Massimo Tonolini (ed.)Imaging of Ulcerative Colitis201410.1007/978-88-470-5409-7_1
© Springer-Verlag Italia 2014
1. Introduction
(1)
Radiology Department, “Luigi Sacco” University Hospital, Via G.B. Grassi 74, 20157 Milan, Italy
Abstract
As defined in the European Crohn’s and Colitis Organization (ECCO) guidelines, Ulcerative Colitis (UC) is a chronic inflammatory condition involving a non-granulomatous mucosal inflammation that probably arises from an interaction between genetic and environmental factors. UC commences in the rectum and extends proximally in a confluent manner to affect a variable extent of the large bowel. Traditionally, diagnostic imaging of UC relied on double-contrast barium enema, which in experienced hands could provide useful information concerning the extent of colonic disease, although limited to the mucosal surface. Currently, thanks to dramatic technical improvements, imaging modalities such as multidetector computed tomography (MDCT), magnetic resonance imaging (MRI) and ultrasound are increasingly employed at referral Centres to investigate UC patients in both urgent and elective settings. Complementary to endoscopy, cross-sectional imaging comprehensively investigates the intestinal disease, associated perivisceral changes and extraintestinal manifestations. Furthermore, diagnostic imaging is needed to stage neoplasms and perianal inflammatory diseases in UC patients. Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is currently the gold standard procedure for surgical treatment of UC. Knowledge of the surgical technique and of normal imaging appearances of the “pouch” reservoir are needed to interpret early postoperative studies and to assess chronic pouch-related disorders.
Keywords:
Ulcerative colitisDouble contrast barium enema CTMRIUltrasoundPlain radiographsPrognosisAcute colitisComplicationsColorectal neoplasmsPerianal inflammatory diseaseIleal pouch anastomosis surgerySurgical techniquePelvic sepsisPouchitisAs defined by the current guidelines of the European Crohn’s and Colitis Organization (ECCO), which have been recently revised in 2012, Ulcerative Colitis (UC) is a life-long disease whose precise aetiology is unknown, that probably arises from an interaction between genetic and environmental factors. Pathologically, UC is a chronic inflammatory condition involving a non-granulomatous mucosal inflammation that starts from the rectum and extends proximally in a continuous, confluent manner to affect a variable extent of the colon or its entire mucosal surface [1, 2].
Nowadays, UC is observed predominantly in the developed world, and its incidence is reportedly increasing in Southern and developing countries. Characterized by a relapsing and remitting course, UC affects both sexes equally and usually presents in late adolescence and early adulthood. A second, smaller peak of incidence is observed after the fifth decade of life. The onset of UC is often insidious. Symptoms generally reflect the severity and extent of the disease, and most commonly include bloody diarrhoea, rectal bleeding and/or urgency [1, 2].
The diagnosis of UC is established upon a combination of medical history, clinical evaluation, and consistent endoscopic and histological findings. Traditionally, diagnostic imaging of UC relied on double-contrast barium enema, a modality which in experienced hands could provide useful information concerning the extent of colonic disease, although limited to the mucosal surface. The characteristic radiographic appearances include a continuous disease with invariable rectal involvement, a diffuse granularity or stippled pattern of the mucosa, pseudopolyps in a denuded flat mucosal surface, and a shortened, rigid and narrow colon with loss of normal haustral folds in advanced stages [1, 3, 4].
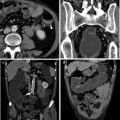
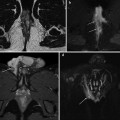
In recent years, diagnostic imaging modalities such as multidetector computed tomography (MDCT), magnetic resonance imaging (MRI) and ultrasound have undergone dramatic technical improvements, and are increasingly employed at referral centres to investigate UC patients in both urgent and elective settings. Complementary to endoscopy, cross-sectional imaging can assess the thickness and structure of the intestinal wall, as well as associated abnormalities of the perivisceral fat planes and surrounding organs. Therefore, imaging studies are optimally suited to comprehensively investigate the intestinal disease, associated perivisceral changes and extraintestinal manifestations [5–7].
For instance, since the intestinal extent of UC influences prognosis and dictates patient management and surveillance, the disease distribution classified according to the Montreal criteria may be investigated by means of water enema MDCT colonography or MRI in selected cases, such as proximally to an impassable stricture [1, 2].
A potentially life-threatening condition, acute severe UC occurs in 15 % of patients, includes systemic symptoms such as malaise, vomiting, abdominal pain and fever, and represents an indication for in-hospital treatment. Although plain radiographs retain their traditional value in the initial assessment of patients with suspected severe UC, MDCT and MRI are increasingly employed to provide an earlier diagnosis, differentiate from other causes of acute abdomen, identify possible complications such as perforation or abscess collections, obviate the risk for endoscopy in a critical situation, allow intensive medical treatment and provide support for timely surgery [8, 9].
Furthermore, cross-sectional imaging is necessary to assess associated extraintestinal manifestations of UC that require a specific treatment approach, such as primary sclerosing cholangitis, portal venous system thrombosis and arthritis [10–16].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree