Inherited Metabolic Disorders
This section discusses a diverse group of disorders due to inborn errors of metabolism. Imaging is often suggestive of the general diagnosis, but rarely specific for the individual disease. White matter is usually involved, although this may be secondarily. In the chronic phase for each, these diseases share a similar imaging appearance, with atrophy and usually generalized white matter abnormality. The specific genetic defect for each disease, and often its many variants, is usually today well known. These have not been discussed in detail below, as they contribute little to image interpretation.
Diseases Affecting White Matter
Metachromatic Leukodystrophy
The most common form of this disease presents in the second year of life. The imaging appearance is nonspecific, with symmetric abnormal high signal intensity in the cerebral white matter on T2-weighted scans. This progresses temporally, together with generalized cerebral atrophy.
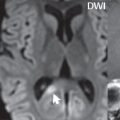
Krabbe Disease
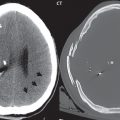
Clinical symptoms begin between age 3 and 6 months. Early features on imaging can be helpful for diagnosis, with involvement of the thalamus, caudate nucleus, and dentate nucleus, in addition to the more nonspecific involvement of the white matter of the corona radiata. In the nuclei, high density is seen on CT, with this finding preceding the generalized low-density in white matter. The thalami may be high signal intensity on T1-weighted scans early in the disease process, another useful finding for diagnosis if present. This leukodystrophy is often associated with enlargement of optic and cranial nerves.
X-linked Adrenal Leukodystrophy
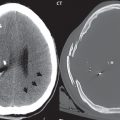
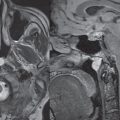
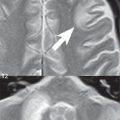
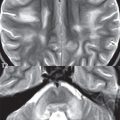
Of the many types of adrenoleukodystrophy, the childhood cerebral form is the most relevant and most common. This is a disease of young boys, with presentation between 5 and 12 years of age. Early clinical features include decreased visual acuity, gait disturbances, and mild intellectual impairment, with rapid disease progression. The most common imaging pattern is that of posterior white matter involvement, including specifically the periatrial (parieto-occipital) white matter, the fornix and the splenium of the corpus callosum. The pattern of spread is from posterior to anterior, as opposed to other leukodystrophies that extend from anterior to posterior (i.e., Alexander disease) ( Fig. 1.29 ).

As to be anticipated, these areas display low density on CT and increased signal intensity on T2-weighted MR scans. The anterior disease margin (the leading margin of demyelination) may display abnormal contrast enhancement, due to its inflammatory nature. In chronic disease, there is atrophy of the splenium. In 15% of patients, the pattern is predominantly frontal in location, with again abnormal contrast enhancement at the peripheral disease margin. In rare instances, the disease is predominantly unilateral.
Phenylketonuria
Imaging findings are nonspecific, with abnormal white matter hyperintensity on T2-weighted MR sequences due to delayed/defective myelination.
Maple Syrup Urine Disease
The classic form of this disease presents in the first few days of life. Profound edema is seen in regions of the brain that are normally myelinated at birth. There may be in addition generalized edema of the cerebral hemispheres.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree