INTRACONAL ORBIT: VASCULAR MALFORMATIONS
KEY POINTS
- Computed tomography and magnetic resonance imaging in combination are the primary tools, as opposed to biopsy, for establishing the diagnosis of orbital vascular malformations.
- Computed tomography and magnetic resonance imaging are in the critical pathway for evaluating the cause of a visual loss that might be due to compression or other involvement of the optic nerve and sheath.
- Computed tomography and magnetic resonance imaging are extremely useful for posttreatment surveillance or as a follow-up tool when a “watchful waiting” strategy is adopted.
Any orbital mass or disease process may be approached by first establishing whether it is preseptal (Chapters 70 and 71) or postseptal (Chapters 57–60, 62, and 64). If postseptal, it should be established as a process arising primarily intraconally (Chapters 57–60), extraconally (Chapters 62 and 64), or transcompartmentally. If intraconal, it should be decided whether the mass is of optic nerve/sheath origin or arises from some other structure comprising or within the muscle cone. This chapter considers intraconal vascular malformations and those arising intraconally and spreading across the orbital compartments and related spaces.
These are most often spontaneous developmental abnormalities that are a common explanation of an intraconal mass; there may also be an extraconal component. These are most often some variety of venolymphatic malformation, most commonly a well-encapsulated “hemangioma” likely more properly referred to as a cavernous malformation as discussed in Chapter 9. True proliferative (infantile) hemangiomas arising in the muscle cone are very uncommon. Occasionally, especially if bilateral or associated with intracranial findings, malformations may be syndromic. Orbital varix is included in this developmental group of diseases.
Acquired vascular malformations of the orbit are most often posttraumatic and to some extent will manifest in the intraconal compartment as secondary changes of vascular congestion and venous distension due to a cavernous carotid fistula (CCF). The pathophysiology of a CCF and other fistulas is discussed in Chapter 75; their pathologic changes in contrast to other malformations are discussed in Chapter 9.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
The embryology of congenital origin vascular malformations is discussed in Chapter 9.
Applied Anatomy
The relevant anatomy of the orbit, eye, and optic nerve/sheath complex is discussed in detail in Chapter 44. In particular, the anatomy of the arteries and veins of the eye and orbit should be reviewed.
IMAGING APPROACH
Techniques and Relevant Aspects
The orbit, eye, and optic nerve and sheath are studied with ultrasound (US), computed tomography (CT), and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. Specific CT protocols by indications are detailed in Appendix A. Specific MR protocols by indications are outlined in Appendix B. Almost all studies to investigate intraconal pathology and in particular vascular malformations are done with contrast.
If an orbital varix is suggested, a CT scan might be done with a provocative maneuver such as Valsalva. Alternatively, CT or magnetic resonance imaging (MRI) may be done with the patient face down to provoke filling of the varix.
Pros and Cons
The use of US is for the most part restricted to the identification of a swollen optic disc and possible intraocular complications of disease primarily within the muscle cone. US may show findings immediately adjacent to the nerve–globe junction and around the distal sheath that marginally contribute to the differential diagnosis.
Disease of and within the muscle cone is studied primarily with CT and MRI. MRI is far more definitive in its rendering of the optic nerve and ocular effects of such disease and providing objective evidence of secondary optic nerve compromise. MRI may be more sensitive than CT to possibly related intracranial involvement with these vascular lesions.
CT may be used primarily in very acute situations when the clinical presentation mimics an aggressive infectious process or tumor perhaps with a sinonasal origin. CT may also be done first for an emergent evaluation of possible associated tension orbit (Figs. 9.6 and 48.5). CT is also a first choice in patients too sick or for some other reason unable to complete a very high quality, free of motion artifact, MRI examination. CT is a reasonable secondary screening tool for identifying intracranial extension of disease and intracranial complications. Computed tomographic angiography is a good and perhaps preferred screening tool to search for vascular complications such as aneurysms and cavernous sinus thrombosis.
SPECIFIC DISEASE/CONDITION
Vascular Malformations
Etiology
Vascular malformations (Chapters 9 and 75) may be either congenital or acquired; the latter are usually due to trauma. These are generally sporadic, but if bilateral they may be syndromic. The best known of the syndromic variety is the Wyburn-Mason syndrome (Figs. 9.3, 9.4, and 59.1). This consists of a high-flow arteriovenous (AV) malformation extending from the orbit and retina along the anterior visual pathways to the midbrain. Klippel-Trenaunay-Weber syndrome may be associated with venous angiomata of the orbit (Figs. 9.3 and 9.4); this syndrome can involve the kidneys and other viscera.1 Sturge-Weber and von Hippel-Lindau syndromes may also be associated with vascular abnormalities of the eye; these were discussed in Chapters 9 and 52 (Figs. 9.21 and 52.2).
Prevalence and Epidemiology
These factors are discussed in Chapter 9.
Clinical Presentation
Localized intraconal lesions will usually present with painless proptosis. The orbital lesions sometimes seen in Wyburn-Mason syndrome are usually associated with similar retinal “racemose hemangiomas,” and these patients can present with loss of vision. Transcompartmental lesions may present as a palpable or visible mass or because they too cause proptosis, interfere with eye motion, or cause a compressive optic neuropathy2–8 (Figs. 9.22, 59.2, and 59.3A). Vascular malformations may bleed, thrombose, or become infected or react to an infection, in which case pain and inflammation and rapid enlargement may mimic an infectious or neoplastic lesion (Figs. 59.3B,C and 59.4). They may be discovered incidentally on imaging findings done for other reasons3 (Figs. 59.5–59.7).
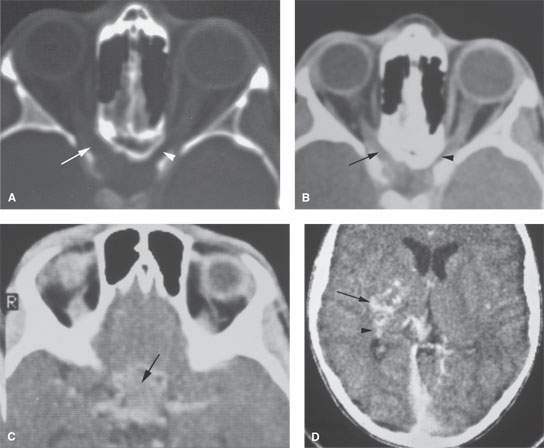
FIGURE 59.1. Contrast-enhanced computed tomography (CT) study of a patient with a vascular malformation at the orbital apex and extending along the posterior visual pathways. A: There is widening of the optic canal on the right (arrow) compared to the normal left side (arrowhead). B: Soft tissue views show enhancing tissue within the optic canal (arrow) compared to the normal side (arrowhead), but the nature of the abnormality is uncertain. There is no obvious enlargement of the vessels within the orbit. C: There is an enhancing abnormality within the suprasellar cistern (arrow). The nature of this is not entirely certain based on this image. D: CT image showing a vascular malformation (arrow) extending posteriorly to the region of the lateral geniculate body (arrowhead).
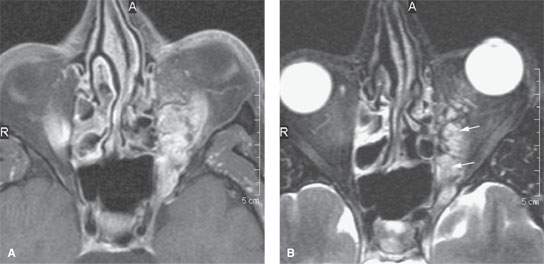
FIGURE 59.2. Magnetic resonance imaging of a patient with a transcompartmental venolymphatic malformation of the orbit. A: T1-weighted fat-suppressed images show this to be mainly composed of vascular blood pools. B: T2-weighted image with fat suppression shows the vascular spaces to be relatively static, as suggested by their brightness on this image (arrows).
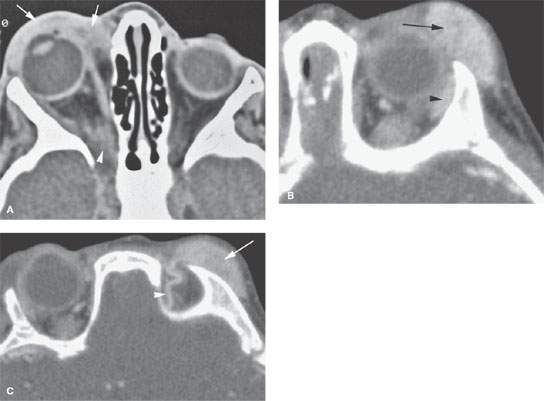
FIGURE 59.3. Two pediatric patients with vascular abnormalities. A: Contrast-enhanced computed tomography (CECT) study of Patient 1 presenting with acute onset of periorbital swelling. The preseptal, mainly vascular component of the vascular malformation swelled acutely due to inflammation (arrows). The component at the orbital apex is shown to be less vascular (arrowhead). The chronic nature of the lesion has resulted in widening of the superior orbital fissure. B, C: CECT study of Patient 2 presenting with a palpable subcutaneous supraorbital mass and abnormal eye movements. In (B), this proliferative (infantile) hemangioma involves the preseptal soft tissues (arrow) and is indistinguishable from the orbital portion of the lacrimal gland (arrowhead). In (C), the mass (arrow) does not extend significantly into the orbit, as was questioned clinically. The large draining vein (arrowhead) is a fairly characteristic feature of a proliferative hemangioma.

FIGURE 59.4. Two patients with complicated venolymphatic malformations. A, B: A patient presenting with acute onset of proptosis on the left. In (A), the contrast-enhanced T1-weighted (T1W) image shows an intraconal venolymphatic malformation surrounding the optic nerve/sheath complex (arrow) and displacing and distorting other structures within the muscle cone (arrowheads). In (B), the T2-weighted (T2W) axial image shows the cystic-appearing intraconal mass to contain a fluid–fluid level (arrow) due to hemorrhage that resulted in the rapid onset of proptosis. C–F: A 10-month-old boy, with a known orbital vascular malformation causing slight exophthalmos, retraction of the eyelid, and epiphora, developed swelling of the cheek. In (C) and (D), sagittal and axial T2W images reveal an intraconal, extraconal, preseptal, and extraorbital mass with fluid–fluid levels within the temporal muscle fascia (*) and a central bright area (arrowhead) surrounded by very low signal intensity in the intraconal component, suggestive of hemorrhage in evolution. Within the extraconal/preseptal portion, septae seem to be present (arrows). The lesion causes displacement of the optic nerve without any functional loss of the nerve. In (E), on T1 weighting, an area of high signal intensity is seen centrally in the intraconal component (arrow), whereas the remainder of the lesion shows intermediate signal intensity (arrowhead) probably due to a fibrous matrix or blood vessel component. In (F), postcontrast variable enhancement of the venolymphatic malformation is seen. The most prominent enhancement is seen in the intraconal component, surrounding the central blood clot in evolution.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








