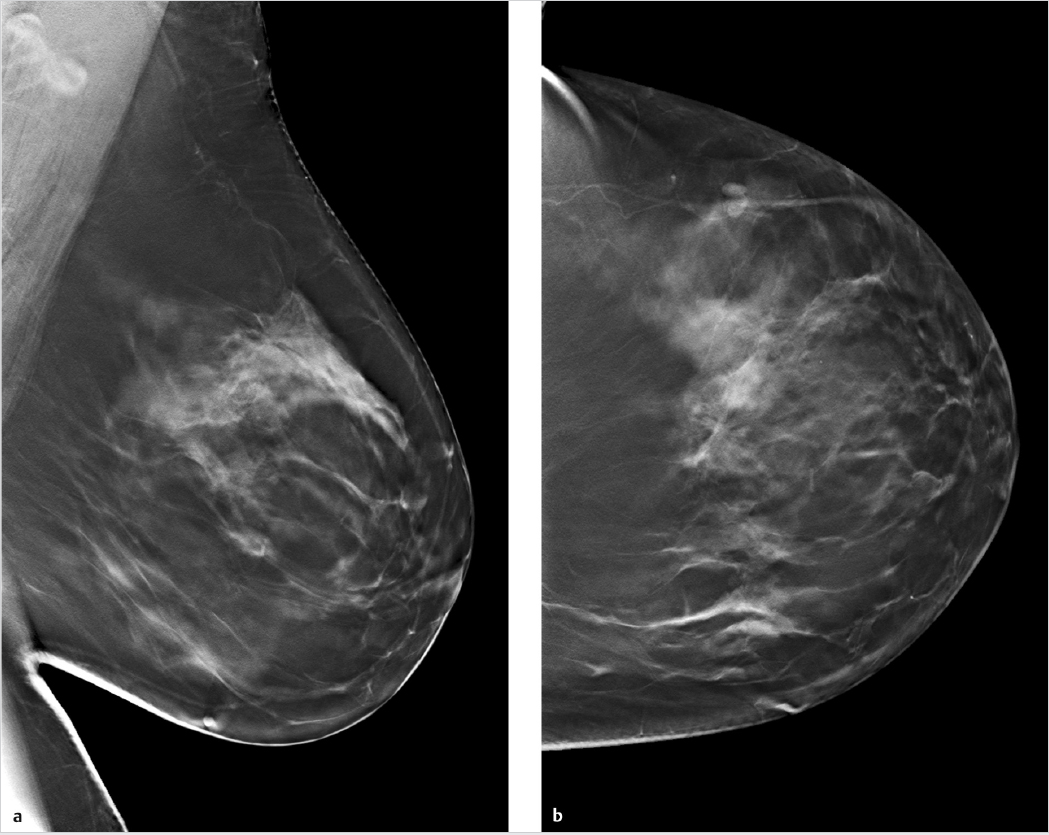
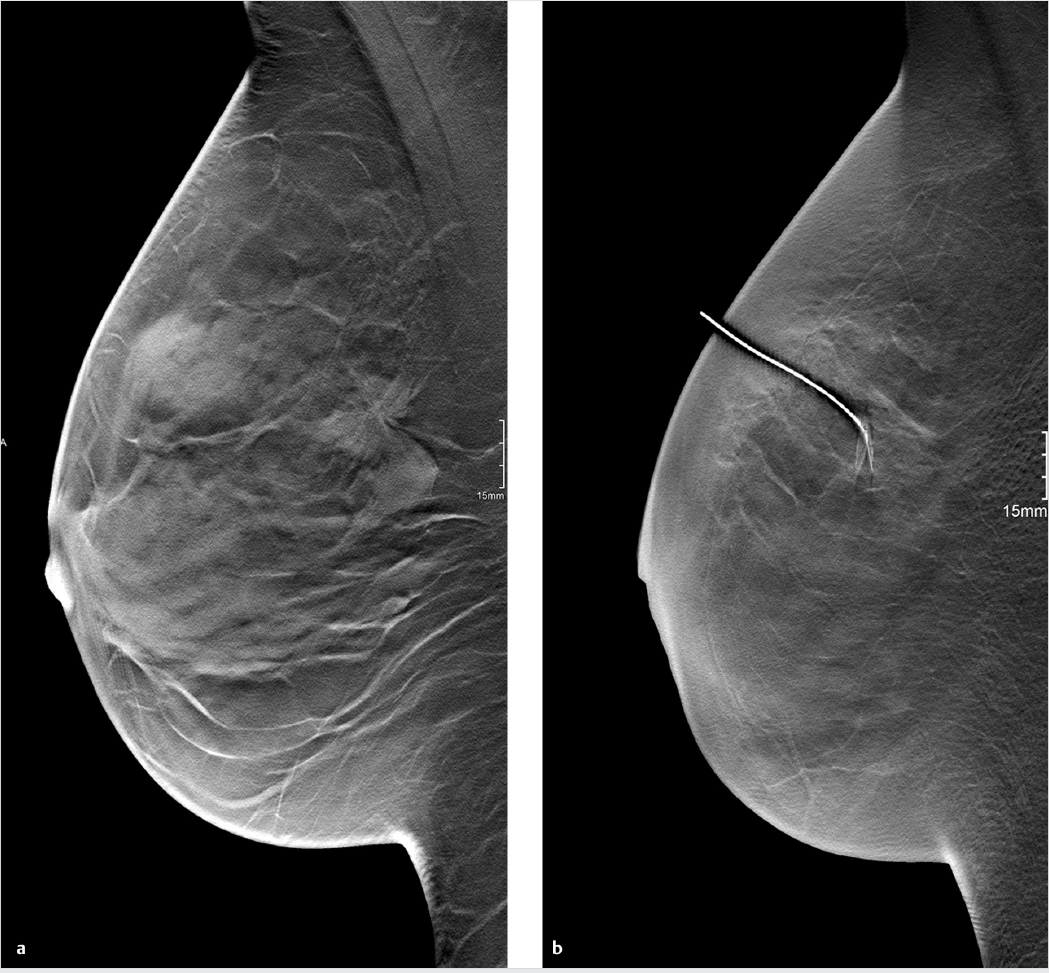
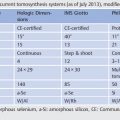
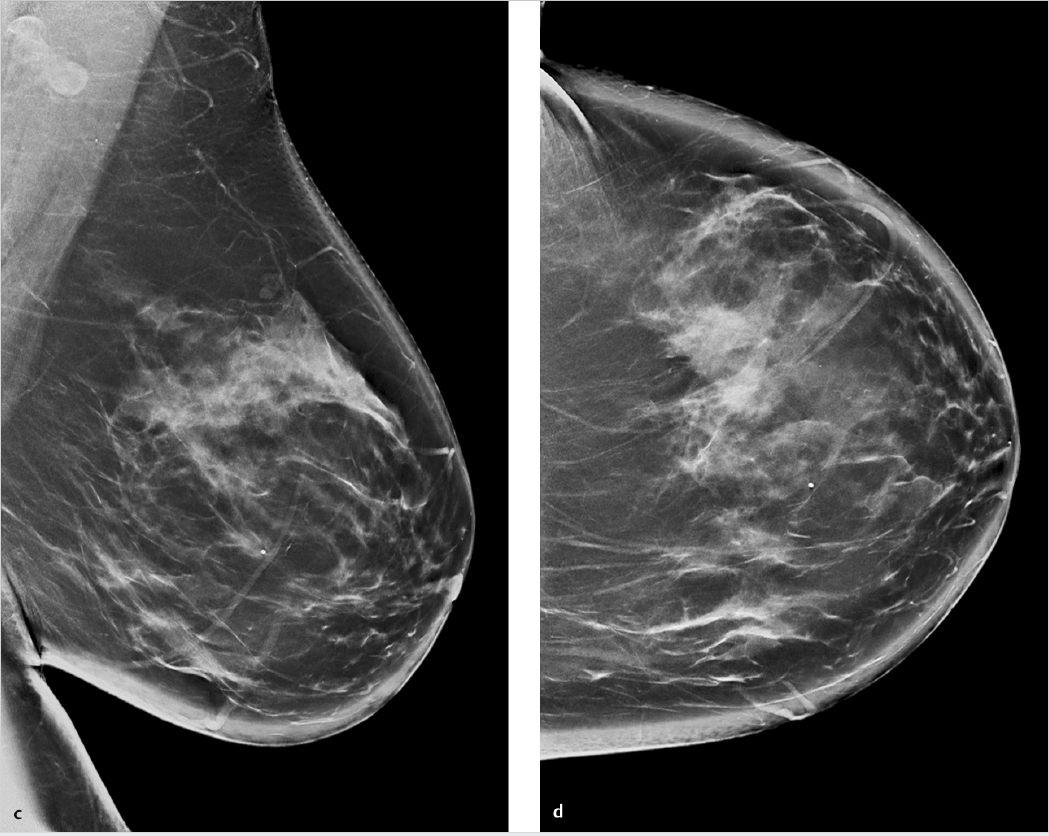
Chapter 4 4.2 Synthesized Digital Two-dimensional Mammography 4.3 Computer-aided Detection in Tomosynthesis 4.4 Tomosynthesis-guided Interventions 4.5 Contrast-enhanced Tomosynthesis Tomosynthesis is still a relatively new technology, and its technical evolution is far from complete. Compared to mammography, it still has great potential for advances in image reconstruction and postprocessing, as well as new clinical applications. Some of the techniques described in this chapter are still conceptual, some exist as prototypes, and some are already in clinical use. In all cases, however, the benefits of these techniques have not yet been adequately evaluated for routine clinical use, and it is still too early to draw definite conclusions. Fig. 4.1 Tubular breast cancer, confirmed histologically by core-needle biopsy. (Image data were provided courtesy of M. Sonnenschein, MD, Bern, Switzerland.) (a) 3D tomosynthesis of the left breast, mediolateral oblique (MLO) projection: 14-mm spiculated lesion at the 1o’clock position. (b) 3D tomosynthesis of the left breast, craniocaudal (CC) projection: 14-mm spiculated lesion at the 1 o’clock position. (c) Summation (c-view) image in the MLO projection, synthesized from the tomosynthesis data set. In overall appearance, the image closely resembles a conventional digital mammogram. (d) Summation (c-view) image in the CC projection, synthesized from the tomosynthesis data set. The image closely resembles a conventional digital mammogram. The spiculated mass is visualized but is more difficult to detect compared with 3D tomosynthesis. However, the image does facilitate comparison with prior images. New techniques are currently being developed for the reconstruction of conventional mammograms from a three-dimensional (3D) tomosynthesis data set (Fig. 4.1). Comparison of a 3D tomosynthesis data set and the corresponding slices with digital or even analog mammography poses a significant challenge. It is therefore desirable not only to reconstruct sectional images from the digital breast tomosynthesis (DBT) projections but also to generate a summation image that is comparable to a mammogram. With this technique, called synthesized digital two-dimensional (2D) mammography (“c-view”), both sectional images and mammograms for comparison with prior images can be reconstructed from a DBT data set, without additional radiation exposure. On initial viewing, the synthesized 2D image has a notably artificial appearance. The skin is markedly thickened in comparison with conventional mammograms, and this finding should not be mistaken for edema. There is also a marked accentuation of tissue contrasts, which may, for example, cause microcalcifications to appear more prominent. A first study on the performance of reconstructed 2D images in combination with DBT versus full-field digital mammography (FFDM) combined with DBT was published by Skaane et al in 2014.1 Using the most recent version of synthetically reconstructed 2D images, the cancer-detection rate was 7.8/1,000 for FFDM plus DBT versus 7.7/1,000 for reconstructed 2D images plus DBT, and the false-positive rate was 4.6% for FFDM plus DBT versus 4.5% for the current version of reconstructed 2D images plus DBT. The authors concluded that the combination of the current reconstructed 2D images plus DBT performed comparably to FFDM plus DBT and may be adequate for routine clinical use when interpreting screening mammograms.1 Computer-aided detection (CAD) systems for digital mammography have been in development for 20 years and have been commercially available for digital mammography for approximately 10 years. These systems cannot be applied to tomosynthesis without modifications, however: While the acquired image slices, with their extremely large data volumes, open new possibilities for image postprocessing, they also present new challenges. Thus, for detection of breast masses, CAD systems may work with projection images, reconstructed slices, or a combination of projection images and slices. A recent study used a CAD system focused on 2D images for mass detection in tomosynthesis.2 With this approach, it has proven helpful to assemble multiple DBT slices into a thicker slab, as this produces images that are more similar to standard mammograms. This algorithm was tested in 192 patients, and the best results were achieved with a slab thickness of 15 mm. Besides mass detection, CAD systems could also be used for characterization of lesions by methods such as volumetric segmentation. A prototype system of this kind is available and was successfully tested on experimental data sets.3 Adequate experience with clinical data sets is not yet available, however. CAD systems could also be used in tomosynthesis for the detection of microcalcifications. The first prototype software for this application was tested on 72 DBT data sets with histologically confirmed microcalcification clusters (17 cancers, 55 benign lesions). The study succeeded in developing a more advanced algorithm, but the average number of false positives was 3.4 per DBT data set, with a sensitivity of only 85%.4 This false-positive rate is still too high for clinical use.
Innovations and Future Developments
4.1 Introduction
4.2 Synthesized Digital Two-dimensional Mammography
4.3 Computer-aided Detection in Tomosynthesis
Radiology Key
Fastest Radiology Insight Engine