Fig. 3.1
Longitudinal section of descending colon in patient with left-sided active ulcerative colitis shows thickened bowel walls characterized by stratified echopattern and absence of haustra coli

Fig. 3.2
Transversal ultrasonographic section of sigmoid colon in patient with quiescent ulcerative colitis. The stratified echopattern of the bowel wall is preserved and the thickness is within the normal values
In active ulcerative colitis, the thickness of the bowel wall is usually homogeneous and continuous, circumferential and symmetrical. It predominates in the left colon, it is easily detectable in the hypogastrium and extends throughout the entire colon in extensive colitis and in pancolitis.
In active and extensive disease, the bowel wall usually shows a stratified echopattern with loss of haustra coli. In acute colitis, the thickening involves the submucosa which may also appear slightly hypoechoic and dyshomogeneous, sometimes with loss of stratification and increased vascularity at colour Dopper. The muscularis propria, normally imaged as an external hypoechoic line, is preserved, and therefore the external profiles of the colonic wall in ulcerative colitis are usually linear and regular. Unlike Crohn’s disease, ulcerations are usually superficial and not detectable by ultrasound and therefore in mild to moderate active ulcerative colitis, the inner layers of the colonic wall are usually regular. However, severe ulcerative colitis is characterized by markedly thickened and hypoechoic bowel walls (Fig. 3.3), sometimes with irregular inner layer and small linear hyperechoic spots representing deep penetrating ulcers of the submucosa. The bowel ultrasound can also suggest the presence of toxic megacolon when severely thickened and hypoechoic bowel wall in the left colon, associated with marked dilatation (>6 cm) of the transverse colon characterized by decrease in bowel wall thickness (<2 mm), and presence of increased fluid and dilation of the ileal loops, are found (Fig. 3.4a and b) [4]. However, it should be acknowledged that ultrasound plays only a supportive role in this clinical context, which is still marginal in comparison to the plain abdominal radiography that is the reference investigation.

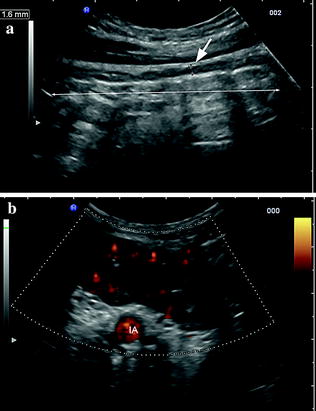

Fig. 3.3
Longitudinal ultrasonographic section of transverse colon in patients with severe ulcerative colitis showing thickened and hypoechoic bowel wall
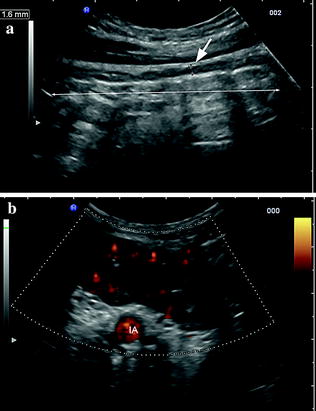
Fig. 3.4
Ultrasonographic findings in ulcerative colitis patient with impending toxic megacolon. a Thin hypoechoic bowel wall (short arrow) and dilated transverse colon (long arrow). b Longitudinal section of the sigmoid colon of the same patient showing thickened hypoechoic and hypervascularised bowel walls. IA, iliac artery
In quiescent ulcerative colitis, in particular in patients with previous several recurrences, as well as in some cases with mild inflammation, the colonic wall shows normal or only slight thickening with a predominant echogenic submucosa contrasting with the hypoechoic inner mucosa and outer muscularis (Fig. 3.5).


Fig. 3.5
Longitudinal ultrasonographic section of descending colon in patient with quiescent ulcerative colitis showing slight thickening of the bowel wall with preserved stratified echopattern and predominant echogenic submucosa (asterisks)
In ulcerative colitis patients with pseudopolyposis, small echogenic hypoechoic nodules may be observed at the surface of the mucosa (Fig. 3.6). These may be isolated and well appreciable into the fluid-filled intestinal lumen, also by using hydrocolonic sonography. Extensive pseudopolyposis appears as an increased and inhomogeneous thickness of the bowel wall (up to 15 mm), without the typical bowel wall stratification (also in quiescent ulcerative colitis), markedly irregular internal margins and/or as a dilated incompressible bowel with echogenic inhomogeneous content. The colour Doppler can be used to obtain confirmation of the pseudopolypoid nature of the intestinal content, assessing the blood flow within the echogenic material.


Fig. 3.6
Ulcerative colitis patients with pseudopolyposis. Longitudinal scan of the descending colon showing small echogenic hypoechoic nodules (asterisks) within the lumen
3.4 Diagnostic Accuracy
Bowel ultrasound has been demonstrated to be a reliable tool for diagnostic purposes, to assess disease extension and activity in ulcerative colitis, thus providing important information if endoscopy is incomplete or contraindicated, and also to predict the outcome of disease after therapy (Table 3.1).
Table 3.1
Indications and potential usefulness of bowel ultrasound in UC
Early evaluation of patients with suspected ulcerative colitis |
|---|
Evaluation of extension |
Assessment of activity |
Assessment of response to therapy |
Long-term prediction of outcome (relapse/remission) |
Diagnosis of abdominal complications |
–Toxic megacolon |
–Pseudopolyposis |
Differential diagnosis in chronic inflammatory colitis |
3.4.1 Detection of Ulcerative Colitis and Assessment of Disease Activity
The studies carried out in adults, which have adopted the bowel wall thickness >4 mm as criterium for abnormality, have shown that transabdominal ultrasound has a median of 76 % (range: 53–89 %) in detecting ulcerative colitis [5–12]. The sensitivity in assessing ulcerative colitis is lower than that reported to assess other inflammatory bowel diseases, such as Crohn’s disease or diverticulitis. This may be explained by the fact that inactive ulcerative colitis or disease characterized by mild inflammation has frequently normal bowel wall thickening (<4 mm) and when the disease activity is confined to the rectum, it is difficult to assess by transabdominal ultrasound .
Several studies have shown that the degree of bowel wall thickening correlates well with clinical activity [7, 8, 13–17], biochemical (namely C-reactive protein and erythrocyte sedimentation rate values) [14, 15, 18], endoscopic [14, 16, 18, 19] and scintigraphic activity [13] of ulcerative colitis.
3.4.2 Evaluation the Anatomical Extension
Bowel ultrasound has been proved to be of value in evaluating the anatomical extension of the inflammation during disease flare-up. In particular, the technique has a very high sensitivity in detecting left-sided colitis, although it has low sensitivity in identifying proctitis [10]. For these reasons, bowel ultrasound may be a valid alternative to invasive procedures in assessing the extension of ulcerative colitis, provided that the disease is active (e.g. bowel examination should be performed only during flare-up of the disease) and is not limited to the rectum (e.g. bowel examination may be negative in patients presenting without diarrhoea and only with rectal bleeding).
3.4.3 Response to Therapy and Outcome
Bowel ultrasound may evaluate the response to medical treatment in active ulcerative colitis and predict relapses of the disease [13, 14]. In severe ulcerative colitis, it has been shown that the absence of significant decrement in wall thickness from baseline, shortly after a course of therapy (high-dose steroid therapy or cytapheresis), is associated with a high risk of endoscopic relapse at 1 year [19–22].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree