Fig. 4.1
Keer-Muller maneuver performed with the patient on the delivery table; the top operator in the left hand placed on the abdomen pushes the fetal head down and evaluates the fetal–pelvic proportion while with his right hand placed in the vagina currency progression. The large arrow at the top indicates the possible thrust of aid, practiced on the uterine fundus (upper picture). Below maneuver palpation to highlight the sign of the step, in fetal–pelvic disproportion (lower picture)
Labor dystocia is one of the most common indications for cesarean section [5].
The fetal lie can be longitudinal or transverse, presentation describes the lowest fetal part in the birth canal, position means how the fetus is rotated, and station refers to the level of the presenting part in the birth canal. Müller first described the concept of station in 1868. The fetal descent in the birth canal is assessed by vaginal digital examinations and related to the ischial spine (Fig. 4.2a, b). Minus five corresponds to the pelvic inlet, zero to the level of the ischial spine, and plus four corresponds to the pelvic floor (Fig. 4.3a, b) [3]. In 1954, Friedman introduced the partograph [1]. He has documented a strong correlation between cervical dilatation and station [6] and an association between high station at arrest of labor and adverse outcome [7]. Philpott suggested in 1972 to use “alert lines” and “action lines” (4 h from the “alert line”) in partographs to evaluate labor progress [8], and WHO has adopted this method [3]. Prolonged labor is defined when cervical dilatation crosses the “action line.” Some hospitals use partographs from the Dublin school of “active management of labor” [9] and expect one-cm dilatation/hour (the slope of the alert line), whereas other hospitals define prolonged labor when cervical dilatation is <1.2 cm/h in nulliparous women and <1.5 cm/h in parous women [2].
Fig. 4.2
Palpation of the ischial spines. (a) The ischial spines can be felt before the commitment of the presenting part. (b) Maneuver to assess the midpelvis
Fig. 4.3
(a) Levels of obstetric pelvis level 0 passes through the ischial spines. (expressed in cm) (b) Palpation of the fetal head placed at −3, at the narrow top (the other two hands indicate palpation at level 0 that is the narrow, medium, and at +3, i.e., close to the bottom) (expressed in inches)
Traditionally, labor progression has been assessed by digital examination of cervical dilatation and fetal descent. In one study from the 1980s, repeatability of digital examinations was found to be acceptable [10]. Recent studies, however, dispute these findings and found clinical examination of fetal descent and position to be subjective with high interobserver variation [11, 12]. Dupuis et al. made an important contribution to this debate when he rigorously assessed the accuracy of station diagnosis with digital examinations [13]. He used a birth simulator with objectively defined stations and studied the reliability of clinical assessment of engagement and fetal station in 57 physicians (32 residents and 25 attending physicians). A fetal head mannequin was placed in 11 different stations in a random order. The error in the diagnosis of station was assessed by calculating the difference between the true station (established by sensors in the birth simulator) and that determined by the clinician’s fingers. Numerical errors occurred in 50–88% of cases for residents (average experience 2 years) and in 36–80% of cases for attending physicians (average experience 9 years). The mean error rate in the diagnosis of engagement was 12%, and this misdiagnosis was distributed equally between false-positives and false-negatives. Undiagnosed “high” stations accounted for 22% of the errors made by residents, and 16% of those made by attending physicians [13]. This study provides evidence that digital assessment of fetal head station is unreliable.
Consequently, an objective method for assessing labor progression is highly desirable. Sherer has compared the search for new methods to assess descent of the fetal head with the search for “the holy grail” and called it the ultimate challenge of clinical applicability of intrapartum ultrasound imaging [14].
4.4 Cardinal Movements
The birth canal is curved, and the fetal head at term is quite large compared to the pelvis (Fig. 4.4). Therefore, the fetal head has to rotate in order to pass through the birth canal. For a fetus in occiput anterior position, the four cardinal movements of labor are flexion, internal rotation, extension, and external rotation. The fetal head usually enters the birth canal transversely and engages in the pelvic inlet. Descent will occur due to pressure from uterine contractions. As soon as the descending head meets resistance, the fetal head flexes and rotates. During the active first stage of labor, the fetal head descent first depends on internal rotation and later on deflexion of the neck (extension) (Fig. 4.5a–f).
Fig. 4.4
Sagittal section of midwives’ pelvis: on the left, it shows the curvature of the birth canal, while on the right, it shows the pelvic floor Hodge (P = cylinder of descent of Pigeaud, F = triangle the disengagement of Fochier). (1) Inlet pelvis, (2) midpelvis, (3) outlet pelvis, (4) pelvic floor
Fig. 4.5
(a) Illustration of a transabdominal ultrasound showing the mechanism of commitment, the bending of the head down the narrow upper left oblique diameter according to the transverse (right). (b) Transabdominal ultrasound image showing the progression of the head toward the close medium and rotation (right). (c) An ultrasound image of translabial that displays the rotation of the head that has reached the ischial spines, and the diameter of the occipito-front is aligned with the anteroposterior diameter of the pelvis. (d) Translabial ultrasound image showing the complete rotation (internal rotation) and the full extent of the fetal head. (e) Movement of return (or external rotation of the fetal head) in which the frontal–occipital diameter is oriented along the oblique diameter left (right), as similar to the one position that the head assumes the entrance pelvic. (f) Fetal head expression from birth canal. (g) Birth of the anterior shoulder (arrow). (h) Birth of the posterior shoulder (arrow)
Figure 4.5a–f show the movements of the cardinal delivery in both the first in the second stage, for didactic.
For a fetus in an occiput posterior position, the cardinal movements are slightly different. The first, second, and fourth movements are the same (flexion, internal and external rotation), but the third is maximal flexion followed by extension. Not surprisingly these complex movements are difficult to assess objectively using digital examinations. Ultrasound might add important information when trying to assess the cardinal movements.
4.5 Ultrasound Methods Assessing Fetal Station
The bony maternal pelvis limits the quality of ultrasound acquisitions. The traditional clinical examination relates the presenting part of the fetus to the ischial spine. Unfortunately, the ischial spine is difficult to define using ultrasound. Consequently, other landmarks are necessary, and several different ultrasound methods for assessing fetal descent have been proposed.
Already in 1977 Lewin et al. suggested using ultrasound to evaluate station. They measured the distance from the fetal head to the sacral tip of the mother [15]. The transducer was placed over the sacral tip, and A-mode ultrasound was used. The first echo was from the sacral tip; the second from the fetal scull and the distance could be measured. This method was never implemented in clinical practice.
In 2003, Sherer and Abulafia suggested a transabdominal approach. The fetal head was considered engaged on transverse suprapubic ultrasound if the fetal biparietal diameter was below the maternal pelvic inlet [16].
However, due to shadowing from the bony structures of the maternal pelvis, transabdominal ultrasound is not reliable when the presenting part has descended to low levels in the birth canal. Therefore, transperineal or translabial approaches have been suggested, and a number of different methods have emerged.
At present, the best landmark is the symphysis pubis which is better viewed with ultrasound than digital examination, as ultrasound immediately meets the symphysis (Fig. 4.6a, b).
Fig. 4.6
The figures illustrate the ways to palpate the symphysis pubis during the digital obstetric examination (a) and to show symphysis by translabial ultrasounds (b)
4.5.1 Progression Distance
A sagittal transperineal ultrasound method for assessing fetal head descent was published by Dietz and Lanzarone in 2005. They used a line vertical to the central axis of the symphysis pubis as reference (the “infrapubic line”) and measured the distance between this line and the presenting part [17]. This method is called the progression distance (Fig. 4.7). Although this method was originally suggested evaluating head engagement, the method can also be used to evaluate labor progression.
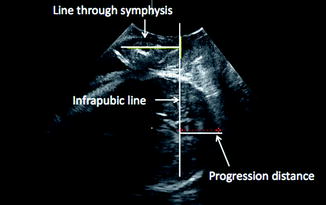
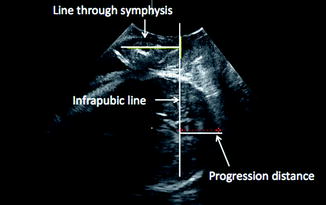
Fig. 4.7
The progression distance is related to the “infrapubic line”
4.5.2 Angle of Progression
A similar but more convenient method is suggested by Barbera et al. They also refer to a line through the symphysis pubis and draw a line tangentially to the fetal head to measure the angle between the lines (Fig. 4.8) [18]. The angle increases with fetal head descent. The two methods (progression distance and angle of progression) are correlated, but not mathematically identical because the fetal head has an oval shape and the lowest part of the presenting part is not necessarily identical with the point where the tangent touches the fetal head. The angle of progression method was designed for use during the second stage of labor, and the method has been found to predict the probability of an easy operative vaginal delivery [19]. The repeatability of this method is very good [20]; however, the scientific documentation is restricted to fetuses in occiput anterior position only.
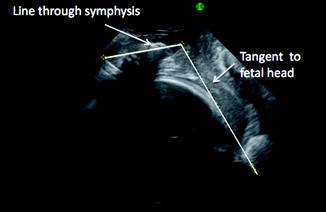
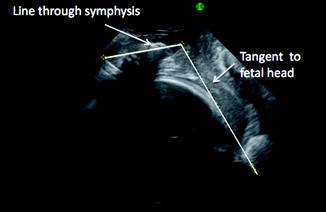
Fig. 4.8
The angle of progression is measured as the angle between a line through the pubic symphysis and a line tangentially to the fetal head
4.5.3 Head Direction
Henrich et al. focused on the fetal head deflection and assessed the direction of the fetal head. They also used the “infrapubic line” perpendicular to the long axis of the symphysis as a reference and assessed the widest fetal head diameter and its movement with regard to the infrapubic line. At high stations, the fetal head points downward, and at low stations, the head points upward [21]. This method has also been used in assessment of station. The parallel plane through the ischial spines is defined 3 cm below the infrapubic line. Ultrasound-assessed head station can be measured along the longest visible axis of the fetal head, between the intersections with the infrapubic line and the deepest bony part of the fetal head, subtracting 3 cm for the level of the ischial spines (Fig. 4.9) [22]. The clinical value of the method is probably best in the active phase of the second stage, and a change in fetal head direction during pushing can easily be observed.
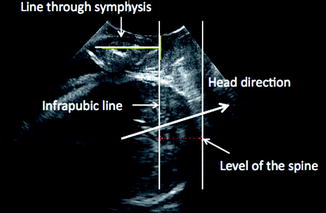
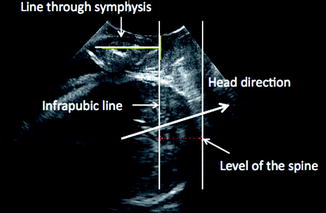
Fig. 4.9
The head direction is related to the “infrapubic line.” In this figure, the fetal head is directed upward and at the level of the spine (3 cm below the “infrapubic line”)
4.5.4 Midline
The rotation (position) of the fetal head can be defined in a transverse perineal scan as published by Ghi et al. and illustrated in Fig. 4.10. This result can be combined with fetal head direction [23]. However, the midline echo of the fetal head is difficult to obtain in fetuses at high stations, and a high degree of interobserver variation has been documented [20]. The midline is easier to observe directly in a transverse 2-D acquisition than obtaining the B-plane from a 3-D acquisition.
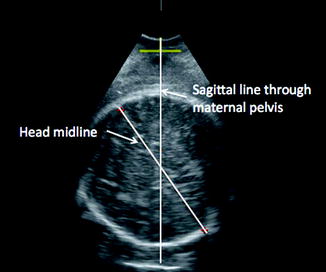
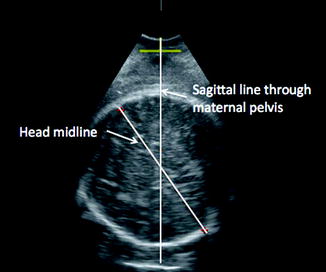
Fig. 4.10
The midline of the fetal head is related to a sagittal plane through the maternal pelvis
4.5.5 Head–Perineum Distance
Fetal head descent can be measured as the shortest distance between the outer bony limit of the fetal skull and the perineum (head–perineum distance) as suggested by Eggebø et al. (Fig. 4.11) [24, 25]. The transducer is placed between the labia majora obtaining a transverse view. The soft tissue is easy to compress, and the transducer meets resistance against the pubic arch. The transducer should be wide enough not to enter the vagina, and the “goal line” of the labor will be the reference line. To obtain the shortest distance, the transducer should be moved and angled before the distance is defined. This method can be used at all stations and for fetuses in all positions. The distance will be shorter with fetal descent even though the fetus passes through a curved birth canal (Fig. 4.12a, b). The soft tissue between the labia majora is easy to compress even in obese women, and it is not painful for the women [25].
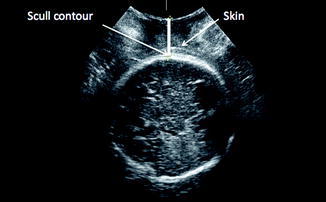
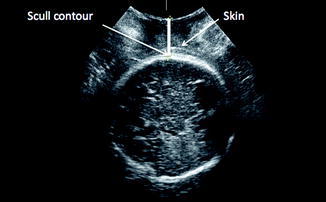
Fig. 4.11
Head–perineum distance
Fig. 4.12
(a) Schematic drawing of fetal head descent in a curved birth. (b) Sagittal section of pelvis and obstetrical birth canal shows that the mechanism of engagement, descent, and rotation of the fetal head in vertex presentation of left occiput anterior (LOA). The three arrows indicate the position of the head close to the upper, middle, and bottom and the direction of the summit (as described by Cadwell, Moloy, and D’Esopo)
4.5.6 Continuous Ultrasound Monitoring
Computerized continuous labor-monitor systems have been developed [26, 27]. These systems allow a continuous registration of the labor progress. Sensors are attached to the maternal pelvis, and with an additional sensor attached to the physician’s finger, the position of the ischial spines can be defined. Using this information in combination with a sensor attached to the fetal head and on to a transperineal ultrasound transducer, the fetal head descent can be continuously monitored.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree