Fig. 14.1
Visualisation of the surgical bed. The surgeon checks the fit of the applicator to the dimensions of the tumour cavity

Fig. 14.2
The applicator on an arm of the INTRABEAM PRS 500 is placed in the tumour cavity: (a) via laparotomy; (b, c) via a sacro-perineal approach

Fig. 14.3
Ongoing intraoperative radiation. The operating field is secured with sterile surgical sheets
14.3 Results
IORT is thought to supplement surgery, resulting in improved local control of disease. To date very few studies have been conducted using orthovoltage IOXRT. Instead, most trials have been based on IOERT. Assimilation of the necessary equipment in non-modified operating theatres is, however, not possible. IOERT requires stringent radiation protection measures and the operating theatre needs to comply with the conditions of a radiotherapy bunker because the radiation energy is much higher and the penetration of radiation, greater. Radiotherapy using the INTRABEAM PRS based on kilovoltage photons allows the use of IOXRT within the existing premises of the operating theatre due to the low penetration of radiation. Since the radiation dose is frequently limited by the tolerance of surrounding tissues, INTRABEAM enables escalation of the dosage without affecting adjacent organs (Treiber et al. 2004; Dresen et al. 2008).
While there are few publications on the use of the INTRABEAM system in CRC, the Cleveland radiotherapy group has longstanding experience (Guo et al. 2012). At the European Society of Surgical Oncology congress in 2010, S. Guo presented the preliminary results of 10 years’ experience with the use of orthovoltage IORT in highly selected patients with primary advanced and recurrent CRC. These results have been published recently (Guo et al. 2012). In the recurrence study group, median survival was 32 months with a median follow-up of 22 months. Addition of orthovoltage IORT to surgery in patients with locally recurrent rectal cancer resulted in an overall 3-year survival of 43 %. Median hospitalisation time after surgery was 7 days (range 2–59 days). These results were similar to those obtained in other U.S. centres where IOERT equipment is used. Studies from the Mayo Clinic demonstrated a median survival of 36 months and a 3-year overall survival of 43 % (Guo et al. 2012) (Fig. 14.4). This contrasts with a median survival of 19 months with palliative surgery alone (Garcia-Aguilar et al. 2001).
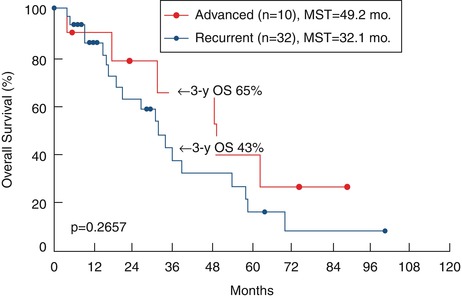
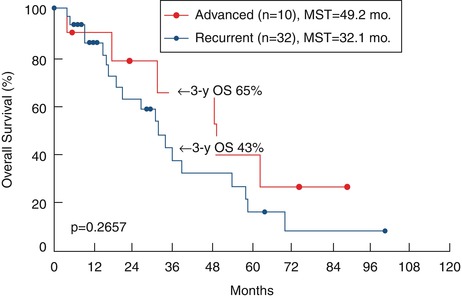
Fig. 14.4
Results of a retrospective phase I/II study on CRC at the Cleveland Clinic, Ohio (Guo et al. 2012)
In the Department of Surgical Oncology of the Medical University of Lublin, between 2006 and 2011, 79 patients with recurrent CRC underwent surgical treatment. Surgery supplemented with IORT using the PRS system was performed in 22 cases of locally recurrent rectal cancer. Twelve women and ten men were treated; the median age of the entire group was 66 years (range 26–77 years). The median duration of IORT was 17 min (range 6–47 min). The types of surgical procedure performed were as follows: 13 transabdominal resections of the tumour, six transanal resections (transanal microsurgical tumour excision), two abdominosacral amputations of the rectum and one sacrectomy. In 13 cases (59 %), extended multivisceral resections had to be done due to extensive spread of the tumour and involvement of other organs. There were no postoperative complications that might be purely attributable to the use of IORT. In particular, no cases of ureteric stenosis were detected during the postoperative course. None of the patients died during postoperative hospitalisation. In four (18 %) patients, re-operations were necessary, in two cases because of the intestinal obstruction, in one because of the presence of a fistula (anastomotic dehiscence) and in one due to intraperitoneal bleeding. The median postoperative hospital stay was 7 days (range 2–23 days). One patient who received IORT died early after surgery (90-day mortality, 4.5 %) owing to exacerbation of chronic renal failure during the postoperative period. The median follow-up time is 11 months (range 1–53 months), which is too short for late outcome evaluation.
14.4 Conclusions
Since there are only scattered data on the use of IORT in recurrent CRC patients, IORT cannot be considered standard treatment and should still be regarded as an experimental treatment option (Wydmanski et al. 2005). It seems that IORT performed after surgical resection is a safe and feasible procedure with a good therapeutic index that can improve treatment results and significantly increase local tumour control. The use of IORT as an adjunct to surgical resection does not prolong hospitalisation. Thorough follow-up should be conducted (with the use of tumour markers, endoscopy and modern metabolic imaging) to identify LR in the earliest stage, and R0 resection remains the baseline in accomplishing satisfying long-term survival rates.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree