KEY FACTS
Terminology
- •
Intraductal papillary mucinous neoplasm: Mucin-producing cystic tumor arising from main &/or branch pancreatic ducts with low malignant potential
- •
Previously called: Intraductal papillary mucinous tumor, duct ectatic mucinous cystadenoma, mucinous hypersecretory neoplasm, mucin-producing tumor
- •
Cystic neoplasm of pancreas arising from mucin-producing epithelium of main pancreatic duct (MPD) &/or side branch pancreatic ducts (SBD) with variable malignant potential
Imaging
- •
US: Not modality of choice: Difficult to evaluate entire pancreas due to bowel gas and limited characterization
- •
MPD type: Dilated MPD > 5 mm, may contain low-level internal echoes (mucin vs. mural nodule); without obstructive mass
- •
SBD type: Multicystic, grape-like cluster of anechoic or hypoechoic masses; may see communication with dilated pancreatic duct
- •
Mixed type: Findings of both types
- •
Typically in head/uncinate
- •
May be multiple (21-40%); entire pancreas in up to 20%
- •
Endoscopic US (EUS): Provides best morphologic evaluation and opportunity for cyst aspiration &/or biopsy
- ○
Higher spatial resolution than transabdominal US; can depict internal septations, mural nodules, wall thickening
- ○
- •
CT or MR: Important in identifying features associated with increased risk of malignancy
- •
MRCP: Best noninvasive imaging modality for identification of ductal communication
- •
Follow-up surveillance imaging with CEMR/MRCP
Top Differential Diagnoses
- •
Pancreatic pseudocyst
- •
Chronic pancreatitis
- •
Mucinous cystic pancreatic neoplasm
- •
Pancreatic serous cystadenoma
- •
Pancreatic ductal adenocarcinoma
Pathology
- •
Main duct type: Precursor to invasive ductal carcinoma
- •
Branch duct type: Generally benign, low malignancy risk
Clinical Issues
- •
Mean at diagnosis: 68 years; range: 60-80 years; M > F
- •
Nausea/vomiting, abdominal pain, weight loss, anorexia
- •
MPD type may result in pancreatitis
- ○
From obstruction secondary to excess mucin production
- ○
- •
Tanaka criteria (update to Sendai classification): Classifies intraductal papillary mucinous neoplasm as high risk, worrisome, or low risk based on imaging features in order to guide treatment decisions
- •
If high-risk stigmata present based on Tanaka criteria → surgical resection
- •
If worrisome features present → EUS for biopsy/aspiration
- •
If no worrisome features present → follow-up interval determined by cyst size
Scanning Tips
- •
Look for communication between cystic lesion and pancreatic duct, which may be dilated

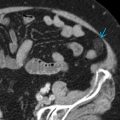
 . Splenic vein
. Splenic vein  is also noted.
is also noted.
 communicating with a dilated main pancreatic duct
communicating with a dilated main pancreatic duct  .
.
 , some of which show communication with the mildly dilated main pancreatic duct
, some of which show communication with the mildly dilated main pancreatic duct  .
.