Abstract
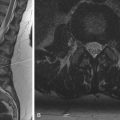
Interventional radiology (IR) is a radiologic subspecialty that uses imaging guidance to perform minimally invasive procedures on patients. Given that the focus of IR is treatment, rather than diagnosis, it is fundamentally different than other radiologic subspecialties. As such, the skills needed to care for patients in IR are unique. Moreover, the base of procedures in IR is expanding in both number and complexity, which introduces new patients with more difficult medical problems to the IR service. It is critical that the trainee have a firm grasp of the noninterpretive skills in IR to avoid patient harm. This chapter reviews core principles of patient management in IR, including safety culture, informed consent, conscious sedation, hemostasis, and complications.
Keywords
communication, conscious sedation, complications, Interventional radiology, patient safety, patient care
Safety Culture and Teamwork in Interventional Radiology
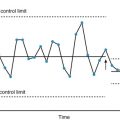
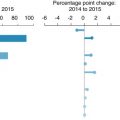
The practice of interventional radiology (IR) is distinct from that of diagnostic radiology (DR) in that IR is able to treat patients with a wide variety of vascular and nonvascular disorders. Inherent in these abilities is the responsibility to provide safe, evidence-based, and patient-centered care. One method of working toward this goal is creating a safety culture within the IR team. The safety culture requires a commitment at all levels of an organization, including hospital administration, physician leaders, physicians, managers, nursing, and technical staff. According to the American Board of Radiology, a safety culture encompasses these four features: (1) acknowledgement of the high-risk nature of an organization’s activities and the determination to achieve consistently safe operations, (2) a blame-free environment, (3) encouragement of collaboration across ranks and disciplines to seek solutions to patient safety problems, and (4) organizational commitment of resources to address safety concerns. There are several validated resources available that aim to measure the safety culture within an institution or team, such as the Agency for Healthcare Research and Quality Patient Safety Culture Surveys and the Safety Attitudes Questionnaire.
Even though an improved safety culture can enhance patient care and reduce medical errors, there is still considerable work to be done in achieving sustainable increases in safety culture and addressing heterogeneity in perceived safety culture among team members. One potential reason for this heterogeneity may be due to steep authority gradients , in which team members who view themselves as lower in the hierarchy are hesitant to raise patient safety concerns. Overcoming such obstacles necessitates a team-oriented approach in which the contributions of all team members are acknowledged and valued. Teamwork is a critical component during preprocedure preparation, procedure performance, and postprocedure care. Teamwork relies on open, respectful communication. This is particularly evident during the preprocedure checklist or time-out . The time-out immediately precedes the procedure and serves as the last defense against wrong site, wrong patient, and wrong procedure events. To eliminate these never events , the time-out and other communications need to extend beyond simply broadcasting information. Rather, effective communication is defined by its ability to eliminate uncertainty in the message’s recipients. All team members are encouraged to actively participate, raise concerns, and exchange information. When viewed from this perspective, communication depends on team members having shared mental models of not only the planned task but also its likely failure modes. High-performing teams will also share strategies for detecting and recovering from potential errors. As part of this preparation, the team anticipates communication errors and minimizes the impact of such errors through redundancy and closed feedback loops. For example, the use of multiple patient identifiers (name, date of birth, and/or medical record number) and reviewing the patient’s allergies illustrate how redundancy can reduce communication breakdowns. Reconciling the consent form with the referring physician’s order creates a feedback loop. Reviewing procedure-specific details such as plans for specimen handling, preprocedure antibiotics, and needs for special equipment and supplies serves to get the entire team on the same page.
A second barrier in achieving a safety culture is the tendency to blame individuals. In a culture of individual blame, excessive emphasis is placed upon the person who makes the error rather than focusing on the contributive systemic and environmental factors. This approach to patient safety often results in punitive or corrective actions toward the individual team member. Unfortunately, this has the untoward effect of making team members less likely to report mistakes and raise concerns. If errors are underreported, then the team misses an opportunity to address systemic patient safety issues, which increases the likelihood that the error will be repeated in the future. Therefore, when considering medical errors within a culture of safety, it becomes necessary to distinguish between active errors (mistakes that occur at the point of contact between a caregiver and patient, e.g., performing a percutaneous biopsy on the wrong kidney) and latent errors (systemic, design, or organizational failures that contribute to adverse events). However, it should be recognized that there are certain situations in which the specific actions of an individual team member need to be addressed. Therefore, the concept of a just culture has been introduced. A just culture does not punish team members when their actions are commensurate with their experience and training but does hold them accountable for negligent or reckless behavior. In a just culture, it is critical to distinguish human errors (also referred to as slips or mistakes) from at-risk behavior (e.g., not placing sharps within the appropriate container on the procedure table) from reckless behavior (e.g., proceeding with central line placement without performing the required time-out). In this model, any punitive measures to the individual would be based upon the type of behavior exhibited rather than the severity of the event or whether a patient was actually harmed by the incident.
Preprocedural Care
Many of the noninterpretive skills necessary for IR occur before the patient ever enters the procedure suite. It is crucial that the interventionalist approaches each case with a thorough patient assessment including an evaluation of the patient’s history, physical exam findings, imaging data, and review of pertinent laboratory values. The initial interaction between the IR service and the referring team should be viewed as a request for a consultation rather than an order for a procedure. As consultants, the IR team adds value to the patient’s care. Such an approach will maximize the opportunities for success while minimizing the possibility of errors. Moreover, it allows the interventionalist a chance to determine the appropriateness of the requested procedure. In some instances, it may be necessary to offer an alternative treatment from that which was originally requested. The following section discusses several subsequent aspects of preprocedural care including determining the appropriateness of the procedure, establishing realistic patient expectations, planning for pain control and sedation, managing coagulation status, and obtaining informed consent.
Appropriateness
After gathering basic information about the patient’s needs, the next question is whether the patient’s condition might be best addressed by an image-guided procedure. This requires an understanding of the indications for the procedure as well as the identification of any potential contraindications. Certainly, it would be beyond the scope of the present chapter to adequately address all the indications and contraindications for the wide variety of procedures performed in IR. However, the American College of Radiology (ACR) has developed a set of guidelines, called the ACR Appropriateness Criteria, that can act as a valuable resource when trying to determine the correct course of action for a particular patient. These guidelines have been developed over the past 20 years by task forces consisting of recognized experts. The panels include radiologists and nonradiologists. The guidelines are meant to be seen as living documents that can change with new scientific discoveries. The Appropriateness Criteria are divided into 10 clinical imaging topics (breast, cardiac, gastrointestinal, musculoskeletal, neurologic, pediatric, thoracic, urologic, vascular, and women’s), which are divided into clinical conditions, then further subdivided into variants of clinical conditions. The panel then uses the best scientific evidence available and, if lacking, expert opinion to determine the appropriateness of an intervention according to each clinical condition on a scale of 1 to 9. Ratings of 1 to 3 are defined as “usually not appropriate,” 4 to 6 as “may be appropriate,” and 7 to 9 as “usually appropriate.” The panel may also opt to indicate that no consensus was reached. In a similar fashion to the Appropriateness Criteria, the ACR has also generated several Practice Parameters and Technical Standards documents that aim to give medical providers guidance toward best practices for their patients. Per the ACR, Practice Parameters describe recommended conduct in specific areas of clinical practice, whereas Technical Standards describe technical parameters that are quantitative or measureable. Importantly, when applying any guideline, one must remember that each individual patient and situation is unique and a one size fits all approach may not be optimal for patient care. It is vital that differences in training and experience in addition to local practice patterns be taken into account when determining the appropriateness of any given treatment.
Establishing Reasonable Expectations
The interventionalist then needs to review the planned procedure with the patient. This conversation provides an opportunity to establish a rapport with the patient. Such discussions can have a marked impact on the perceived quality of care because patients tend to judge the quality of their healthcare experience by whether it met or exceeded expectations. Patient expectations vary widely, and time spent discussing reasonable predictions about when the procedure will occur, how long it might take, and its impact on the patient’s condition is almost always time well spent. This conversation also touches on topics needed to complete the informed consent process, which are discussed later in this chapter.
Pain Control and Sedation
A chief concern for many patients is whether the procedure will be painful. The preprocedure discussion is an opportunity to gauge the patient’s needs for analgesia and anxiolysis. This includes the patient’s ability to tolerate proper positioning during the procedure. For example, a patient with compromised respiratory status may not be able to lie flat on the table for an extended period of time. Some situations may require the involvement of an anesthesiologist. This process is facilitated by familiarity with the American Society of Anesthesiologists (ASA) physical status classification score ( Box 24.1 ). Patients who classify as ASA I or ASA II should qualify as candidates for sedation. Patients who are classified as ASA III or ASA IV may require further consideration before sedation, which could potentially include a formal consultation with an anesthesiologist. Patients who are classified as ASA V or above should not be sedated without the assistance of an anesthesiologist. The Joint Commission (TJC) and ASA have described four levels of sedation, including minimal sedation, moderate sedation, deep sedation, and general anesthesia ( Box 24.2 ). Most procedures in IR are performed with minimal or moderate sedation. Prior to administering sedation medications, one must inquire about the patient’s NPO (nothing by mouth) status (most institutions require patients to be NPO for 6–8 hours to receive sedation), medication allergies, ability to protect his or her own airway (patients who are at significant risk for aspiration may require general anesthesia for airway protection during their procedure), and any history of obstructive sleep apnea (these patients may require continuous positive airway pressure during their procedure).
Class I: Normal healthy patient
- •
Example: Pheresis catheter placement in a healthy stem cell donor
Class II: Patient with mild systemic disease
- •
Example: Percutaneous abscess drain placement in a child for appendicitis
Class III: Patient with severe systemic disease
- •
Example: Chemoembolization of liver cancer in a cirrhotic patient
Class IV: Patient with severe systemic disease that is a constant threat to life
- •
Example: Thrombectomy and thrombolysis of a clotted dialysis graft in a patient with fluid overload, compromised respiratory status, and end-stage renal disease
Class V: Moribund patient that is not expected to live without the procedure
- •
Example: Splenic angiography and embolization in an unconscious, hypotensive patient with a grade IV splenic laceration after a motor vehicle collision
Class VI: Brain-dead patient being evaluated for organ transplant
Minimal Sedation
- •
Patient responds to verbal commands
- •
Cognitive function and coordination may be impaired
- •
Ventilatory and cardiovascular functions are intact
- •
Achieved with oral or intravenous medications
Moderate Sedation
- •
Minimal depression in the level of consciousness
- •
Patient retains protective reflexes, maintains a patent airway, and has the ability to be aroused by physical or verbal stimulation
- •
Achieved with intravenous medications
Deep Sedation
- •
Depression of consciousness
- •
Patients cannot be easily aroused but respond purposefully to repeated or painful stimuli
- •
Patient’s ventilatory function and airway may be compromised but cardiovascular function is maintained
- •
Usually requires involvement of an anesthesiologist
General Anesthesia
- •
Controlled state of unconsciousness
- •
Complete loss of protective reflexes
- •
Do not respond appropriately to painful stimuli
- •
Requires involvement of an anesthesiologist
Coagulation Status and Hemostasis Risk
Coagulopathies and the use of anticoagulating medications represent one of the most commonly encountered contraindications to image-guided procedures in current practice. Thus, it is imperative that the interventionalist have a general idea about how to manage this complex issue, especially with the ever-increasing number of newer anticoagulants that are coming on the market. The Society of Interventional Radiology (SIR) has established practice guidelines for managing the coagulation status of patients undergoing image-guided interventions, which classifies procedures based on the anticipated bleeding risk ( Table 24.1 ). The SIR has also issued guidelines regarding the use of anticoagulant and antiplatelet medications. The following are general guidelines:
- 1.
A heparin infusion should be stopped or reversed when the activated partial thromboplastin time is 1.5 times normal.
- 2.
One dose of low-molecular-weight heparin should be held for low- to moderate-risk bleeding procedures, and low-molecular-weight heparin should be held for 24 hours for high-risk procedures.
- 3.
It is advisable that patients on warfarin have international normalized ratios within accepted limits (see Table 24.1 ) prior to the procedure.
- 4.
Clopidogrel should be held for 5 days prior to elective procedures although a platelet transfusion may be appropriate in urgent or emergent circumstances.
- 5.
Aspirin needs to be held for 5 days for high-risk procedures only.
- 6.
Newer oral anticoagulants such as rivaroxaban should be stopped 1 to 2 days prior to the procedure.
| Low Risk | Moderate Risk | High Risk | |
|---|---|---|---|
| Target Lab Values | |||
| INR | ≤2.0 | ≤1.5 | ≤1.5 |
| Platelets (in K/mm 3 ) | ≥50 | ≥50 | ≥50 |
| Examples | |||
| Vascular | Dialysis access interventions, venography, central line removal, peripherally inserted venous catheter line placement, inferior vena cava filter placement | Angiography, venous interventions, chemoembolization, uterine fibroid embolization, transjugular liver biopsy, tunneled central venous catheter placement, port placement | Transjugular intrahepatic portosystemic shunt |
| Nonvascular | Catheter exchanges, thoracentesis, paracentesis, superficial aspirations and drainages, superficial biopsy | Intraabdominal or chest wall drainage or biopsy, lung biopsy, transabdominal liver biopsy, cholecystostomy tube, gastrostomy tube, radiofrequency ablation, spinal procedures | Renal biopsy, biliary interventions, nephrostomy tube placement, complex radiofrequency ablations |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree