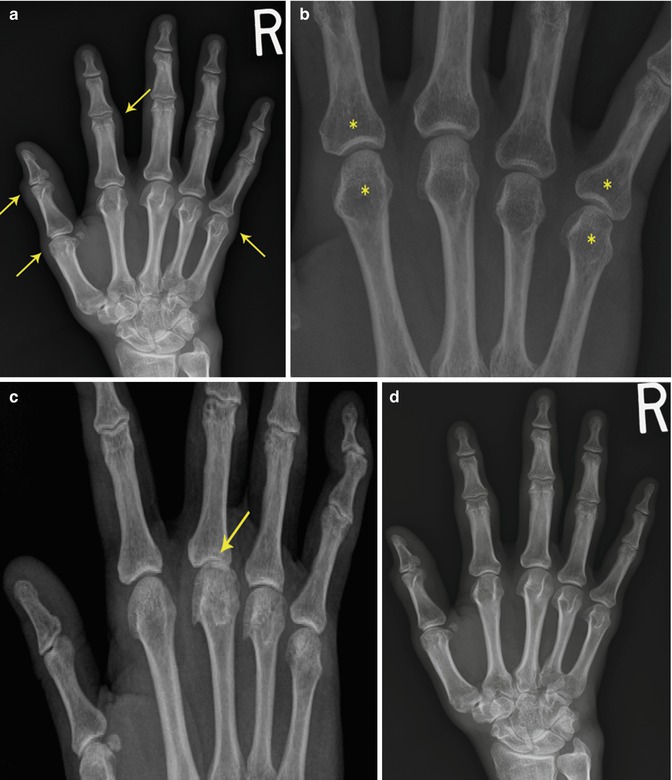
Fig 5.3
(a) Soft tissue swelling of the MCPJs and PIPJs (arrows). (b) Periarticular osteopenia (asterisks). (c) Joint space narrowing at 3rd MCP joint (arrow). (d) Normal R hand radiograph for comparison
Osteopenia is an early radiographic change of active disease (Fig. 5.3b). Osteopenia is thought to be related to high levels of inflammatory cytokines, particularly tumour necrosis factor (TNF)-alpha and interleukin (IL)-6 and IL-17. It is one of the first features of RA and usually predates erosions.
Joint space narrowing (JSN) occurs due to cartilage thinning resulting from the presence of inflammatory cytokines and invasion of synovitis. On plain radiographs, joint space loss is assessed by measuring the distance between the joints, comparing with the other joints in that limb, e.g. MCPJs, and comparing with the other side (Fig. 5.3c). In RA, cartilage loss is usually uniform across the whole joint compared to OA where the cartilage loss is often focal and with subsequent asymmetrical joint space loss.
Erosions and ankylosis are hallmark features of RA. As the disease progresses, erosions develop at the intracapsular articular margins (known as “marginal erosions”) (Fig. 5.4). This region is an area of exposed bone without articular cartilage where the joint capsule inserts, referred to as the “bare area”. A combination of synovial proliferation and invasion (“pannus”) along with high levels of inflammatory cytokines is thought to contribute to the development of marginal erosions. Other pathological changes include tenosynovitis with underlying erosions, for example, at the ulnar styloid (see Fig. 5.9), and cartilage destruction and osteopenia inducing compression erosions. Marginal erosions begin as small cortical breaks. These progress to larger defects in the bony cortex, associated with osteopenia. There is a lack of periosteal sclerosis or new bone formation, which would be typical in psoriatic arthritis or gout (see Fig. 5.32). Progression of erosions occurs without adequate treatment (Fig. 5.5a–d). With progression, there can be bony collapse followed by destruction and ankylosis most commonly seen in the carpal bones (Fig. 5.6).
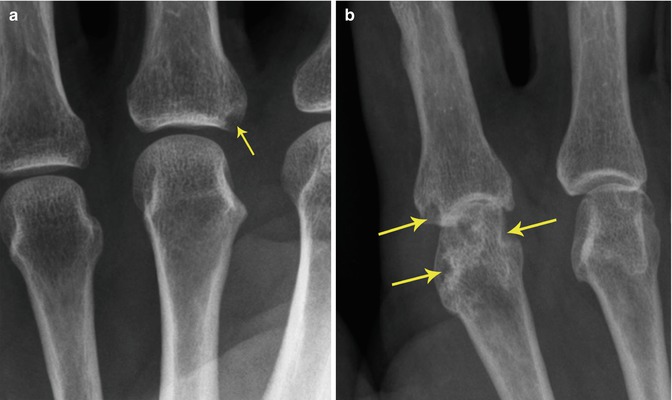
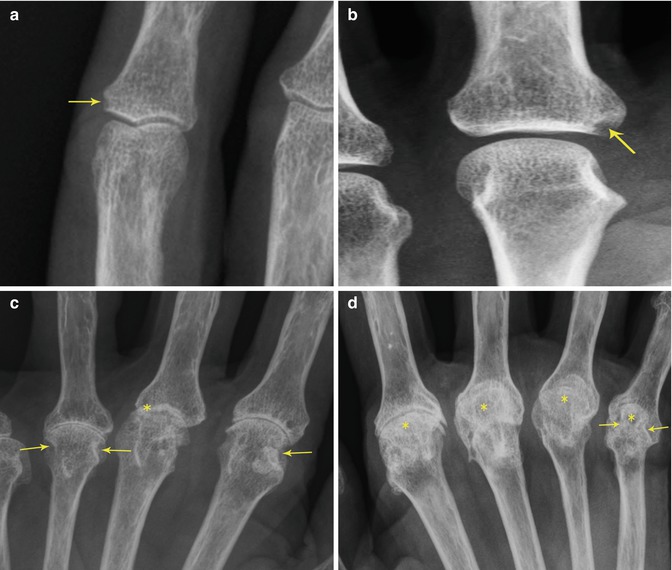
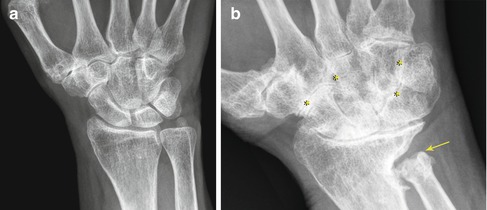
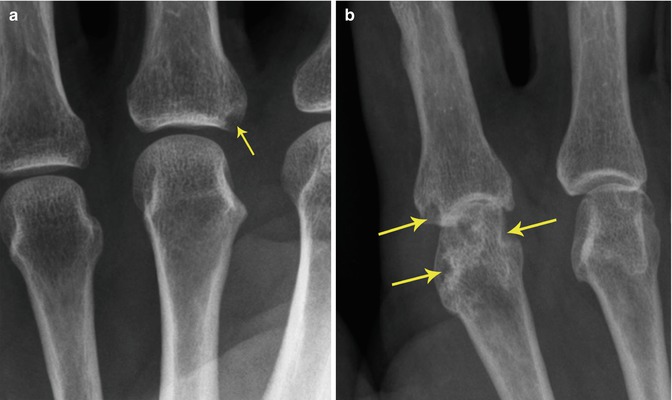
Fig. 5.4
Marginal erosions in (a) a 43-year-old woman with a 2-year history of arthralgia and arthritis symptoms. Small MCP marginal erosion (arrow); (b) 58-year-old man with 10-year history of moderately active RA despite DMARD treatment. Multiple larger erosions affecting metacarpal and proximal phalanx bones (arrows)
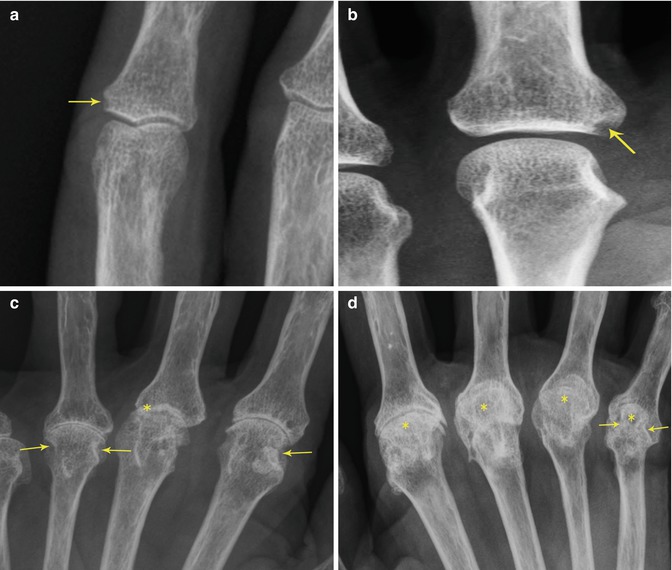
Fig. 5.5
Progression of erosions in four different patients. (a) Marginal erosion at PIP (arrow); (b) larger marginal erosion (arrow); (c) large erosions (arrows) with marked joint space narrowing at MCP (asterisk); (d) erosions (arrow) with joint space narrowing and subluxation at MCP (asterisk)
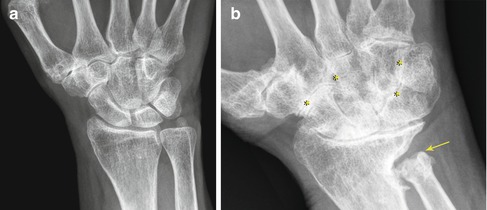
Fig. 5.6
Carpal ankylosis in two different patients: (a) early carpal ankylosis at capitate and hamate and capitate and trapezoid and crowding of the carpal bones in a 58-year-old woman with RA for 15 years and (b) severe carpal ankylosis (asterisk) in a 74-year-old woman with long-standing disease. Note ulnar translocation of the proximal row of carpal bones. Note also large ulnar erosion (arrow)
Joint Involvement
Characteristic Hand Deformities
The characteristic joint involvement in RA is depicted in Fig. 5.2 using the homunculus. The hand and wrist are most commonly involved in RA.
The second and third MCPJs are the most common and earliest joints involved, with frequent involvement of the second and third PIPJs.
Synovitis with joint destruction, tenosynovitis, ligamentous instability and tendon rupture lead to the characteristic deformities of RA – swan neck (Fig. 5.7a) and boutonnière deformities, ulnar deviation (Fig. 5.7c), subluxation at the MCPJs (Fig. 5.7c) and finger drop. In anatomical terms, swan neck deformities relate to hyperextension at the PIP and flexion at the DIP, while boutonniere’s is caused by flexion at the PIP and hyperextension at the DIP (Fig. 5.8).
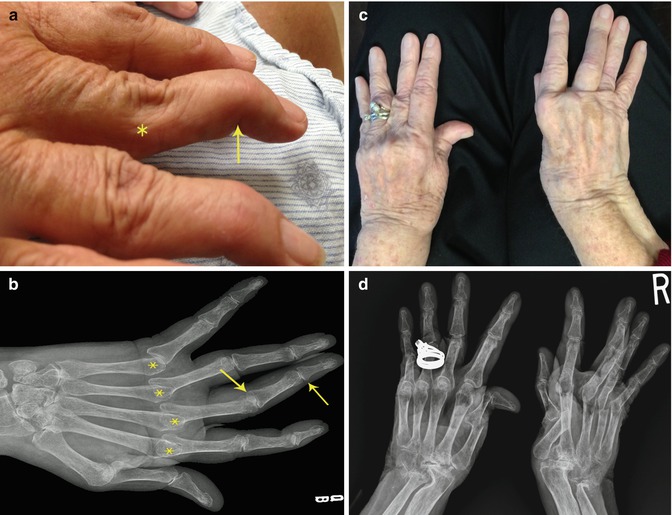
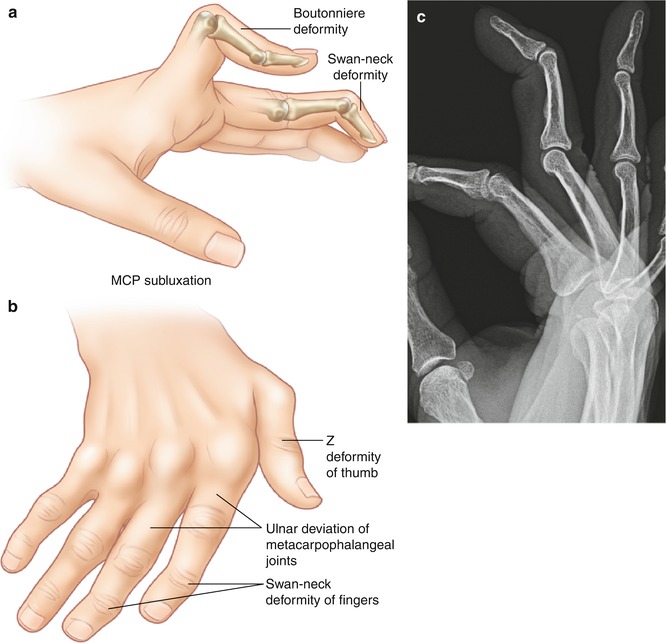
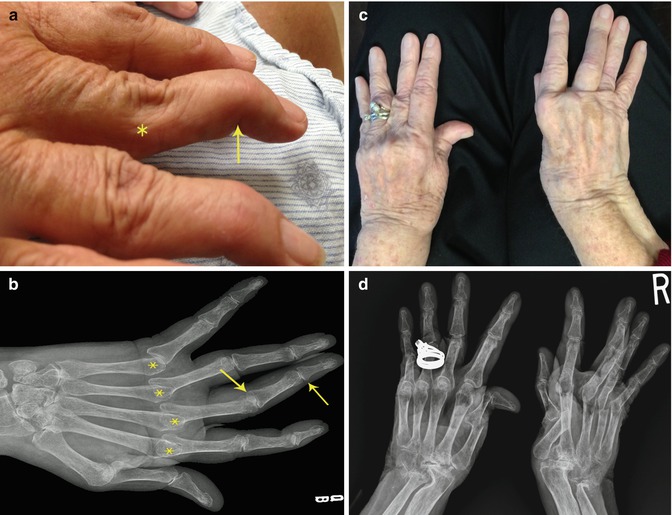
Fig. 5.7
(a) Swan neck deformity with flexion of the DIP (arrow) and hyperextension at PIP with (b) corresponding radiographic features in a 64-year-old woman with long-standing RA; (c) 77-year-old woman with a 50-year history of RA and multiple deformities including subluxation, ulnar deviation, boutonniere’s deformity of right third finger and Z thumb; (d) corresponding radiograph
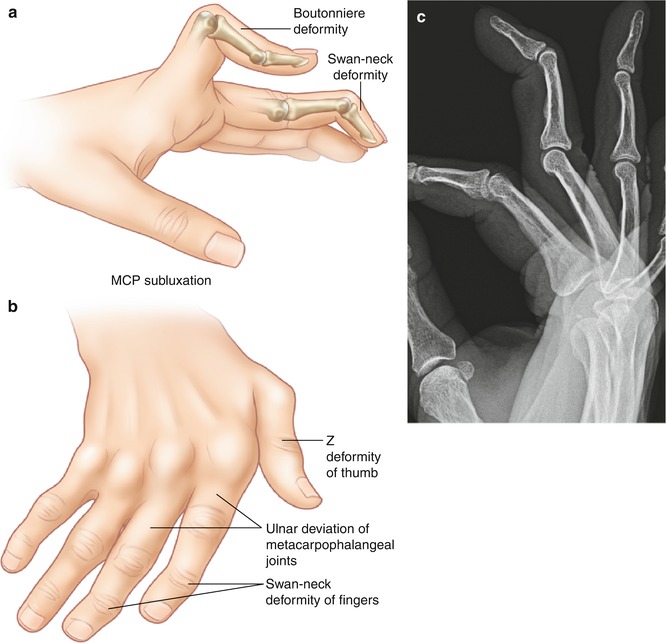
Fig. 5.8
(a) Swan neck and boutonniere’s deformities, (b) chronic deformities in rheumatoid arthritis, (c) magnified lateral hand radiograph demonstrating swan neck deformity
Wrists
In the wrist, there are multiple sites of involvement, including the radiocarpal, intercarpal and distal radioulnar joint, with their own specific radiographic findings. Malalignment generally occurs because of the complex biomechanical forces from tendons and ligaments resulting in subluxations of the carpal bones on the radius or ulna.
Deformities at the wrist include the following:
Erosions at the ulnar styloid (Fig. 5.9)
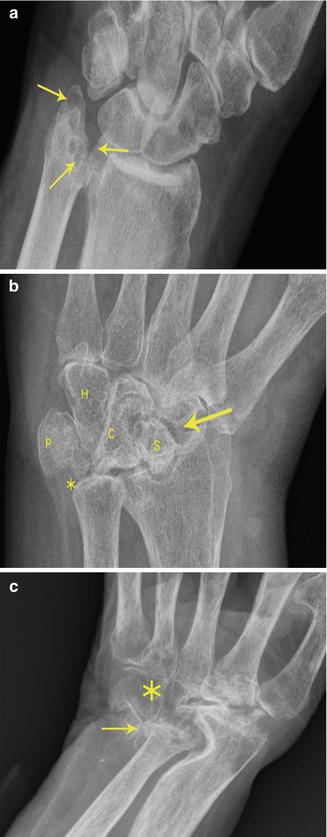
Fig. 5.9
(a) Erosions at ulnar styloid (arrows) in a 53-year-old man with newly diagnosed RA but symptoms for around 5 years; (b) osteolysis of the ulnar styloid (asterisk) with ulnar migration (arrow) of many of the carpal bones (S scaphoid, C capitate, P pisiform, H hamate); (c) complete destruction of the carpus (asterisk) and the ulnar styloid (arrow)
Radial deviation of wrist which may accompany ulnar deviation of fingers
Ulnar translocation of the proximal row of carpals (See Fig. 5.6b)
Dorsal or volar slip of the scaphoid in relation to the lunate
Distal ulnar subluxation with interruption of the distal radioulnar ligaments which may result in the “piano key sign” where pressure on the distal ulna results in impingement on the carpals
Feet and Ankles
In up to 20 % of patients with newly diagnosed RA, the MTP joints are the presenting joints. Deformities and erosions in the MTPJs mimic those in the MCPJs with marginal erosions, soft tissue swelling, joint space narrowing, misalignment and eventual ankylosis. Erosions are particularly commonly seen on the lateral aspect of the fifth MTPJ (Fig. 5.10).


Fig. 5.10
(a) Erosions at MTPJ (arrows) in a 74-year-old woman with 20-year history of RA. (b) Erosions (arrows) and subluxation and lateral deviation (asterisks) of phalanges in a 58-year-old man with inadequately treated RA. (c) Severe destructive arthropathy of the feet
The tibiotalar joint demonstrates cartilage loss with bony erosions around the distal tibiofibular articulation. The intertarsal joints are affected in a similar manner to the intercarpal joints in the hands.
Large Joints
In the knee, hip, elbow and shoulder joints, articular cartilage loss is the predominant finding on plain radiography. Soft tissue swelling (either synovitis or effusion) is also a common feature, particularly in the knee with an increased soft tissue density in the suprapatellar pouch or anterior displacement of the patella visible on lateral knee x-ray. Erosions are the hallmark radiological feature of RA and can be found in any large joints including the knee and elbow (Fig. 5.11a, b). Hip joint effusions can be determined on AP radiographs as a widened distance between the lateral aspect of the acetabulum and the medial femoral head. Often this is asymmetrical, and comparison can be made with the unaffected side. Cartilage loss in the hip in patients with RA is usually uniform throughout the joint and results in migration of the femoral head superiorly and medially in the direction of the femoral neck angulation. This can result in the femoral head protruding in to the pelvis: a condition known as acetabular protrusion.
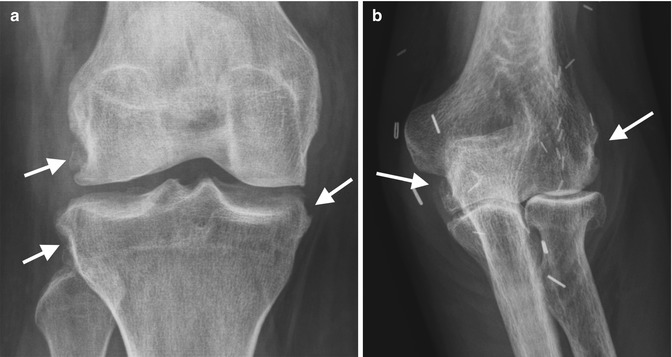
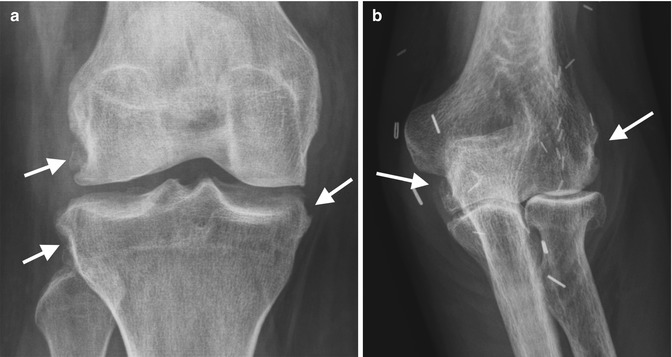
Fig. 5.11
(a) AP radiograph of the knee in a 24-year-old female patient with long-standing RA with multifocal erosions (arrows) with sclerotic margins suggesting erosions are inactive. (b) Marginal erosions elbow different patient with RA. Incidental note of the multiple surgical clips (arrows)
In the elbow, effusions and synovitis can be recognised on plain radiography as first disappearance of the anterior fat pad followed by distension of the posterior fat pad (Fig. 5.12). Cartilage loss and erosion are visible at any of the articulations in the elbow.


Fig. 5.12
Left elbow of a 71-year-old man with long-standing seropositive RA showing large effusion (asterisks) and secondary osteophytosis (arrows). H humerus, R radius, U ulna
Similarly in the shoulder, diffuse uniform cartilage loss and disruption of the rotator cuff tendons result in superior and medial migration of the humerus. Narrowing of the acromiohumeral distance to <6 mm suggests a chronic complete rotator cuff tear involving at least the supraspinatus and often the infraspinatus tendons (this would be best imaged by US or MRI). There can be progression with involvement of the subscapularis and long head biceps and development of a rotator cuff arthropathy.
Spine
The cervical spine is the most commonly affected part of the spine in RA, with up to 70 % of patients demonstrating involvement. Patients may have asymptomatic disease. The atlantoaxial joint is most commonly involved. This is the articulation between the C1 vertebral body, known as the atlas, and the C2, the axis. The axis has a large superior process, the odontoid peg, which articulates with the anterior arch of the atlas. Synovium can be found between the odontoid process (also referred to as the dens) and the atlas and between the odontoid process and the transverse ligament (Fig. 5.13a–c, X-rays, and Fig. 5.14a, b illustration of bones in C spine c CT scan of C-spine involvement). The transverse ligament runs posterior to the odontoid process and maintains stability of the atlantoaxial joint. In rheumatoid synovitis, the integrity of the transverse ligament is compromised, allowing for anterior subluxation of C1 on C2. Furthermore, the odontoid process can be eroded resulting in further instability of the cervical spine and potential spinal cord compression. Flexion views of the cervical spine allow for more accurate assessment of instability with measurement of the posterior atlantodental interval (PADI). This is the distance between the posterior aspect of the odontoid and the anterior surface of the posterior arch of the atlas and should be >14 mm. Axial CT imaging of the neck better delineates erosions of the dens and spinal cord compression. The most extreme neck pathology in RA involves atlantoaxial impaction where the odontoid peg migrates superiorly into the cranium and compromises the spinal cord. With the advent of more intensive therapies for RA, these complications are becoming much less frequent.
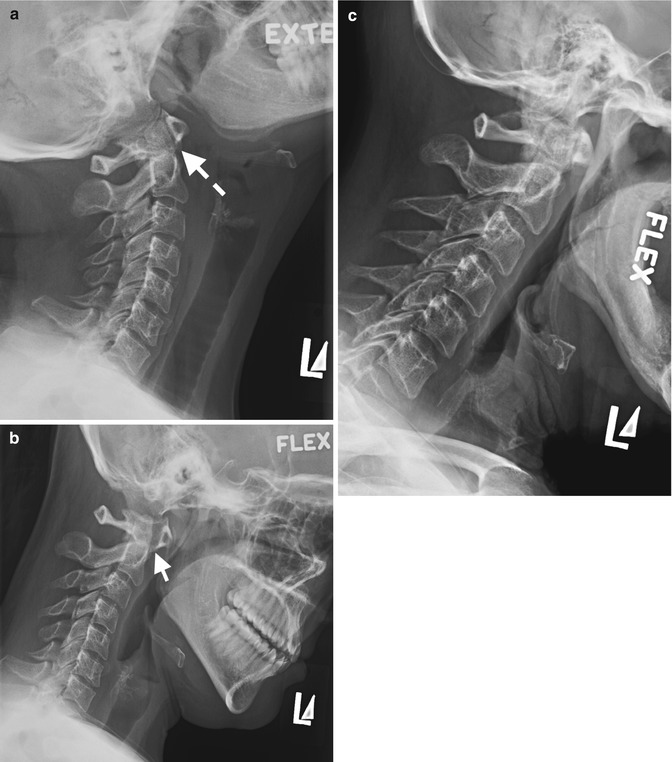
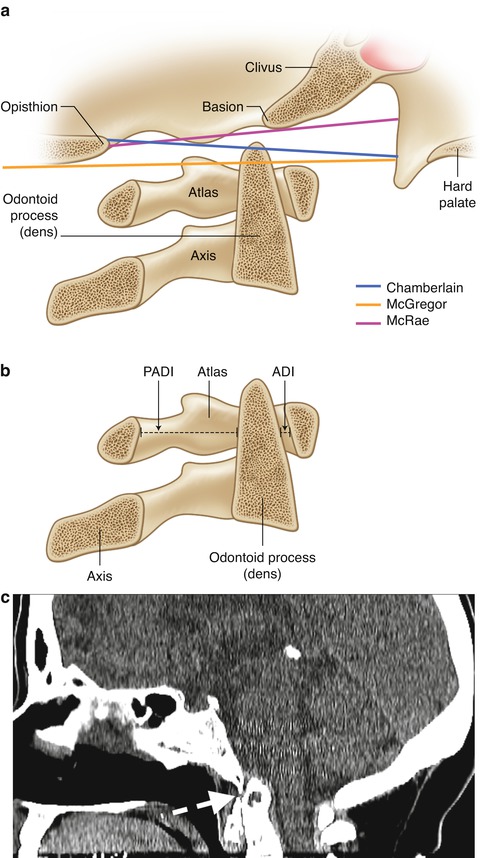
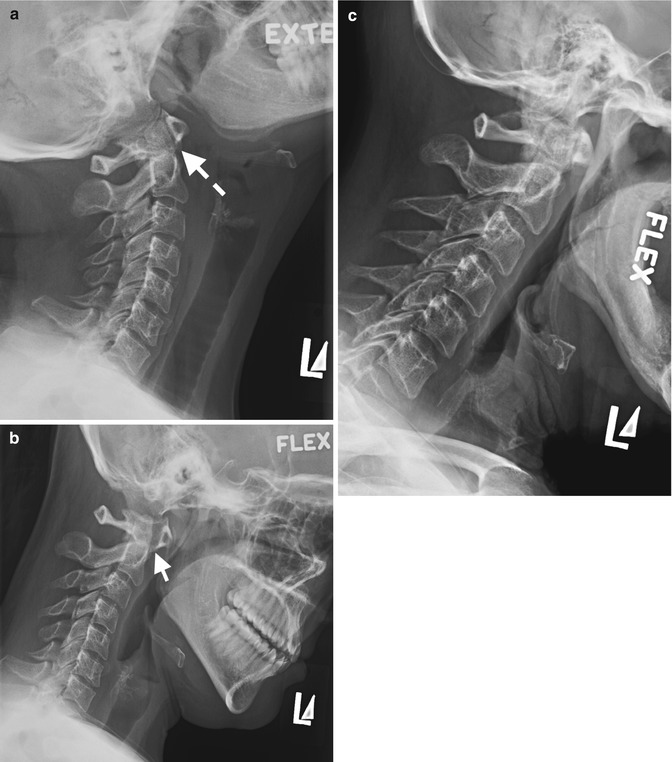
Fig. 5.13
Lateral cervical spine radiographs showing atlantoaxial instability in a 75-year-old woman with long-standing RA in a routine pre-op assessment, (a) in extension with normal atlantoaxial interval (dashed arrow) which increases significantly in flexion, (b) in keeping with instability. Alignment remainder cervical spine is maintained, (c) normal flexed cervical spine for comparison
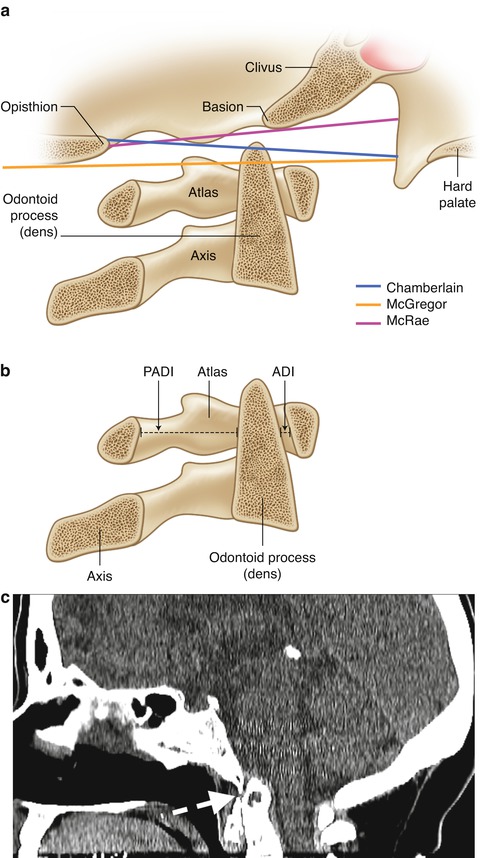
Fig. 5.14
(a, b) Illustration of the bones in the C-spine with measurements of anterior and posterior atlantodental interval (AADI, PADI). (c) A 63-year-old female RA: basilar invagination (dashed arrow) noted as an incidental finding for CT of the paranasal sinuses
Extra-articular Manifestations
The extra-articular manifestations of RA can be imaged by plain radiographs, CT, MRI, US, radioisotope bone scanning, angiography or bone densitometry where appropriate. Other radiographic features include rheumatoid pulmonary nodules or pulmonary fibrosis (either idiopathic or secondary to methotrexate) on plain chest radiograph (Figs. 5.15 and 5.16), avascular necrosis (Fig. 5.17) or osteopenia/osteoporosis secondary to long-term corticosteroid use. Other imaging modalities are better suited to outlining the extra-articular manifestations such as:
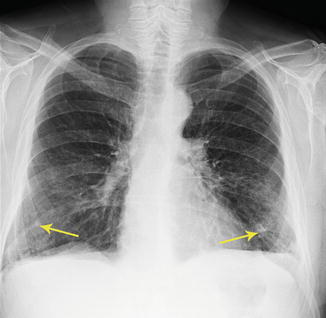
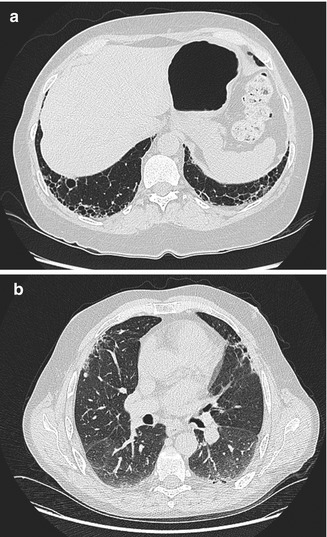
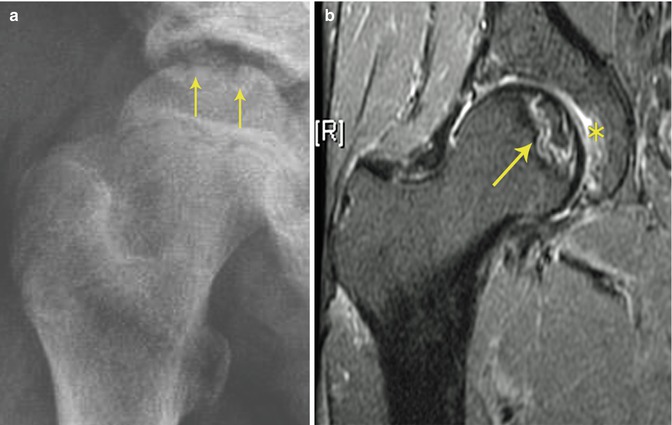
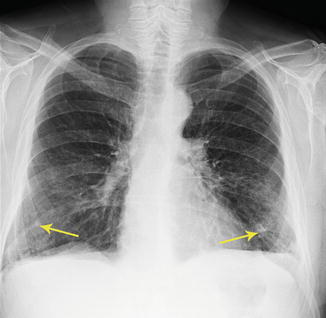
Fig. 5.15
Chest radiographs showing multiple pulmonary nodules (arrows)
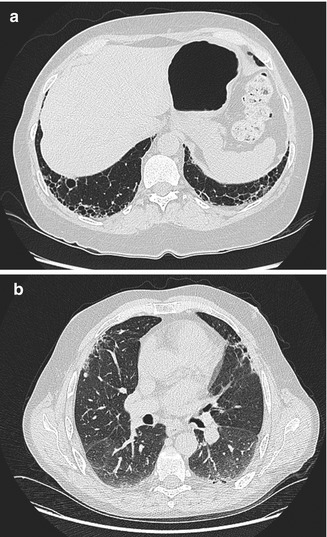
Fig. 5.16
CT chest showing (a) basal pulmonary fibrosis with honeycombing and (b) ground glass opacification on the dorsal side
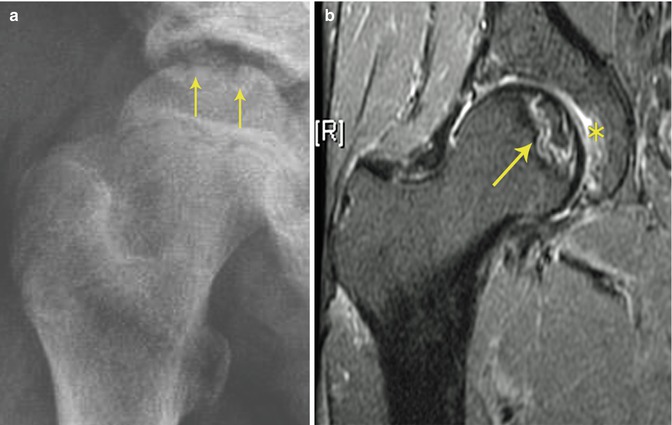
Fig. 5.17
Avascular necrosis (AVN) in a 56-year-old man treated for 30 years with 15 mg prednisone for RA. (a) Plain radiograph with collapsed femoral head (arrows) and (b) corresponding T2-weighted MRI showing BME and collapsed femoral head (arrow), and small effusion (asterisk)
Entrapment neuropathies, popliteal cysts or bursal or tendon involvement best imaged by US or MRI
Vasculitis best imaged by conventional angiography or MRA or CTA
Septic arthritis or osteomyelitis by bone scintigraphy or MRI
Chest pathologies by HRCT
Felty’s syndrome by CT or US
Spinal cord compression by MRI
Osteoporosis by bone densitometry
Secondary osteoarthritic changes and surgical correction are common with long-standing severe RA (Fig. 5.18).


Fig. 5.18
Secondary OA in the C-spine of a woman with long-standing RA with large anterior osteophyte (arrow)
Rheumatoid nodules are typically seen on the extensor surface of MCPJs and PIPJs. Figures 5.15 and 5.19 depict some of the extra-articular features of RA.
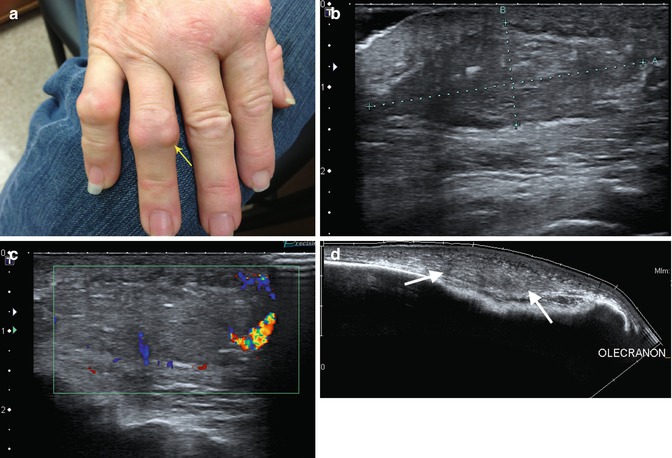
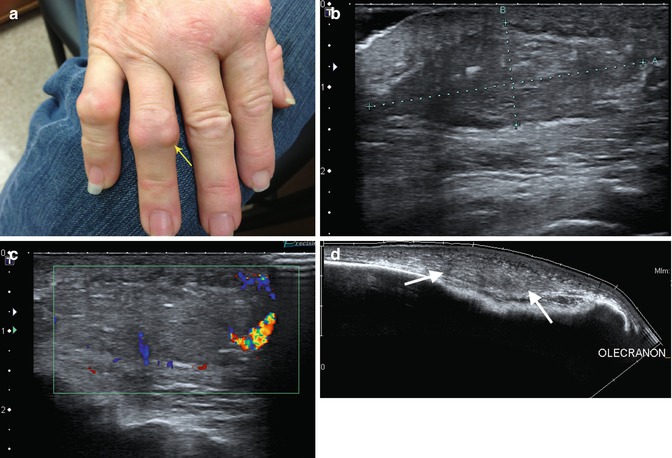
Fig. 5.19
Nodules around PIPJs in 68-year old woman with longstanding seropositive RA. (a) Picture right hand of 68-year old woman with longstanding rheumatoid arthritis with soft tissue nodule (Rheumatoid nodule) over the 4th PIP extensor surface (arrow) (b) same patient with larger rheumatoid nodule on the extensor surface right elbow on ultrasound with (c) peripheral flow on colour Doppler. (d) Extended field of view noting the olecranon as a bony landmark (rheumatoid nodule demarcated with arrows)
Several radiographic scoring methods have been developed for use in clinical studies. These are reviewed in Appendix. The most commonly used scoring system in rheumatoid arthritis is the modified Sharp score that has been adopted by the Outcome Measures in Rheumatology formally called Outcome Measures in Rheumatoid Arthritis Clinical Trials (OMERACT) group.
Tomosynthesis
Tomosynthesis is a relatively new technique which has shown early promise in the assessment of erosions in RA. The technique is described in detail in Chap. 1. It is a more sensitive tool for detecting erosions. An example of a clearly defined erosion visualised by tomosynthesis is shown in Fig. 5.20. This technique requires further research but is likely to be a useful tool for assessing erosions in the future.
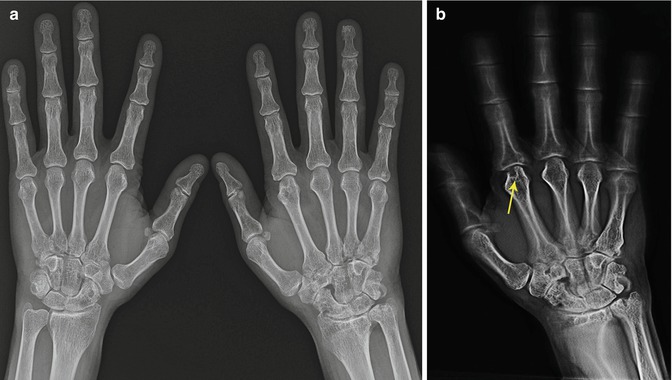
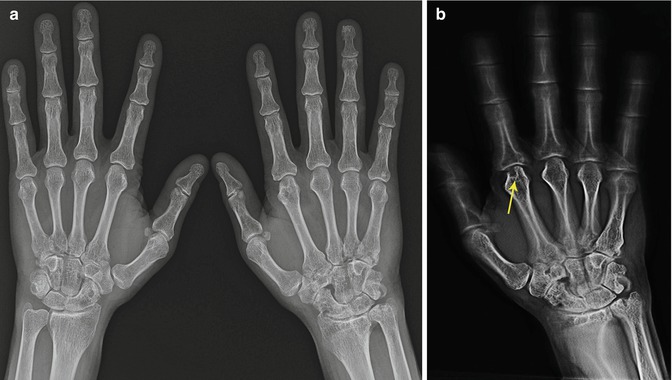
Fig. 5.20
(a) Plain radiograph which looks essentially normal in a 38-year-old man with a 1-year history of arthritis symptoms; (b) corresponding tomosynthesis image of the same patient taken on the same day showing erosion at second MCP (arrow)
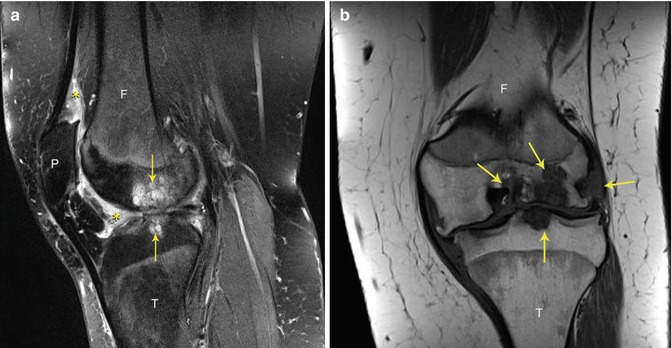
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) (Chaps. 1 and 2) has the advantage of being able to determine synovitis, synovial fluid and bone marrow oedema (which may be an indicator of inflammation), all of which can be seen in early disease in addition to erosions which often occur as the disease progresses. Other imaging modalities cannot determine inflammatory changes within the bone marrow. Bone marrow oedema on MRI is defined as a high signal with irregular borders on T2 fat-suppressed or short tau (STIR) images. BME may predict future erosions. Synovitis has been defined by the OMERACT group as post-gadolinium enhancement of the thickened synovial membrane. On T1-weighted images, erosions appear as focal cortical defects of low signal intensity (SI). Synovitis enhances post-gadolinium. On T2 images, synovitis, bone marrow oedema and synovial fluid have high SI (Figs. 5.21a and 5.22). Active tendon involvement with tenosynovitis also appears high SI.