S piral (helical) computed tomography (CT) allows the entire chest to be imaged in a few seconds or less (i.e., during a single breath hold), with volumetric acquisition of scan data. Two- and three-dimensional reformations may be performed if desired. Because scanning is rapid, contrast agents can be injected quickly, excellent vascular opacification can be achieved, and reduced volumes of contrast agent can be used.
Multidetector CT (MDCT) scanners have multiple parallel rows of X-ray detectors (an ever-increasing number, now exceeding 250 in some scanners, and capable of reconstructing more than 500 slices at a time). With MDCT, each of the detector rows records data independently as the gantry rotates; consequently, a volume of the patient (e.g., up to 16 cm along the longitudinal axis, or z -axis, with a 256-detector scanner) is imaged with each gantry rotation. With large-area detector scanners, scanning of a volume may be performed without table motion; this is most useful for cardiac imaging. The gantry rotation time is 0.5 seconds or less.
Spiral Chest CT: General Principles
The specific protocols used for chest CT depend on the scanner used, the scanner manufacturer, and the reason for the study. However, several general principles apply to all chest scans ( Table 1.1 ).
|
|
|
|
|
|
|
|
|
|
Scan Levels
Chest CT is usually performed from a level just above the lung apices (near the suprasternal notch) to the level of the posterior costophrenic angles; these scans also encompass the diaphragm and the upper abdomen. The distance (or volume) needed to cover the thorax (usually 25–30 cm) is determined by a preliminary projection scan (e.g., a “scout view”).
Patient Position
Routinely, patients are scanned supine. Prone scans may be obtained for high-resolution CT (HRCT) or to assess movement of pleural fluid collections. The patient may also be positioned prone for biopsy of posterior lung lesions or drainage of pleural fluid collections.
Lung Volume
Scans are routinely obtained after a full inspiration (i.e., at total lung capacity) and during suspended respiration. Postexpiratory scans may be performed in some cases (particularly on HRCT) to assess air trapping.
Detector Row and Slice Thickness
Scan data are usually acquired with the thinnest detector width available on the scanner (detector rows on most scanners range from 0.25 to 0.625 mm), and the reconstructed slice thickness used for scan interpretation is determined by the indication for the scan. For example, if data are recorded with 0.625-mm detectors, slices can be reconstructed at any thickness from 0.625 to 5 mm for viewing. Thin slices are required for some specific indications, whereas thicker slices are quicker to interpret and do not occupy as much memory when they are stored.
Most chest scans are reconstructed with a 1- to 1.25-mm thickness. When one is viewing a study reconstructed with 2.5- or 5-mm-thick slices, if the scan data were collected using thinner detectors, and if the scan data are still available (they are usually preserved on the scanner disk for a day or two), you can have thinner slices reconstructed at a later time.
Usually slices are reconstructed at an interval equal to the slice thickness (e.g., 1.25 mm) to provide a volumetric data set. On occasion, scans are reconstructed at overlapping levels (e.g., 1.25-mm slices reconstructed at 0.625-mm intervals), although this is not generally necessary.
Pitch (Table Excursion)
The term pitch refers to the distance the table travels during a complete gantry rotation divided by the width of all the detectors used (e.g., table excursion/detector width × number of detector rows). With MDCT, pitch usually ranges from 1 to 2. The higher the pitch, the faster the scan, but images are generally noisier, spatial resolution is reduced somewhat, and the effective slice thickness (the thickness of the patient that is actually imaged) is increased.
Keep in mind that with the spiral technique the actual thickness of the slice you view (i.e., “effective slice thickness”) may be greater than the slice thickness you select (e.g., 1.25 mm), depending on the pitch or table excursion during gantry rotation; the greater the pitch, the greater the effective slice thickness. Thus there is a trade-off; with a higher pitch, the study is quicker but the scans are not quite as good.
Scan Duration
MDCT of the chest can be easily performed during a single breath hold (2.5 seconds or less), generally avoiding respiratory motion artifacts, except in very dyspneic or uncooperative patients.
Reconstruction Algorithm
Once the scans have been performed, the scan data are reconstructed using an algorithm that determines some characteristics of the resulting image. For routine chest imaging, a high-resolution algorithm is often used to optimize detail, but this makes the image somewhat noisy in appearance. A standard or soft-tissue algorithm , which produces a smoother image, is better for assessing thoracic vascular structures (e.g., studies performed for diagnosis of pulmonary embolism, aneurysm, or aortic dissection) but is not optimal for other chest imaging. This algorithm is often used for abdominal imaging.
Two- and Three-Dimensional Reconstruction
Because the scan data are acquired continuously and volumetrically by spiral CT, scans may be reconstructed in any plane desired. A variety of display techniques have been used for imaging the thorax. These include multiplanar reconstructions, three-dimensional shaded surface display or volume rendering from an external perspective, or shaded surface or volume rendering from an internal (i.e., endoluminal) perspective, also known as virtual bronchoscopy .
Multiplanar, two-dimensional reconstructions offer the advantage of being quickly performed and are sufficient for diagnosis in most cases in which a reformation is considered desirable. Subsequent chapters provide a number of examples of two-dimensional reconstructions. Three-dimensional techniques, such as shaded surface display and volume rendering, can be valuable in selected cases, but they are time-consuming and require operator experience. These techniques are not commonly used in day-to-day clinical chest imaging.
Maximum- or minimum-intensity projection images representing a slab of three-dimensional data reconstructed from a volumetric data set may sometimes be useful in imaging pulmonary, airway, or vascular abnormalities.
Window Settings
For chest CT, scans must be viewed with at least three different window settings. Scans are usually viewed with a workstation having preset windows available. The presets used when one is reading chest CT scans are generally termed lung , soft-tissue (or mediastinal ), and bone windows, names that also describe their primary use. These preset windows are often adjusted by the viewer during scan interpretation to optimize visibility of certain structures or abnormalities of interest.
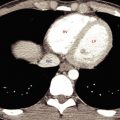
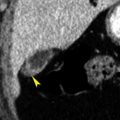
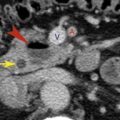
Lung windows typically have a window mean of approximately -600 to -700 Hounsfield units (HU) and a window width of 1000 to 1500 HU. Lung windows best demonstrate lung anatomy and disease, contrasting soft-tissue structures with surrounding air-filled lung parenchyma.
Mediastinal or soft-tissue windows (window mean 20–40 HU; window width 450–500 HU) demonstrate soft-tissue anatomy in the mediastinum and in other areas of the thorax, allowing the differentiation of fat, fluid, tissue, calcium, and contrast-opacified vessels. This window is also of value in providing information about consolidated lung, the hila, pleural disease, and structures of the chest wall. Subsequent chapters discuss more specific uses of these two windows. In the assessment of vascular structures (e.g., for pulmonary embolism or dissection diagnosis), a wider window or higher window mean than that used for a routine mediastinal window is often selected by the radiologist to better see detail within the dense contrast column.
Bone windows typically have a window mean of approximately 300 to 500 HU and a window width of 2000 HU. They best demonstrate skeletal structures or very dense objects. This window is sometimes valuable in looking at densely opacified vascular structures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree