and Alfredo Blandino1
(1)
Department of Radiological Sciences, University of Messina, Messina, Italy
The prevalence of small bowel diseases is low, and their clinical diagnosis is often complicated by the presence of aspecific symptoms. Moreover, the small intestine has always been a challenging area to investigate by clinical or radiographic means due to its anatomy, location, and relatively tortuosity. The upper gastrointestinal tract, comprising the esophagus, stomach, and duodenum, is accessible by direct endoscopy, as the colon is. The small bowel, however, is beyond the reach of the most flexible endoscopes.
In the past years, barium small bowel follow-through (SBFT) studies and enteroclysis were the standard radiological approaches for diagnosing gut diseases. In particular, SBFT provides information about intraluminal extension of disease and small bowel motility disorders. On the other side, small bowel enteroclysis is more accurate than SBFT at detecting early mucosal changes, but both methods provide only limited, indirect information on the state of bowel wall and of surrounding structures. Moreover, these techniques suffer from problems with overlapping bowel loops.
Nowadays, the diagnosis of Crohn’s disease (CD) and the detection of disease activity are the major indications for small bowel imaging in most centers. However, there are many other conditions that may cause similar clinical symptoms or radiological signs to those of CD.
Cross-sectional imaging has a clear advantage in this aspect, and it can also depict clinically unsuspected abdominal diseases that may mimic a flare of inflammatory bowel disease (IBD), such as acute appendicitis or diverticulitis [1, 2].
In the last decade, there has been a renewed interest for small bowel imaging, using a variety of techniques such as ultrasound (US), computed tomography (CT), and magnetic resonance imaging (MRI).
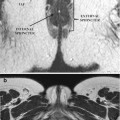
US is a useful radiation-free alternative for evaluating IBD; it is widely available and is not affected by patient motion, making it particularly attractive for children examination [3–7]. In patients with CD, the most widely used criterion for the diagnosis of IBD is bowel wall thickening with increased vascularization at color or power Doppler [3–7].
Although these US findings are rather nonspecific, they can be used to guide further studies, to evaluate the response of inflamed bowel segments to therapy, and to detect postsurgical recurrence of inflammation.
Contrast-enhanced ultrasound (CEUS) of the intestinal tract is a relatively new technique that involves i.v. administration of an ultrasound contrast agent with real-time examination, providing an accurate depiction of the bowel wall microvascularization and the perienteric tissues, thus further improving the therapy planning and the monitoring of the treatment efficacy [8–10].
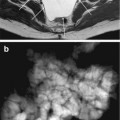
In small intestine contrast-enhanced ultrasonography (SICUS), performed using an oral contrast agent to distend the bowel (i.e., iso-osmolar polyethylene glycol solution), the sensitivity and specificity of US in detecting IBDs range from 78 to 90 % and 83 to 95 %, respectively [5, 11–13].
US is most effective at detecting IBD in the terminal ileum but may fail to fully delineate complications and to exclude disease elsewhere in the small and large bowel [14].
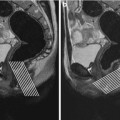
CT has become a routine examination in the evaluation of gastrointestinal disorders because of its accuracy with axial images and multiplanar reconstruction and rapid execution time. The primary role of conventional CT in patients affected by IBD was to evaluate extraenteric manifestations and complications, such as fistulas, abscess, and bowel obstruction. Multidetector technology, enabling faster imaging and higher spatial resolution, has increased the role of CT in intestinal diagnostic. In addition to allowing direct visualization of extraenteric structures, CT enterography (CTE), performed using oral neutral contrast agents and rapid intravenous contrast infusion, can be also used to reliably identify findings of active inflammation in the small bowel: wall thickening (thickness >3 mm), mural stratification, mural hyperenhancement, increased attenuation of perienteric fat, and engorged vasa recta [15–17].
Many researchers have mentioned positive correlation between CTE findings and clinical/biochemical markers of disease activity, such as CD activity index (CDAI), C-reactive protein, and erythrocyte sedimentation rate. However, because patients with CD are often young and CD is a chronic and relapsing disease, they may have to undergo lifetime repeated imaging examinations to assess the status of their disease. Although CT is widely used in CD, one significant limitation is represented by patient exposure to ionizing radiation. Recent studies highlighted the high cumulative radiation dosages delivered to patients with CD, mainly due to an increased use of CT [18–20]. The carcinogenic effect of radiation can be particularly significant in patients with CD, who already have an increased risk of developing gastrointestinal or hepatobiliary cancer and small bowel lymphoma.
For the above mentioned reasons, it is neither recommendable to perform serial CT scans, to differentiate a stricture from a badly distended tract (this latter case could be due to slow transit of luminal contrast material or to peristalsis).
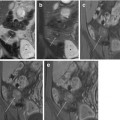
With the increasing awareness on the risk of radiation exposure, global interest in abdominal magnetic resonance (MR) imaging has generally improved. Over the last decade, the increased temporal and spatial resolution of MR images, combined with the use of large volumes of oral contrast agents to provide bowel distention, has allowed the evaluation of bowel wall thickening, wall edema, and contrast enhancement, which are useful findings for the assessment of active ileitis, as well as extraenteric complications [21]. In addition, MRI has the potential advantage of providing functional and quantitative information about bowel wall (e.g., perfusion, diffusion, and motility) that cannot be obtained by CT [22–27]. For these reasons, a new MR technique targeted for the study of small bowel and called MR enterography (MREg) has been introduced as a radiation-free alternative method to evaluate patients with CD, and it is increasingly becoming the first line of investigation for such patients. It can be useful at both initial diagnosis and follow-up [21]; the most important issue is that MRI provides multiplanar images with high contrast resolution for soft tissue, thus enabling differential diagnosis between edema and fibrosis that represents a key issue in patients who suffer from CD.
However, MRI also has some limitations. First of all, MRI of the small bowel requires optimal MR scanner with fast imaging capabilities and a certain degree of operator’s experience [21]. Secondly, a rigorous technical approach should be used to obtain satisfactory results.
Although diagnosis of CD and evaluation of disease activity are the major indications for small bowel MRI in most of centers, MREg is recently playing an evolving role in the detection of other enteric diseases, such as postoperative adhesion, celiac disease, radiation enteritis, scleroderma, and small bowel malignancy [28].