4 Inflammatory Conditions
Infectious Arthritis
Definition and General Pathology
 Bacteria-induced articular damage
Bacteria-induced articular damage
 Hyperemia and proliferation of the synovial membrane with capsular thickening
Hyperemia and proliferation of the synovial membrane with capsular thickening
 Exudation with joint effusion and capsular and periarticular edema
Exudation with joint effusion and capsular and periarticular edema
 Destruction of the synovial membrane, capsule, cartilage, and subchondral bone
Destruction of the synovial membrane, capsule, cartilage, and subchondral bone
Acute Infectious Arthritis
Pathology
 Most frequent cause: Local corticosteroid injection with incidental contamination
Most frequent cause: Local corticosteroid injection with incidental contamination
 Rare: Hematogenous spread of an infection (e.g., head-neck infection, dental abscesses)
Rare: Hematogenous spread of an infection (e.g., head-neck infection, dental abscesses)
 Very rare: Local spread of an infection following external injuries
Very rare: Local spread of an infection following external injuries
 Also rare: Hematogenous spread of a prosthetic infection
Also rare: Hematogenous spread of a prosthetic infection
Clinical Findings
 Considerable painful soft-tissue swelling
Considerable painful soft-tissue swelling
 Erythema and hyperthermia around the joint
Erythema and hyperthermia around the joint
 Restricted motion
Restricted motion
 Elevated C-reactive protein and sedimentation rate, leukocytosis
Elevated C-reactive protein and sedimentation rate, leukocytosis
Diagnostic Evaluation

Indications
 Diagnosis and follow-up
Diagnosis and follow-up
Findings
 Arthritic soft-tissue signs (often subtle):
Arthritic soft-tissue signs (often subtle):
– Depends on patient’s age, arthritis stage, and causes
– Added soft-tissue density of the joint cavity (effusion and synovial swelling)
– Periarticular edema
– Swelling with homogenization of the juxta-articular soft tissues
– Obliterated fat stripes
 Collateral phenomenon:
Collateral phenomenon:
– Patchy or band-like demineralization of the articulating subchondral bone at about two weeks after, for instance, local corticosteroid injection
 Direct arthritic signs:
Direct arthritic signs:
– Joint-space narrowing caused by infectious pannus with destruction of the cartilage
– Joint-space widening caused by effusion or empyema with capsular distension, especially in the growth period (rare in adults)
– After three to four weeks (without therapy), marginal bone destruction (bare areas) (Fig. 4.2)
– Later also central cystoid bone destruction
– Metaphyseal periosteal reaction
– After commencement of the antibiotic therapy, initially progression of the destruction, first marginally, then centrally
– Removal of debris over months, even if the process has subsided clinically and serologically
Assessment
 Initial diagnosis and baseline for follow-up
Initial diagnosis and baseline for follow-up
 Normal findings do not exclude the diagnosis of infectious arthritis
Normal findings do not exclude the diagnosis of infectious arthritis
 An abnormal finding is reasonably specific
An abnormal finding is reasonably specific

Indications
 Specific clinical questions
Specific clinical questions
 Procuring joint fluid and detection of organism
Procuring joint fluid and detection of organism
 Diagnosis of rotator-cuff tear
Diagnosis of rotator-cuff tear
Findings
 Inflammatory synovial changes
Inflammatory synovial changes
Assessment
 Largely replaced by sonography
Largely replaced by sonography
 (Caution: very operator dependent)
(Caution: very operator dependent)
Indications
 Suitable for follow-up, especially in children
Suitable for follow-up, especially in children
 Aspiration of joint fluid, synovial biopsy, for detection of organism
Aspiration of joint fluid, synovial biopsy, for detection of organism
 Diagnosis of rotator-cuff tear
Diagnosis of rotator-cuff tear
Findings
 Detection of effusion/empyema
Detection of effusion/empyema
 Absent effusion virtually excludes bacterial infection
Absent effusion virtually excludes bacterial infection
 Detection of large osseous defects
Detection of large osseous defects
 Rotator-cuff tears and defects (inflammation-induced)
Rotator-cuff tears and defects (inflammation-induced)
Assessment
 More complementary than diagnostic
More complementary than diagnostic
 Suitable to guide the joint aspiration
Suitable to guide the joint aspiration

Indications
 Suspected multiple infectious foci
Suspected multiple infectious foci
 Undetermined location of an infection
Undetermined location of an infection
Method
 Three-phase bone scan
Three-phase bone scan
 White blood cell (WBC) scan
White blood cell (WBC) scan
Findings
 Increased juxta-articular uptake in all three phases
Increased juxta-articular uptake in all three phases
 In the late phase also increased uptake in the joint fluid
In the late phase also increased uptake in the joint fluid
 WBC scan superior for soft-tissue foci than for osseous foci
WBC scan superior for soft-tissue foci than for osseous foci
Assessment
 Positive for days to weeks before the radiograph becomes positive
Positive for days to weeks before the radiograph becomes positive
 Bone scan sensitive but not specific
Bone scan sensitive but not specific
Goals of Imaging
 Differential diagnosis between arthritis, tumor, and trauma
Differential diagnosis between arthritis, tumor, and trauma
 Diagnosis of the type of arthritis
Diagnosis of the type of arthritis
 Extent of the arthritis
Extent of the arthritis
 Localization of the inflammatory process (intra-articularor periarticular, meta-physeal)
Localization of the inflammatory process (intra-articularor periarticular, meta-physeal)
 Extent of the soft-tissue involvement (subdeltoid, subpectoral, subtrapezoid soft-tissue abscesses along the biceps tendon)
Extent of the soft-tissue involvement (subdeltoid, subpectoral, subtrapezoid soft-tissue abscesses along the biceps tendon)
 Determination of any osseous involvement and its extent
Determination of any osseous involvement and its extent
 Determination of the continuity or discontinuity of the rotator cuff
Determination of the continuity or discontinuity of the rotator cuff
 Possibly sonography-guided aspiration to confirm the diagnosis and to identify the causative organisms
Possibly sonography-guided aspiration to confirm the diagnosis and to identify the causative organisms
Therapeutic Principles
Conservative
Emergency requiring early and aggressive therapy. Inpatient and interdisciplinary therapy! Conservative therapy alone is not sufficient.
 Prevention of joint destruction and septic complications
Prevention of joint destruction and septic complications
 Local cryotherapy, only short period of immobilization, early mobilization therapy
Local cryotherapy, only short period of immobilization, early mobilization therapy
 Intravenous antibiotic therapy after culture of the synovial fluid and antibiogram
Intravenous antibiotic therapy after culture of the synovial fluid and antibiogram
 Empirically until the result of the antibiogram is available, for example, Cefuroxime/Cefotaxime and Flucloxa cillin
Empirically until the result of the antibiogram is available, for example, Cefuroxime/Cefotaxime and Flucloxa cillin
Surgical
In the early stage with the rotator cuff still intact and osteomyelitis excluded:
 Arthroscopy
Arthroscopy
 Synovectomy
Synovectomy
 Irrigation and suction drain
Irrigation and suction drain
 Targeted antibiotics
Targeted antibiotics
In the late stage with abscess formation, associated osteomyelitis or torn rotator cuff:
 Open revision, debridement
Open revision, debridement
 Possibly synovectomy
Possibly synovectomy
 Insertion of PMMA (poly methylmethacrylate) beads
Insertion of PMMA (poly methylmethacrylate) beads
 Systemic therapy with targeted antibiotics
Systemic therapy with targeted antibiotics
Prosthetic infection:
 Early stage: Local debridement, synovectomy, PMMA beads, systemic therapy with targeted antibiotics, prosthesis remains in place
Early stage: Local debridement, synovectomy, PMMA beads, systemic therapy with targeted antibiotics, prosthesis remains in place
 Late stage: Revision with exchange of the prosthesis, possibly in two sessions with temporary interim prothesis (increased complication rate, salvage arthrodesis risk-prone)
Late stage: Revision with exchange of the prosthesis, possibly in two sessions with temporary interim prothesis (increased complication rate, salvage arthrodesis risk-prone)

Indications
 Possibly used together with aspiration of effusion/empyema and synovial biopsy for determination of the organism
Possibly used together with aspiration of effusion/empyema and synovial biopsy for determination of the organism
 Delineation of the osseous structures, especially of any glenoid destruction
Delineation of the osseous structures, especially of any glenoid destruction
 Suspicion for associated osteomyelitis to exclude any sequesters
Suspicion for associated osteomyelitis to exclude any sequesters
Findings
 Osseous destruction
Osseous destruction
 Medullary extension (soft-tissue density occupying the marrow space)
Medullary extension (soft-tissue density occupying the marrow space)
 Delineation of sequesters
Delineation of sequesters
 Extension into surrounding soft tissues (intravenous contrast medium)
Extension into surrounding soft tissues (intravenous contrast medium)
Assessment
 Advisable for cases benefitting from a clear delineation of the extent of osseous destruction
Advisable for cases benefitting from a clear delineation of the extent of osseous destruction
 To determine the extent of an advanced process if magnetic resonance imaging (MRI) is contraindicated
To determine the extent of an advanced process if magnetic resonance imaging (MRI) is contraindicated

Indications
 To determine the extent into the surrounding soft tissues and to delineate the articular findings (abscess cavities, fistulous tracts, etc.)
To determine the extent into the surrounding soft tissues and to delineate the articular findings (abscess cavities, fistulous tracts, etc.)
Method
 Superficial or shoulder coil
Superficial or shoulder coil
 Supine, arm parallel to the body and in neutral position
Supine, arm parallel to the body and in neutral position
 Sequences:
Sequences:
– Unenhanced paracoronal or axial T1-weighted spin-echo (SE) or gradient-echo (GE) sequence
– Unenhanced paracoronal T2-weighted short time to inversion recovery (STIR) or axial T2-weighted turbo spin-echo (TSE) fast spin (FS) sequence
– Enhanced paracoronal or axial T1-weighted FS sequences
Findings
 Effusion:
Effusion:
– T2-weighted image: hyperintense; unenhanced T1-weighted image: hypointense; enhanced fat-suppressed T1-weighted image: no enhancement in the early stage, faint enhancement possible in the late stage (diffusion across inflamed synovia)
– With high proportion of leukocytes/protein: unenhanced T1-weighted image: isointense to hyperintense
 Synovitis (Fig. 4.1 a–c):
Synovitis (Fig. 4.1 a–c):
– Thickened synovial membrane and capsule
– Unenhanced T1-weighted image: intermediate; T2-weighted image: slightly hyperintense or intermediate; enhanced fat-suppressed T1-weighted image: enhancement (bone-marrow edema) (Fig. 4.1 a–c)
 Bone-marrow edema:
Bone-marrow edema:
– Subchondral bone-marrow edema, initially along articular margin, near the capsular insertion
– Later extensive irregular epiphyseal or epimetaphyseal bone-marrow edema (unenhanced T1-weighted image: loss of fat signal; T2-weighted image with fat suppression or STIR: hyperintense; enhanced T1-weighted image: variable enhancement
 Cartilage and bone erosions, cystoid destruction (T1-weighted image: intermediate; T2-weighted image: hyperintense; enhanced T1-weighted image: enhancement (Fig. 4.2 d)
Cartilage and bone erosions, cystoid destruction (T1-weighted image: intermediate; T2-weighted image: hyperintense; enhanced T1-weighted image: enhancement (Fig. 4.2 d)
 Periarticular extension:
Periarticular extension:
– Abscesses, collection of pus (T1-weighted image: intermediate or slightly hyperintense; T2-weighted image: hyperintense; enhanced T1-weighted image: no early enhancement; enhancement in abscess membrane)
– Bursitis (effusion, synovitis)
– Involvement of muscle compartment
– Rotator-cuff lesion
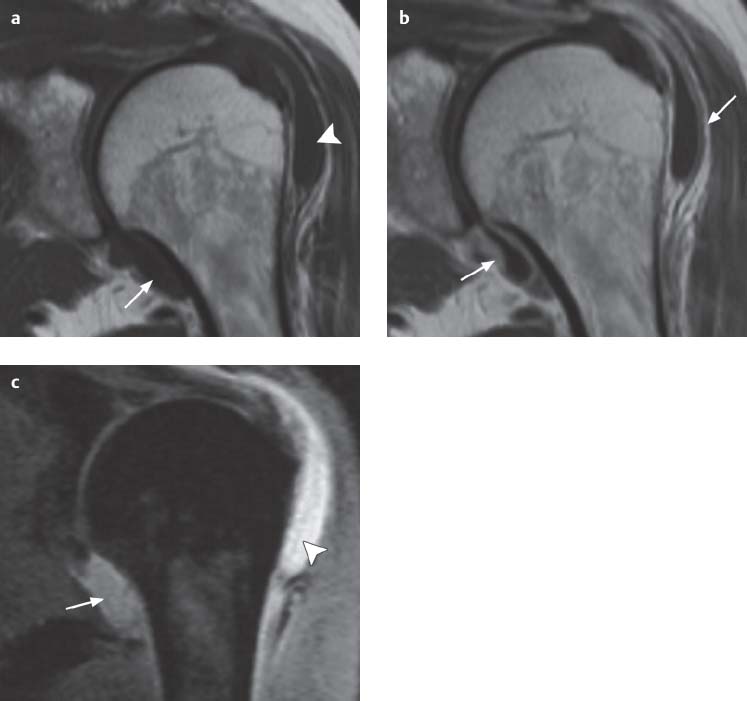
Fig. 4.1 a–c  Infectious arthritis
Infectious arthritis
A 63-year-old female patient following several corticosteroid injections into the left shoulder. Afterwards increasing pain and restricted movement. Staphylococcus aureus was found in the aspirated fluid.
a Paracoronal T1-weighted SE image. Moderate joint effusion (arrow) and extensive effusion in the subacromial/subdeltoid bursa (arrowhead) as manifestation of inflammatory exudation. No detectable osseous erosions.
b Paracoronal T1-weighted SE image after administration of contrast medium, showing enhancement of the synovial membrane as manifestation of synovitis (arrows). No detectable osseous erosions.
c T2-weighted STIR image. Extensive joint effusion (arrow) and effusion in the subacromial/subdeltoid bursa (arrowhead). No noteworthy bone-marrow edema. No detectable osseous erosions. Status post rotator-cuff tear.
(Courtesy of Drs. B. Kormeier and K. Schwieren, Department of Radiology, St. Marien-Hospital Borken GmbH)
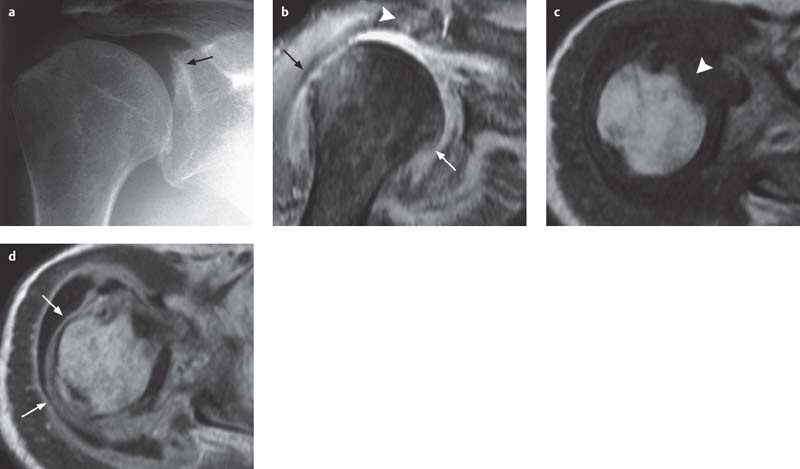
Fig. 4.2 a–d  Infectious arthritis
Infectious arthritis
A 90-year-old male patient with extensive empyema of the shoulder caused by Staphylococcus aureus. Source of infection unknown, most likely hematogenous spread.
a AP radiograph of the right shoulder. Small destructive foci at the upper glenoid margin (arrow).
b Paracoronal fat-saturated proton density-weighted TSE image. Complete destruction of the rotator cuff (arrowhead). Joint effusion. Effusion in the subdeltoid bursa. Bone-marrow edema. Lateral and medial marginal destruction of the humeral head (arrows).
c Axial T1-weighted SE image before administration of contrast medium. Hypointense effusion in the markedly distended subdeltoid bursa. Loss of the bone-marrow signal in the anterior and medial subchondral humeral head with adjacent erosion (arrowhead).
d Axial T1-weighted SE image after administration of contrast medium, same level as in c. Markedly distended subdeltoid bursa with marginal linear enhancement. Furthermore, linear enhancement of the anterior and posterior synovial membrane of the glenohumeral articulation (arrows) and bicipital tendon compartment. Subtle enhancement also adjacent to the humeral erosion.
(Courtesy of Drs. B. Kormeier and K. Schwieren, Department of Radiology, St. Marien-Hospital Borken GmbH)
Assessment
 Superior imaging modality with high sensitivity for soft-tissue and bone infection
Superior imaging modality with high sensitivity for soft-tissue and bone infection
 Not every bone-marrow edema in infectious arthritis corresponds to an accompanying osteomyelitis
Not every bone-marrow edema in infectious arthritis corresponds to an accompanying osteomyelitis
Chronic Infectious Arthritis
Tuberculous Arthritis
Pathology
 Initial focus in either subchondral bone marrow or synovial membrane (synovial type)
Initial focus in either subchondral bone marrow or synovial membrane (synovial type)
 Special case: tuberculous arthritis arising from the subacromial bursa
Special case: tuberculous arthritis arising from the subacromial bursa
Clinical Findings
 More indolent chronic course
More indolent chronic course
 Patients form middle age onward
Patients form middle age onward
 Mostly monoarticular, shoulder infrequently involved
Mostly monoarticular, shoulder infrequently involved
Diagnostic Evaluation

Indications
 Diagnosis and follow-up
Diagnosis and follow-up
Findings
 Typical: minimal or no joint-space narrowing
Typical: minimal or no joint-space narrowing
 Soft-tissue swelling
Soft-tissue swelling
 Severe demineralization of the juxta-articular bone
Severe demineralization of the juxta-articular bone
 Initially marginal, later also large central osseous destruction (developing after several months, often only detectable on cross-sectional image)
Initially marginal, later also large central osseous destruction (developing after several months, often only detectable on cross-sectional image)
Assessment
 Normal radiographic finding does not exclude the diagnosis (delayed imaging manifestation)
Normal radiographic finding does not exclude the diagnosis (delayed imaging manifestation)

 Only in complex cases (Fig. 4.4a–c)
Only in complex cases (Fig. 4.4a–c)
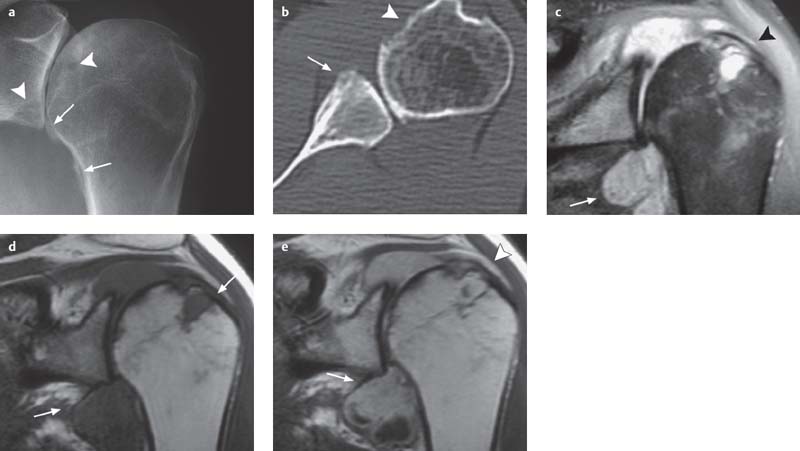
Fig. 4.3 a–e  Rheumatoid arthritis
Rheumatoid arthritis
A 30-year-old female patient with clinical suspicion of rheumatoid arthritis. Differential diagnosis: Septic arthritis of the shoulder.
a AP radiograph of the shoulder. Joint-space narrowing. Subcapital periosteal reaction, extending along the humeral metaphysis (arrow). Destructive changes of the glenoid cavity and humeral head (arrowheads).
b Axial CT. Joint-space narrowing. Flat anteromedial erosion of the humeral head (arrow). Small anteromedial destruction of the glenoid cavity (arrowhead).
c Fat-saturated, proton density-weighted TSE image. Joint effusion in a distended joint cavity with protruding axillary recess and hyperintense intra-articular material (arrow). Patchy humeral and glenoid marrow edema. Major superolateral marginal destruction of the humeral head (arrowhead). Rotator-cuff tear.
d T1-weighted SE image before administration of contrast medium. Cartilage destruction. Loss of the subchondral humeral and glenoid fatty marrow signal, corresponding to areas of bone-marrow edema. Joint cavity and marginal destructive changes are filled with material of medium signal intensity (arrows).
e Axial T1-weighted SE image after administration of contrast medium. Considerable enhancement of the joint cavity and destructive changes, containing in part spherical and in part amorphous tissue structures (arrow). Furthermore, partially linear enhancement of the thickened synovial membrane (arrowhead). Typical manifestation of rheumatoid arthritis. Minimal subchondral enhancement.
(Courtesy of Drs. B. Kormeier and K. Schwieren, Department of Radiology, St. Marien-Hospital Borken GmbH)

Fig. 4.4 a–c  Rheumatoid arthritis and concomitant tuberculous arthritis
Rheumatoid arthritis and concomitant tuberculous arthritis
Male patient with long-standing chronic polyarthritis with involvement of the shoulder, now complaining of increasing pain. Diagnosis confirmed by sonographically guided aspiration of the subdeltoid bursa.
a Sonography. Hypoechoic distension of the subdeltoid bursa containing occasional linear echoes.
b Axial T2-weighted MR image. Visualization of a strongly hyperintense effusion containing less hyperintense areas within the joint capsule and in anteriorly located subchondral bursa.
c Axial fat-suppressed T1-weighted image after administration of Gd-DTPA. The fluid shows low signal intensity and extends anteriorly to the anterior labrum. Large areas within the joint cavity show strong enhancement, corresponding to synovial tissue. It is not possible to differentiate between rheumatoid arthritis and tuberculous arthritis as the underlying cause of the synovitis, but rheumatoid arthritis appears more likely. Moreover, comparison with the T2-weighted image reveals no contrast enhancement anteriorly in the subcoracoid bursa, except for minimal rim enhancement, attributed to caseating granulomas.
(Courtesy of Prof. Dr. K. Bohndorf, Augsburg)
Rheumatoid Arthritis
Pathology
 Proliferation of destructive pannus tissue
Proliferation of destructive pannus tissue
 Frequently early destruction of the ligamentous support with tear of the capsule, rotator cuff, and bicipital tendon
Frequently early destruction of the ligamentous support with tear of the capsule, rotator cuff, and bicipital tendon
 Only later bone destruction: initially small marginal, later mostly deep erosions and cystoid changes in the superolateral aspect of the humeral head next to the major tuberosity
Only later bone destruction: initially small marginal, later mostly deep erosions and cystoid changes in the superolateral aspect of the humeral head next to the major tuberosity
 With progression, involvement of the anatomical neck with substantial destruction of the major tuberosity
With progression, involvement of the anatomical neck with substantial destruction of the major tuberosity
 Loss of joint space due to progressing cartilage destruction
Loss of joint space due to progressing cartilage destruction
 Considerable flattening of the articular surfaces
Considerable flattening of the articular surfaces
 Pressure erosions of the surgical neck medially due to grating of the inferior margin of the glenoid process
Pressure erosions of the surgical neck medially due to grating of the inferior margin of the glenoid process
 Positive rheumatoid factor test
Positive rheumatoid factor test
Clinical Findings
 Painful motion restriction, often noticed late due to the tendency of letting the hands rest
Painful motion restriction, often noticed late due to the tendency of letting the hands rest
 Late involvement of the shoulder in “classical” progression of rheumatoid arthritis
Late involvement of the shoulder in “classical” progression of rheumatoid arthritis
 Primary manifestation of the gleno-humeral joint in “atypical” rheumatoid arthritis (usually older patients)
Primary manifestation of the gleno-humeral joint in “atypical” rheumatoid arthritis (usually older patients)
 Further motion restriction due to rotator-cuff tear, possible subluxation
Further motion restriction due to rotator-cuff tear, possible subluxation
 Accompanying subacromial/subdeltoid bursitis with considerable soft-tissue swelling
Accompanying subacromial/subdeltoid bursitis with considerable soft-tissue swelling
Diagnostic Evaluation

Indications
 Diagnosis of shoulder involvement and follow-up
Diagnosis of shoulder involvement and follow-up
 Close anatomical-pathological correlation corresponding to the described changes
Close anatomical-pathological correlation corresponding to the described changes
 Soft-tissue signs (appearing late in the shoulder):
Soft-tissue signs (appearing late in the shoulder):
– Added soft-tissue density (inflammatory swelling) but also soft-tissue loss (atrophy)
– Uniform appearance of the soft tissues
– Obliteration of the fat stripes, effusion
 Collateral arthritic changes:
Collateral arthritic changes:
– Juxta-articular osteoporosis
 Direct arthritic changes:
Direct arthritic changes:
– Progressive joint-space narrowing
– Bone destruction, especially of the superolateral articular surface of the humeral head (Figs. 4.9 c, 4.10), up to the point of mutilation (Fig. 4.12)
– Increasing deformity and flattening of the head and glenoid process
– Pressure erosions on the surgical neck
– Elevation of the humeral head, possible subluxation due to torn rotator cuff, subacromial neoarticulation (Fig. 4.9)
– Secondary osteoarthritis (Fig. 4.10)
– Complicating osteonecrosis of the humeral head (Fig. 4.11)
Assessment
 Especially in the shoulder joint, the inflammatory changes involve the ligamentous support structures early, often resulting in the radiographic underestimation of the damage
Especially in the shoulder joint, the inflammatory changes involve the ligamentous support structures early, often resulting in the radiographic underestimation of the damage

Indications/Assessment
 No longer indicated, superseded by ultrasound (US) and magnetic resonance imaging (MRI)
No longer indicated, superseded by ultrasound (US) and magnetic resonance imaging (MRI)
Findings
 Diagnosis of rotator cuff (extra-articular extension of contrast medium into the bursa)
Diagnosis of rotator cuff (extra-articular extension of contrast medium into the bursa)
 Intra-articular spherical defects corresponding to pannus (Fig. 4.9)
Intra-articular spherical defects corresponding to pannus (Fig. 4.9)

Indications
 Evaluation of rotator cuff, bicipital tendon, and bursa
Evaluation of rotator cuff, bicipital tendon, and bursa
Findings
 Effusion, pannus, and orientational search for pannus destruction of the humeral head, especially during follow-up
Effusion, pannus, and orientational search for pannus destruction of the humeral head, especially during follow-up
 Tear of the bicipital tendon and rotator cuff, bursitis (Fig. 4.7a, b)
Tear of the bicipital tendon and rotator cuff, bursitis (Fig. 4.7a, b)
 Dynamic assessment of the joint function, possible contralateral comparison
Dynamic assessment of the joint function, possible contralateral comparison
Assessment
 To be obtained before other cross-sectional images
To be obtained before other cross-sectional images
 Most important method for visualizing rotator cuff, bursa, and bicipital tendon
Most important method for visualizing rotator cuff, bursa, and bicipital tendon

Indications
 Rarely indicated, possibly visualizing the extent of osseous destruction
Rarely indicated, possibly visualizing the extent of osseous destruction
Findings
 Joint effusion
Joint effusion
 Erosions, destruction (Fig. 4.11)
Erosions, destruction (Fig. 4.11)
Assessment
 Superior visualization of osseous destruction, especially in 2-D and 3-D reconstruction (Fig. 4.12)
Superior visualization of osseous destruction, especially in 2-D and 3-D reconstruction (Fig. 4.12)

Indications
 Possibly assessment for stability and of the rotator cuff if US is inadequate
Possibly assessment for stability and of the rotator cuff if US is inadequate
 Investigational: Determining prognosis, monitoring therapy (Fig. 4.8) (so far primarily applied to the hand)
Investigational: Determining prognosis, monitoring therapy (Fig. 4.8) (so far primarily applied to the hand)
Method
 As in infectious arthritis, possibly visualizing the cartilage (T1-weighted GE sequence)
As in infectious arthritis, possibly visualizing the cartilage (T1-weighted GE sequence)
 Investigational: Time-activity pattern of enhancement, volumetric assessment of synovitis
Investigational: Time-activity pattern of enhancement, volumetric assessment of synovitis
Findings
 Effusion in joint and bursae (T1 weighting: hypointense; T2 weighting: hyperintense; no early enhancement, possibly faint late enhancement secondary to diffusion across inflamed synovia)
Effusion in joint and bursae (T1 weighting: hypointense; T2 weighting: hyperintense; no early enhancement, possibly faint late enhancement secondary to diffusion across inflamed synovia)
 Synovitis:
Synovitis:
– Irregular thickening of the synovial membrane (T1 weighting: inter- mediate intensity; T2 weighting: intermediate intensity; enhanced T1 weighting: homogeneously hyperintense)
– Synovial proliferation/pannus of variable extent, possibly filling the entire joint cavity and osseous erosions with spherical soft-tissue lesions (Figs. 4.3 d–f, 4.6) (T1 weighting: intermediate intensity; T2 weighting: hyperintense; enhanced T1 weighting: homogeneous, strong enhancement = active; or T1 weighting: intermediate intensity; T2 weighting: heterogeneous, slightly hyperintense to intermediate hyperintense; enhanced T1 weighting: variable enhancement = less active; or T1 weighting: intermediate intensity; T2 weighting: intermediate intensity; enhanced T1 weighting: no enhancement = fibrous)
 Marginal subchondral bone-marrow edema as precursor of osseous erosion (six months to two years before manifested erosions), no correlating radiographic findings (!)
Marginal subchondral bone-marrow edema as precursor of osseous erosion (six months to two years before manifested erosions), no correlating radiographic findings (!)
 Erosion/destruction/cysts
Erosion/destruction/cysts
Therapeutic Principles
Conservative
Therapeutic principles
 Involvement of the shoulder is generally a manifestation of systemic disease
Involvement of the shoulder is generally a manifestation of systemic disease
 Systemic, “dynamic” therapy (depending on disease activity)
Systemic, “dynamic” therapy (depending on disease activity)
Therapy goals
 Causative therapy is so far not possible, only partial intervention in pathogenesis
Causative therapy is so far not possible, only partial intervention in pathogenesis
 Effect on pain and inflammation
Effect on pain and inflammation
 Maintenance of joint function
Maintenance of joint function
 Improvement of quality of life
Improvement of quality of life
Therapeutic modalities
 Systemic or local medication
Systemic or local medication
 Gymnastics
Gymnastics
 Physical therapy
Physical therapy
 Ergotherapy
Ergotherapy
 Surgery
Surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


