Introduction to Brain Imaging
David J. Seidenwurm
Govind Mukundan
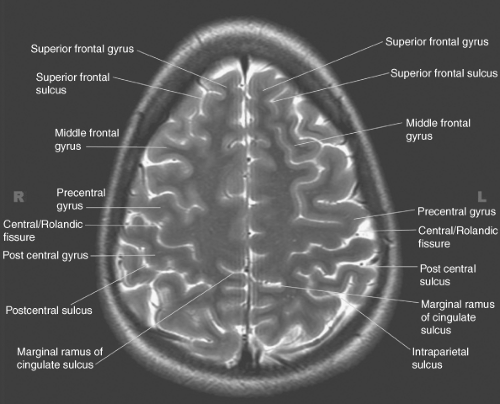
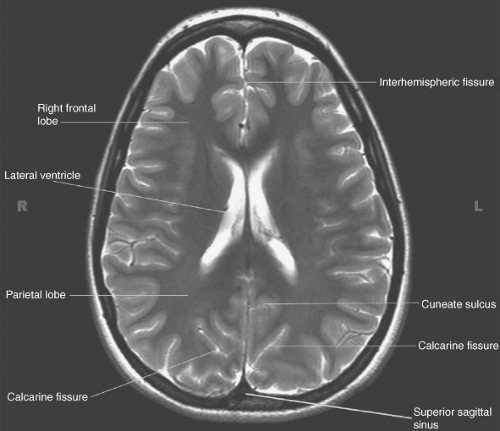
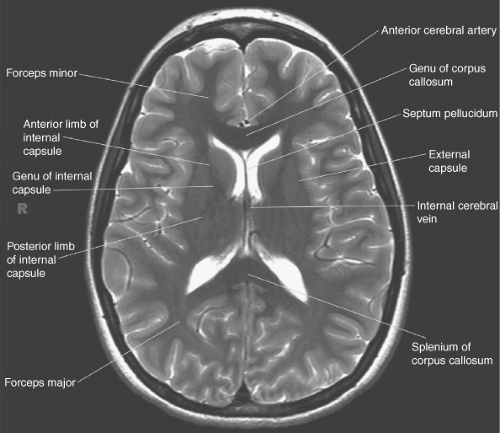
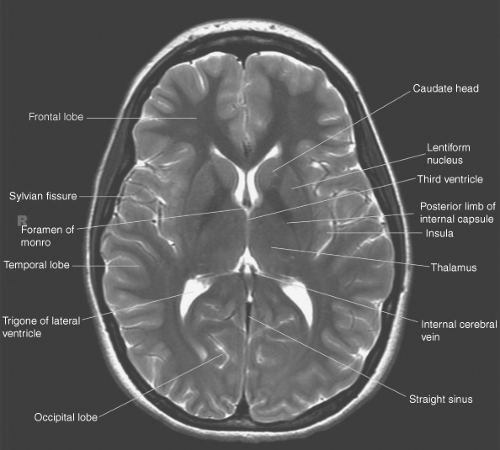
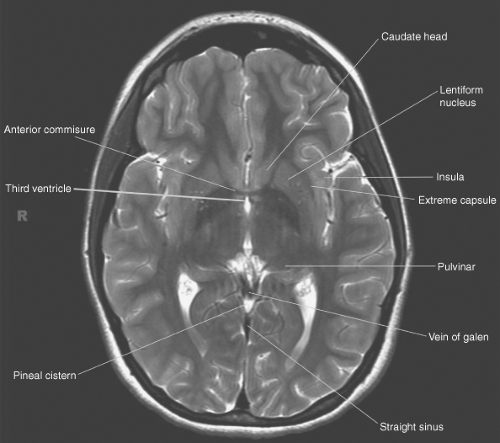
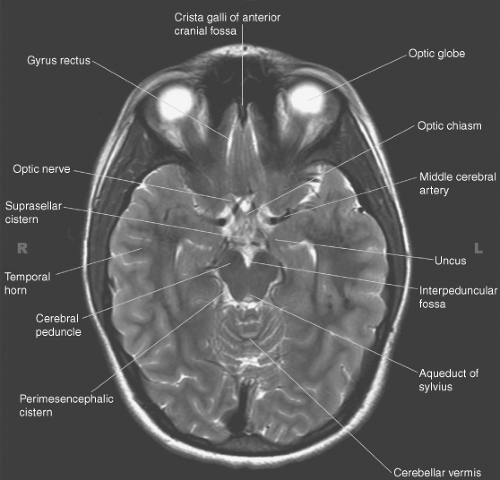
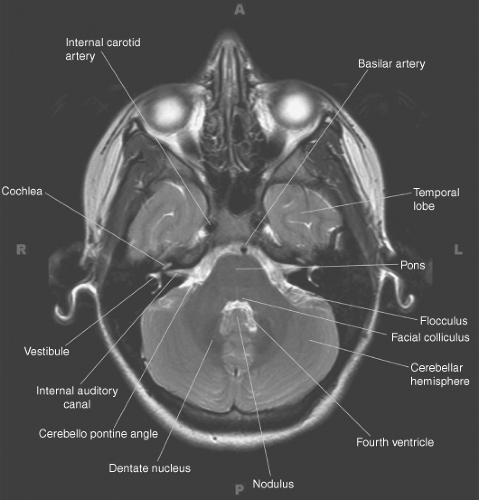
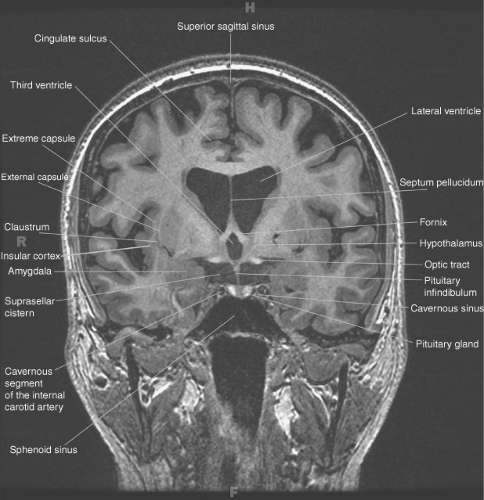
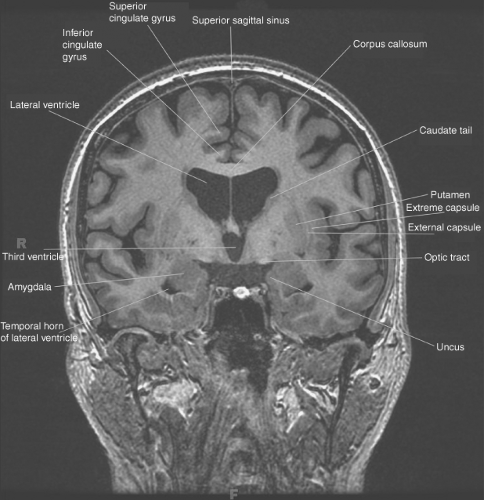
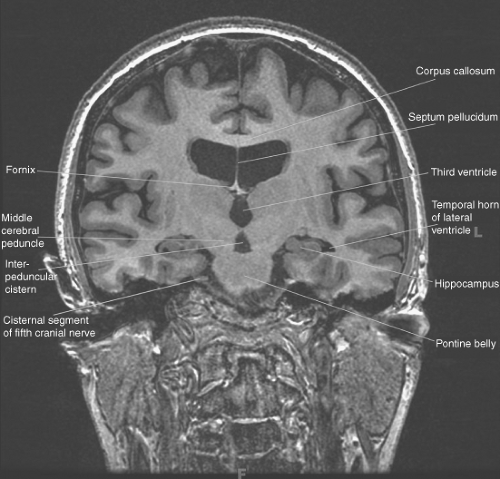
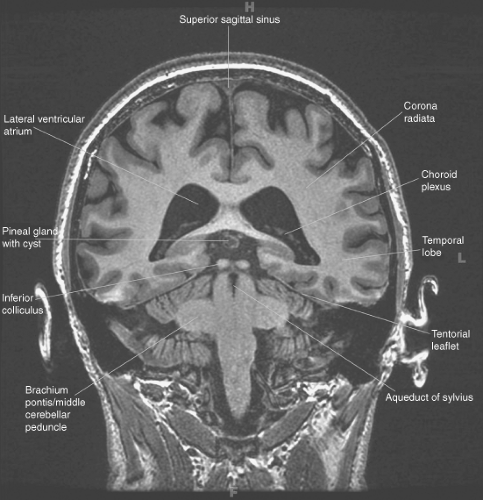
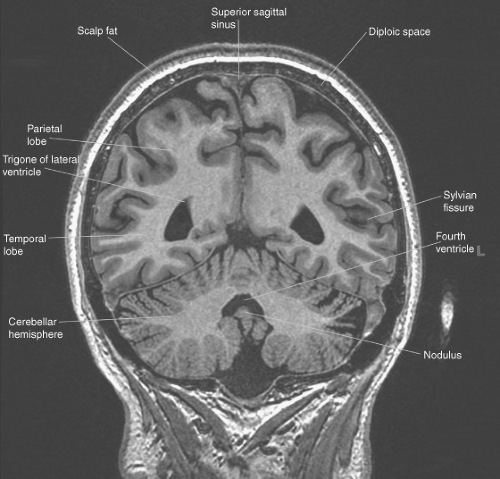
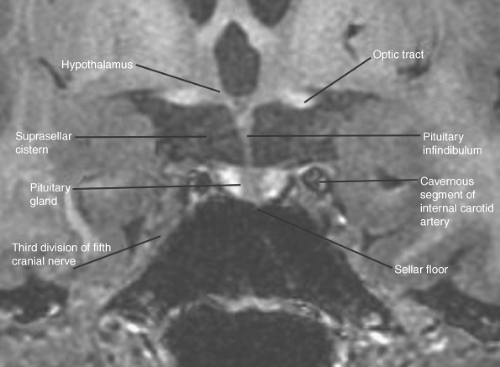
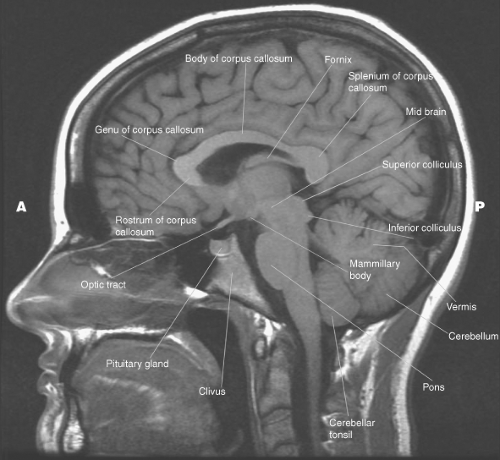
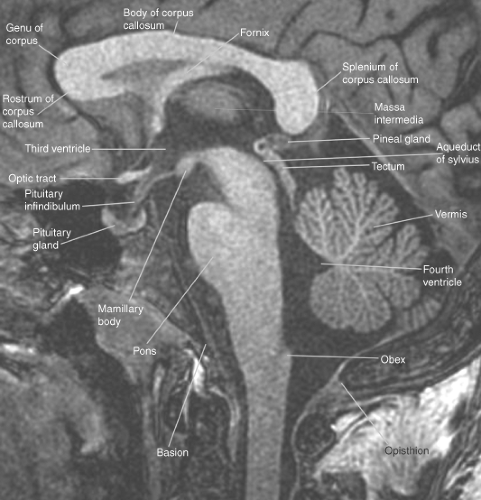
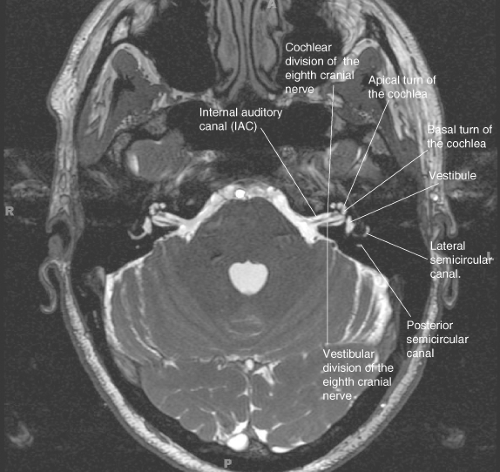
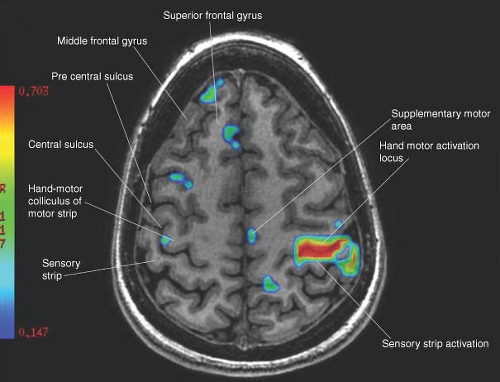
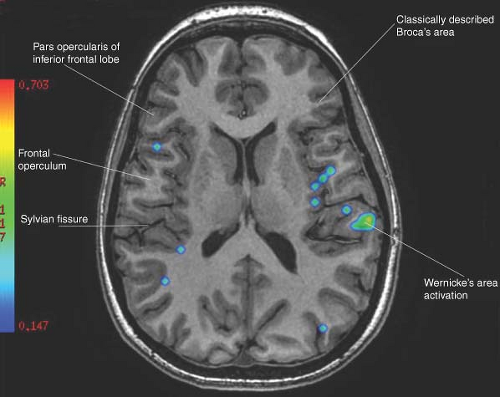
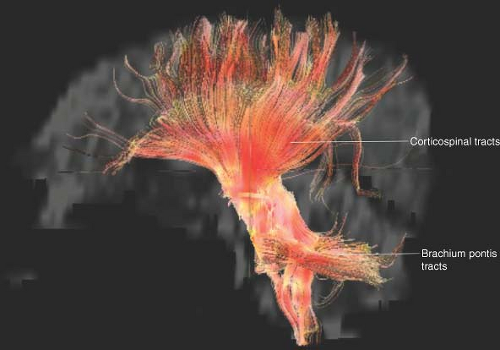
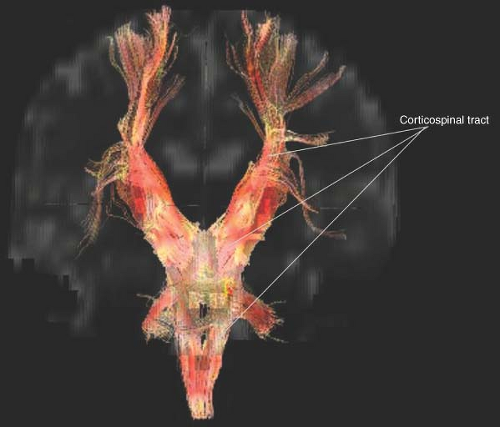
This chapter provides an atlas of neuroanatomy and a discussion of the principles of brain imaging and interpretation. Brain anatomy is shown on 3-T MR T2-weighted images in axial plane (Figs. 2.1 to 2.8), on 3-T MR T1-weighted images in coronal plane (Figs. 2.9 to 2.16), and on 3-T MR T1-weighted images in sagittal plane (Figs. 2.17 and 2.18). Examples of ultrafast MR FIESTA (fast imaging employing steady-state acquisition) images are shown in Figures 2.19 and 2.20. Examples of MR functional brain imaging are shown in Figures 2.21 and 2.22. Examples of MR 3 T diffusion tensor imaging are shown in Figures 2.23 and 2.24. MR white matter tractography is shown in Figures 2.25 and 2.26.
Looking At the Brain
A few simple principles can be followed to ensure that no neurosurgical emergency is missed, even on a first cursory look at an emergency CT scan at midnight.
Midline. The middle of the patient’s brain should be in the middle of the patient’s head and the two sides of the brain should look alike (Figs. 2.1 to 2.5). While there are important functional asymmetries between the right and left hemispheres, the anatomic differences are subtle and play no role in clinical neuroradiology. Any shift of midline structures is presumed to represent a mass lesion on the side from which the midline is displaced. For practical purposes, there are no acute “sucking” brain wounds that draw the midline toward themselves. If the interventricular septum and third ventricle are located in the midline, no subfalcine herniation is present (Fig. 2.5).
The symmetry of the brain is the key to radiologic evaluation. Only experience teaches how much asymmetry is within the range of normal variation. Generally, the sulcal pattern should be symmetric. The sulci on one side are the same size as the corresponding sulci on the other. The anterior interhemispheric fissure should be visualized. Loss of sulci may result from compression by a mass or opacification of CSF following subarachnoid hemorrhage or, less commonly, meningitis or CSF-borne tumor spread. The sulci extend to the inner table of the skull, but in older patients, some atrophy is normal and CSF may be visualized peripherally. Significant medial displacement of the sulci may represent compression resulting from an extracerebral fluid collection, such as a subdural or epidural hematoma. Because these may be bilateral and similar in density to the brain, care needs to be taken in evaluating the periphery of the brain.
Basal Cisterns. More subtle, but more important, signs of intracranial mass include distortion of the CSF spaces of the posterior fossa and the base of the brain. These key structures are the quadrigeminal plate cistern and the suprasellar cistern (Fig. 2.10). Because these CSF spaces are traversed by important neural structures, careful attention to these regions is essential. The quadrigeminal plate cistern in the axial plane has the appearance of a symmetric smile. Any asymmetry must be suspect, and abnormality of this cistern may represent rotation of the brain stem resulting from transtentorial herniation, effacement of the cistern by cerebellar or brainstem mass, or opacification of the cistern as in subarachnoid hemorrhage.
The suprasellar cistern looks like a pentagon, the Jewish star or the Hindu Shatkona, depending upon the angulation of the scan through it. The five corners of the pentagon are the interhemispheric fissure anteriorly, the Sylvian cisterns anterolaterally, and the ambient cisterns posterolaterally. The sixth point of the Jewish star or Shatkona is the interpeduncular fossa posteriorly. The cistern has the density of CSF and the structure is symmetric. The anatomic continuations of the cistern are the same density as CSF. Significant asymmetry may be a result of uncal herniation. Central mass may be the result of a sellar or suprasellar tumor. Opacification of the cistern may be the result of subarachnoid hemorrhage or meningitis.
Ventricles. The final structure that must be evaluated in a quick review of a brain scan is the ventricular system. It is best to start with the fourth ventricle in the posterior fossa because it is the hardest to see on CT. Asymmetry or shift of the fourth ventricle may be the only sign of significant intracranial masses. Because of the shape of the fourth ventricle, some asymmetry in appearance may reflect the patient’s position in the scanner.
The overall size of the ventricular system is assessed next. Enlargement of the lateral ventricles and third ventricle in the setting of headache, or with signs of intracranial mass, may represent hydrocephalus, a potentially fatal yet easily treatable condition. Hydrocephalus is distinguished from enlargement of the ventricular system as the result of atrophy by a discrepancy in the degree of ventricular and sulcal enlargement and by a characteristic pattern of disproportionate temporal horn
enlargement compared with the frontal horns and a rounded appearance of the anterior portion of the third ventricle.
enlargement compared with the frontal horns and a rounded appearance of the anterior portion of the third ventricle.
 Figure 2.15. Brain MR. Occipital horns of the lateral ventricles. Coronal plane T1-weighted image at 3 T. |
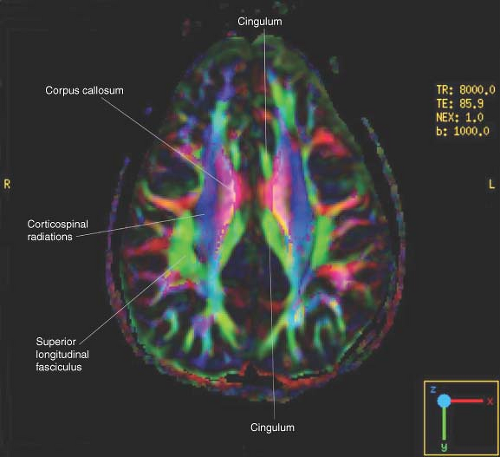 Figure 2.23. Diffusion Tensor Imaging. White matter tracts at the level of the centrum semiovale. Color-encoded fractional anisotropy maps derived from diffusion tensor data at 3 T. |
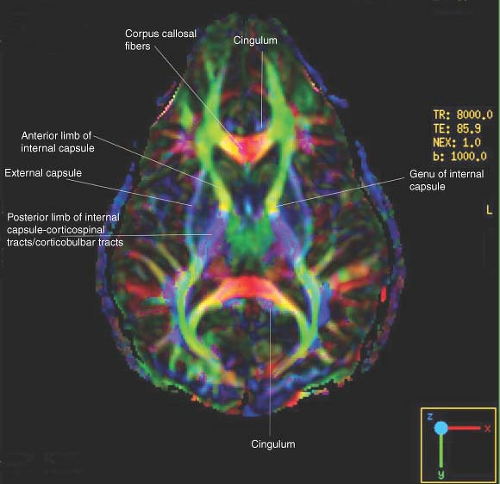 Figure 2.24. Diffusion Tensor Imaging. White matter tracts at the level of the internal capsule. Color-encoded fractional anisotropy maps derived from diffusion tensor data at 3 T. |
Emergency CT Checklist. When confronted with a CT scan under emergency conditions, radiologists must ask themselves the following five questions:
Is the middle of the brain in the middle of the head?
Do the two sides of the brain look alike?
Can you see the smile and the pentagon or Jewish star/Shatkona?
Is the fourth ventricle in the midline and more or less symmetrical?
Are the lateral ventricles enlarged, with effaced sulci?
If a radiologist can give the right answers to these five questions, there is no neurosurgical emergency. This approach leaves many important diagnoses unmade, but the diseases are either untreatable or treatment can safely be delayed several hours. It is important to note that thrombolysis candidates require close scrutiny of the basal ganglia and cortex for signs of early ischemia in addition to a search for acute hemorrhage. When stroke triage is performed, specialized imaging techniques such as perfusion CT and CT angiography (CTA) sometimes supplement the initial screening CT. In an increasing number of centers, MR stroke triage is performed provided that the clinical suspicion of intracranial hemorrhage is very low and no contraindication to MR is known. Remember to document the NINDS thrombolysis criteria: mass, bleed, and acute infarct.
Midline Structures. The anatomy of the midline of the brain is extremely complex and the structures are not duplicated so the principles of symmetry cannot be applied. The midline anatomy must therefore be learned in detail. There are three prime areas to study: the sella and suprasellar region, the pineal region, and the craniocervical junction.
Sella and suprasellar region. On virtually every MR examination, it is possible to localize the sella turcica, the pituitary gland, pituitary infundibulum, optic chiasm, anterior third ventricle, mammilary bodies, and anterior interhemispheric fissure (Fig. 2.10). Important vascular structures are also seen in this region. The tip of the basilar artery and the posterior cerebral arteries are seen posteriorly, and the anterior cerebral arteries are visualized anterior and superior to the sella. The anterior cerebral arteries travel in the interhemispheric fissure. Slightly off the midline the “s”-shaped carotid siphons and the posterior communicating arteries are visualized. Parallel to the course of the posterior communicating artery we frequently see the third cranial nerve. In the parasagittal location, near the optic chiasm, we see the optic nerve anteriorly and the optic tract posteriorly.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree