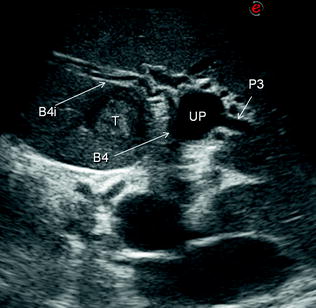
Fig. 9.1
IOUS can provide anatomical details of the intrahepatic biliary tree even if not dilated, with details of its centripetal bifurcation pattern: in a single scan one can recognize the right bile duct (RBD), the one draining the right anterior (B5-8), the one draining the right posterior (B6-7), the left bile duct (LBD), and the duct draining segment 4 (B4), while only the right portal vein (RPV) is to be seen
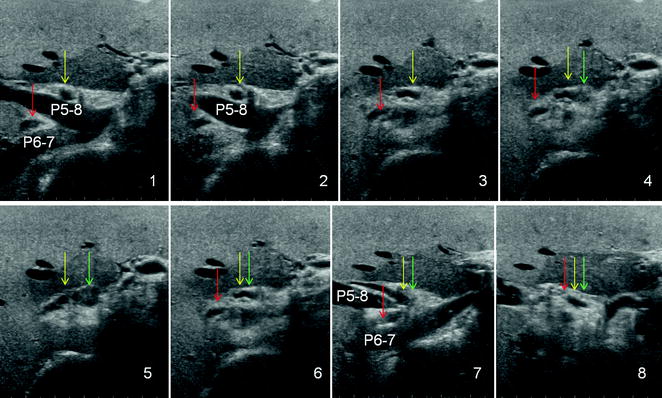
Fig. 9.2
IOUS images from 1 to 8 show how in this patient the right anterior bile duct (B5-8 indicated by yellow arrow) is flowing into the left bile duct (green arrow) which together meet the right posterior bile duct (B6-7 indicated by red arrow) in frame number 8; portal branch to the right anterior section (P5-8); portal branch to the right posterior section (P6-7)
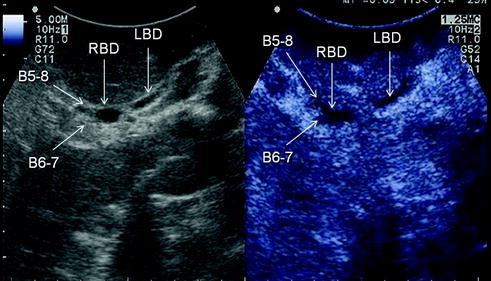
Fig. 9.3
On the left, IOUS of the intrahepatic biliary confluence showing the right anterior bile duct (B5-8), the right posterior bile duct (B6-7), the right (RBD) and the left bile ducts (LBD), and, on the right, the same scan by CEIOUS
1.
resection guidance for biliary tumors;
2.
providing details about the integrity of the intrahepatic biliary tree after a resection; and
3.
proper drainage of the bile duct stump.
9.2 Resection Guidance for Biliary Tumors
Concerning resection guidance, with the exclusion of the mass-forming type of cholangio-carcinoma for which the role of IOUS guidance is similarly relevant as for CLM, the above-mentioned limitations are actually real and linked to the features of the target. Indeed, perihilar cholangiocarcinomas are generally isoechoic (see Chap. 4), and thus less visible even by IOUS (Fig. 9.4a). However, more important, these tumors tend to expand within the bile duct wall frustrating any attempt to disclose the real tumor margin in a reliable way (Fig. 9.4b), and thus accounting for the still considerable rate of palliative resections [5]. This limitation together with the low visibility of the main lesion impacts also the capability of IOUS to disclose an eventual vascular encasement by the tumor (Figs. 9.4c–e, 9.5a, b), which accounts for the need of extemporary vascular reconstruction, in spite of the encouraging results of such a policy [5]. However, as IOUS can recognize the intrahepatic biliary tree anatomy, it can also play a role in avoiding its damage by providing fundamental information for planning the surgical strategy (see Chap. 7) or guiding the liver dissection (see Chap. 8) (Fig. 9.6a–g). Another aspect which is relevant both for planning the surgical strategy and guiding the resection is its ability of reveal even minimal bile duct dilation: this is particularly the case for tumor-vessel relationships for establishing the risk of tumor invasion of the glissonian sheath, and, as a consequence, the need for its resection and for the extension of the resection area according to the criteria mentioned earlier [6] (see Chap. 7). IOUS allows the precise definition of this occurrence in patients with tumors in contact with an intrahepatic glissonian sheath (Fig. 9.7) but also its exclusion (Figs. 9.8, 9.9).
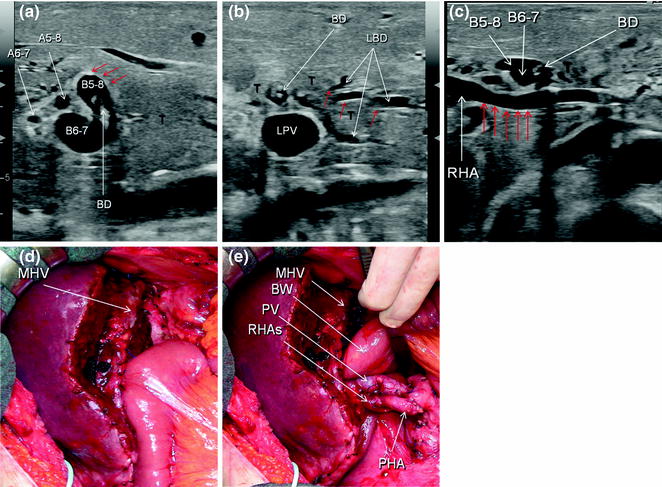
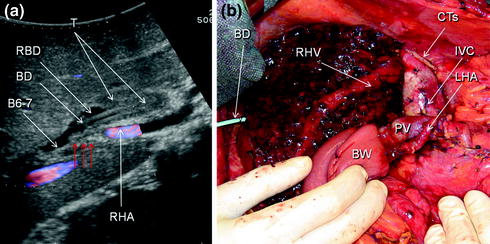
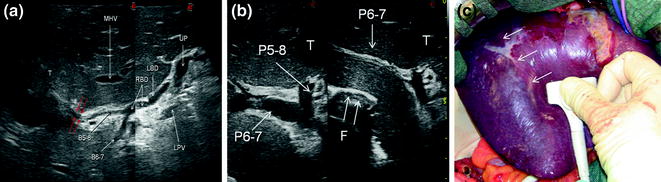
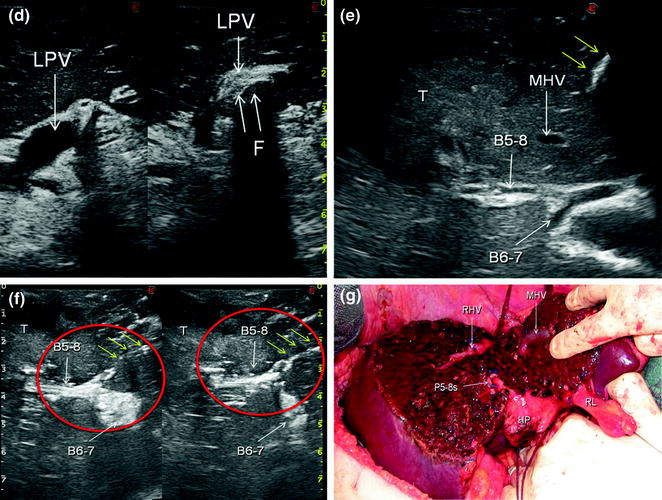
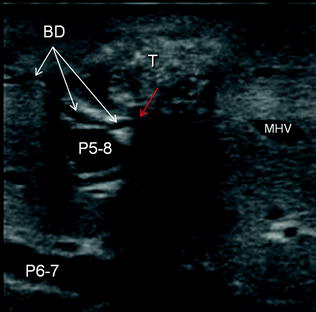
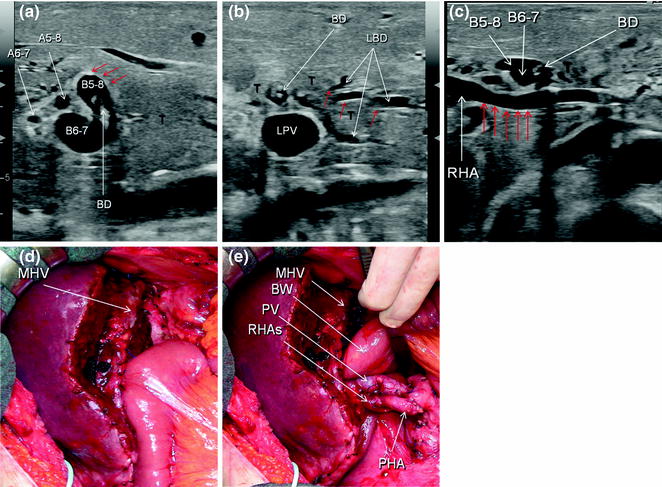
Fig. 9.4
a IOUS image of the main lesion (T) which is slightly hypoechoic compared to the surrounding liver, with undefined margins especially with regard to their intramural extension (red arrows) at the level of the right anterior (B5-8) and right posterior (B6-7) bile ducts, in which the biliary drainage is visible (BD); b the tumor extends to the left bile duct (LBD), but there are no reliable criteria to establish precisely the extent of the intramural extension (red arrows); c the right hepatic artery, passing in contact with the tumor except a slightly reduced caliper and an unusual straightness (red arrows), does not show in IOUS other aspects which could help to define whether it is invaded by the tumor or not; d with the bile duct stump frozen section free of tumor, a right hepatectomy together with segment 1 was carried out; e the right hepatic artery was resected, and, in absence of a left hepatic artery suitable for being tilted and anastomosed with its stump (RHAs), the latter was anastomosed to the proper hepatic artery (PHA), which remained long; hepatic artery to the right anterior section (A5-8); hepatic artery to the right posterior section (A6-7); bowel (BW); left portal vein (LPV); middle hepatic vein (MHV); portal vein (PV)
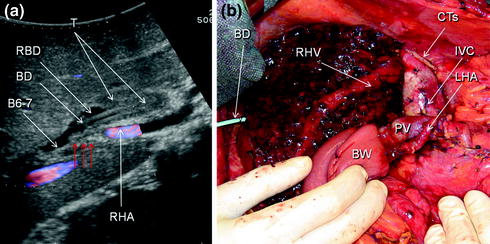
Fig. 9.5
a IOUS image showing the main lesion (T) which is isoechoic in relation to the surrounding liver, with undefined margins especially with regard to its intramural extension at the level of the right bile duct (RBD) just at the level of the confluence of the right posterior bile duct (B6-7); furthermore, the right hepatic artery (RHA) has stopped (red arrows); b a left trisectionectomy together with the left hepatic artery (LHA) tilting to revascularize the stump of the right posterior hepatic artery was carried out; biliary drainage (BD); bowel (BW); stump of the common trunk of the middle and left hepatic veins (CTs); inferior vena cava (IVC); portal vein (PV)
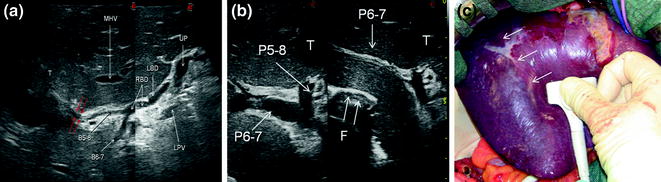
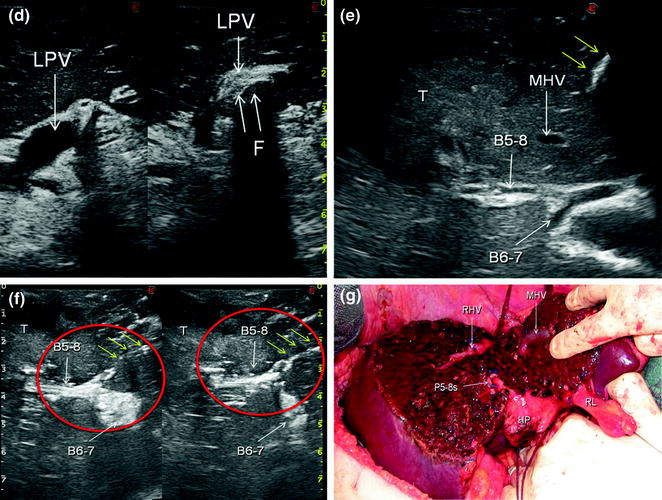
Fig. 9.6
a IOUS image showing the main lesion (T) infiltrating the right anterior pedicle including its bile duct (B5-8) (red arrows); despite this, IOUS was able to also perfectly disclose the anatomy of the biliary tree showing the right-sided confluence of B5-8 and the bile duct from the right posterior section (B6-7) into the right bile duct (RBD), and the confluence of the latter with the left bile duct (LBD) into the common bile duct; b–d then, a right anterior compression sectionectomy was planned as described in Chap. 8, by compressing the right posterior portal branch (P6-7) (b), which made evident the right-sided demarcation line on the liver surface (arrows) (c), compressing the left portal vein (LPV) (d), and marking also the related demarcation line; e dissection was carried out (yellow arrows) approaching the middle hepatic vein (MHV) first, and then the B5-8 distant from its confluence with B6-7; f once the right anterior pedicle was reached and encircled, before its division, the hooking technique was performed as previously described (see Chap. 8), to confirm the preservation of B6-7 (red circles focus the point of encirclement and traction, yellow arrows the dissection line); g then a right anterior sectionectomy was carried out; finger (F); hepatic pedicle (HP); portal branch to the right anterior section (P5-8); stump of the portal branch to the right anterior section (P5-8 s); right hepatic vein (RHV); round ligament (RL); umbilical portion (UP)
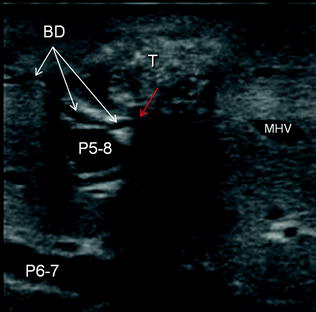
Fig. 9.7
A bile duct (BD) infiltrated (red arrow) by a tumor (T) and thus visible with its peculiar serpiginous path; middle hepatic vein (MHV); portal branch to the right anterior section (P5-8); portal branch to the right posterior section (P6-7)