Ischemic Heart Disease
QUESTIONS
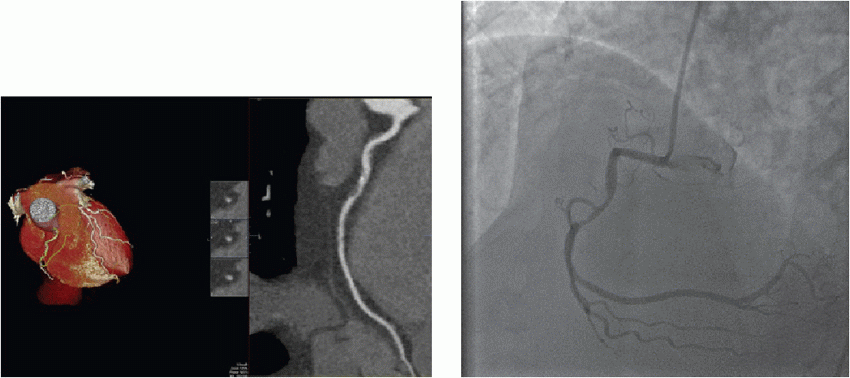
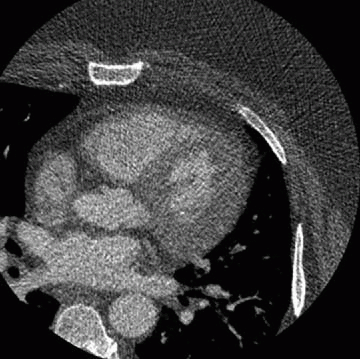
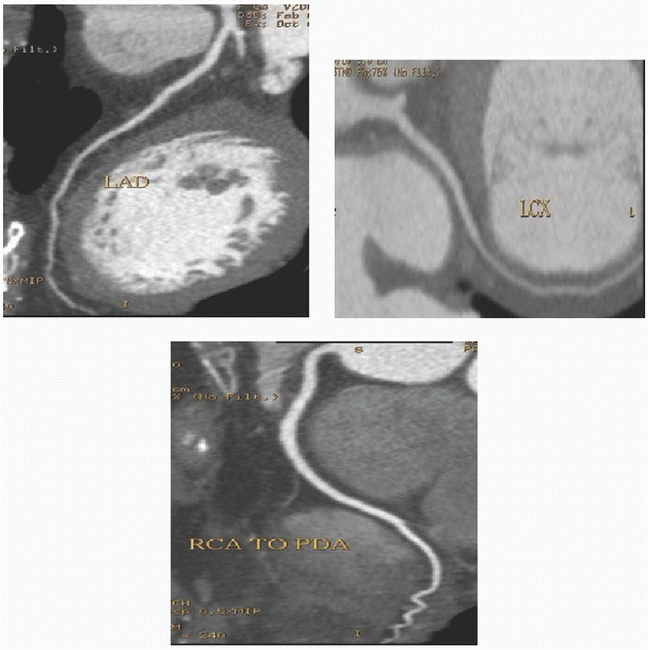
1 In the below images the abnormality of the right coronary artery is most closely associated with which of the following in this patient with chest pain but no EKG changes?
|
A. Lateral wall hypokinesis
B. Significant restriction of blood flow to the inferior wall
C. RCA occlusion
D. ST elevation myocardial infarction (STEMI)
View Answer
1 Answer B. The curved multiplanar reformat of the RCA (right-dominant system) demonstrates mixed plaque within the proximal vessel resulting in severe (roughly 80%) stenosis. A more proximal lesion consisting of noncalcified plaque causes 40% to 50% stenosis. A lesion is considered hemodynamically significant if it causes >70% stenosis. This is based on myocardial blood flow studies. The lateral wall is perfused by the circumflex, not the RCA. Contrast is noted throughout the lumen indicating partial patency. STEMI is caused by acute plaque rupture and acute total occlusion.
Reference: Uren NG, Melin JA, De Bruyne B, et al. Relation between myocardial blood flow and severity of coronary-artery stenosis. N Engl J Med 1994;330(25):1782-1788.
2 The use of which of the following drugs precludes the use of sublingual nitroglycerin for cardiac CTA?
A. Metformin
B. Sildenafil
C. Diltiazem
D. Atorvastatin
View Answer
2 Answer B. During coronary CTA, sublingual nitroglycerin (SL NTG) is given for coronary artery dilation. Use of phosphodiesterase inhibitors serves as a contraindication for SL NTG administration because of possible hypotension. A review of the patient’s medication list is mandatory prior to performing coronary CTA.
Reference: http://www.ctisus.com/learning/pearls/cardiac/patient-prep:-beta-blockers,-iv-contrast,-etc
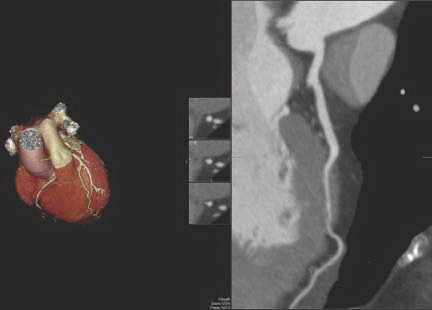
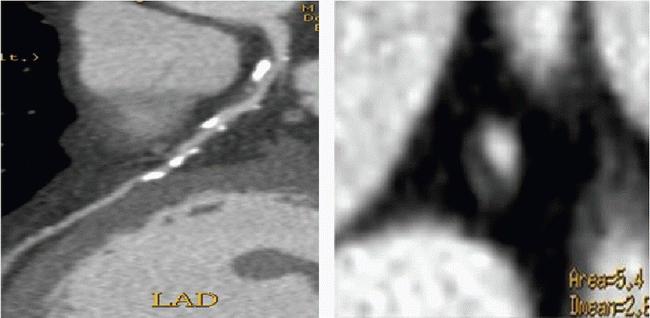
3 What treatment could be initiated for the condition shown in this patient with chest pain with exercise?
|
A. Sublingual nitroglycerin
B. Digoxin
C. Adenosine
D. Beta blockers
View Answer
3 Answer D. The curved multiplanar reformat of the LAD shows a long-segment intramyocardial bridge in the mid LAD. This is the most common site for bridging. Studies show that there is increased likelihood of ischemia with increasing depth and length of the bridge. Initial treatment is with beta blockers to unload the left ventricle. Refractory cases may be referred to surgery for unroofing.
References: Nakanishi R, et al. Myocardial bridging on coronary CTA: an innocent bystander or a culprit in myocardial infarction? JCCT 2012;6:3-13.
Vliegen HW, Jukema JW, Bruschke AVG. Congenital coronary artery anomalies. Anatomy, diagnosis, and management. Leiden, The Netherlands: TTMA B.V., 2012.
A. None
B. At least 1
C. At least 2
D. At least 3
View Answer
4 Answer C. The image shows a “nubbin” from an occluded vein graft arising from the aorta. Additionally, the left internal mammary artery (LIMA) is not along the chest wall like the right one, indicating that the LIMA has been used as a graft to (most likely) the LAD.
Reference: Frazier A, et al. Coronary artery bypass grafts: assessment “with multidetector CT in the early and late postoperative settings. Radiographics 2005;25:881-896.
5 What statement is correct regarding the patency of bypass grafts at 10 years?
A. LIMA > SVG
B. LIMA < SVG
C. LIMA = SVG
D. Indeterminate
View Answer
5 Answer A. Graft at 10 years was 61% for saphenous vein grafts compared with 85% for internal mammary artery grafts (p < 0.001).
Reference: Goldman, et al. J Am Coll Cardiol 2004;44(11):2149-2156.
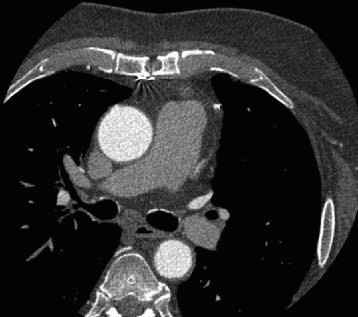
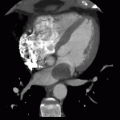
6 A coronary CTA is ordered for a 72-year-old patient with shortness of breath. As part of the examination, a calcium score is performed and the below image is obtained. (Total calcium score is calculated at 2,286 Agatston units.) Which of the following conclusions is accurate?
|
A. The patient has atherosclerotic plaque.
B. High-grade stenosis is likely.
C. The patient is at low risk for a coronary event.
D. Aortic stenosis is likely.
View Answer
6 Answer A. Coronary artery calcification occurs in proportion to underlying plaque burden but not degree of stenosis. While it has been shown that a calcium score of >100 AU carries a 5× increased risk of a coronary event than a score <100, the presence of high-grade stenosis cannot be accurately determined on a calcium score image alone, as this does not account for occult noncalcified plaque. Additionally, it is possible that calcium is mostly intramural and does not cause significant luminal narrowing.
References: Guerci AD, et al. Relation of coronary calcium score by electron beam computed tomography to arteriographic findings in asymptomatic and symptomatic adults. Am J Cardiol 1997;79:128-133.
Yadon, et al. J Am Coll Cardiol 2005;46(1):158-165.
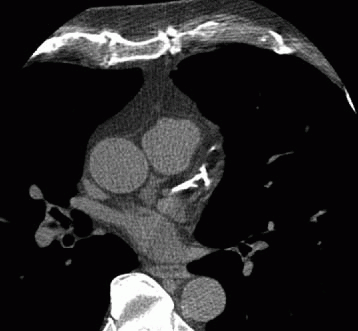
7 The following scan parameters were used to obtain the image in a patient with a heart rate of 60 beats per minute: kVp = 120; mA = 700; gantry rotation speed = 320 msec; contrast volume = 80 mL; contrast rate = 6.5 mL/sec; and slice width = 0.625 mm. The poor image quality in this case is most likely from
|
A. Poor temporal resolution
B. Increased body mass index
C. Incorrect contrast timing
D. Too high spatial resolution
View Answer
7 Answer B. All scan parameters listed above are within reasonable protocol limits. The body habitus in this patient, however, is causing significant attenuation of the x-ray and increased image noise. BMI > 39 can potentially lead to nondiagnostic studies and is a relative contraindication.
Reference: Raff, et al. SCCT guidelines on the use of coronary computed tomographic angiography for patients presenting with acute chest pain to the emergency department: A Report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovas Comput Tomogr 2014;8:254 e271.
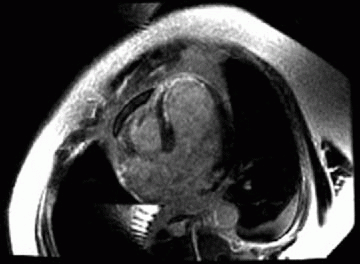
8 A 66-year-old patient is status post myocardial infarction 2 days ago. Which of the following conclusions can be made?
|
A. There is thrombus at the apex.
B. The septal myocardium is viable.
C. The lesion was most likely in the left circumflex coronary artery.
D. The septum is normokinetic.
View Answer
8 Answer B. Infarcted tissue demonstrates subendocardial enhancement or (when extensive) transmural enhancement. If less than 50% of the affected wall demonstrates scarring/enhancement, it is deemed viable, and revascularization has been shown to improve postinfarction ejection fraction and clinical outcome.
References: Cummings, et al. A pattern based approach to assessment of delayed enhancement in nonischemic cardiomyopathy at MR imaging. Radiographics 2009;29:89-103.
Kim R, et al. The use of contrast enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. NEJM 2000;343(2):1445-1453.
9 A 50-year-old male with no past medical history presents for coronary CTA. What is the treatment of choice for the lesion in the left main coronary artery?
|
A. Angioplasty
B. Stenting
C. Bypass grafting
D. Lifestyle modification and statin therapy
View Answer
9 Answer C. The curved multiplanar reformat of the left main and LAD shows mixed plaque within the LM resulting in greater than 50% stenosis. A lesion is considered hemodynamically significant if it causes >50% stenosis in the left main. This is based on myocardial blood flow studies. A greater than 50% lesion in the left main is an indication for coronary artery bypass grafting.
References: Uren NG, Melin JA, De Bruyne B, et al. Relation between myocardial blood flow and severity of coronary-artery stenosis. N Engl J Med 1994;330(25):1782-1788.
Eagle KA, et al. ACC/AHA guidelines for coronary artery bypass graft surgery: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1991 guidelines for coronary artery bypass graft surgery). Circulation 1999;100(13):1464-1480.
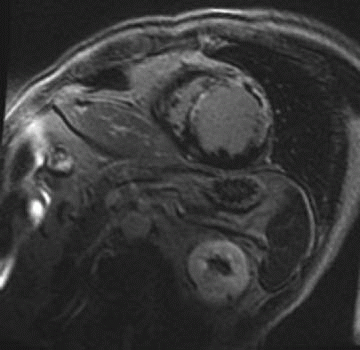
10 Which of the following statements is correct regarding the area of low signal in the anterior wall on this delayed enhancement sequence?
|
A. It is an area of normal nulled myocardium.
B. It represents an area without reflow and carries a less favorable prognosis.
C. It represents hibernating myocardium.
D. It indicates that a suboptimal inversion time was used during acquisition.
View Answer
10 Answer B. Microvascular obstruction (MVO), also known as no-reflow phenomenon is a focus of infracted myocardium where obstruction of the microvasculature does not allow contrast to perfuse the tissue. Following infarction, administered contrast resides in the interstitium and creates the scar seen on delayed enhancement images. In areas where the microvasculature is obstructed, the contrast never reaches the interstitium, and this tissue appears as very dark signal surrounded by an enhancing scar on both sides. MVO is recognized as a poor prognostic indicator and marker of subsequent adverse LV remodeling.
Reference: Wu K. CMR of microvascular obstruction and hemorrhage in myocardial infarction. JCMR 2012;14:68.
11 Which of the following clinical scenarios is an appropriate indication for coronary CTA based on current Appropriateness Criteria Guidelines?
A. Acute myocardial infarction with ST elevation
B. Preoperative clearance for orthopedic surgery in a 70-year-old male with diabetes
C. Persistent symptoms (chest pain) with a normal ECG stress test
D. Coronary CTA in a patient with a known 2.0-mm stent in the LAD to assess disease
View Answer
11 Answer C. Coronary CTA has a negative predictive value greater than 95% and is an excellent test to exclude coronary artery disease. In particular, it has been shown to be of value when evaluating low risk patients with atypical chest pain, low risk patients with negative or equivocal stress testing an in the emergency room setting to evaluate patients with acute chest pain who are of low- to medium-risk (shown in ACRIN-PA and ROMICAT-II clinical trials).
Reference: Taylor, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate use criteria for cardiac computed tomography. Evaluation of graft patency after CABG has an appropriateness score of 8/9 in a symptomatic patient. Circulation 2010;122:e525-e555.
12 A 40-year-old female patient presents to the ER with chest pain, negative cardiac enzyme tests and a normal EKG. A review of the medical record reveals she presented 2 months prior with similar symptoms. At that time, she underwent a coronary CTA, which was normal. What is the next step?
A. Repeat coronary CTA
B. Admission and stress test
C. Catheter angiography
D. Evaluate for possible noncardiac causes of chest pain.
View Answer
12 Answer D. Long-term data is now available for patients who underwent coronary CTA in the emergency room. Current data suggests that a normal CTA in a low-risk patient presenting to the ER has a “warranty period” of up to 2 years meaning a rescan is not necessary as there has been no recorded incident of ACS within 2 years in this population.
Reference: Schlett, et al. Prognostic value of CT angiography for major adverse cardiac events in patients “with acute chest pain from the emergency department. JACC Cardiovas Img 2011;4(5):481-491.
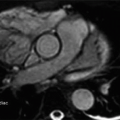
13 A 39-year-old male with no past medical history presents to the ER with chest pain. The workup reveals a normal ECG and negative cardiac enzymes. He undergoes a coronary CTA angiogram (shown below). Based on the images and clinical trials, which of the following is a reasonable plan of disposition?
|
A. Discharge to home
B. Admit to telemetry
C. Stress test
D. Cardiology consult for possible catheterization
View Answer
13 Answer A. Several clinical trials such as ACRIN-PA, CT-STAT, and ROMICAT have demonstrated the utility of coronary CTA for low-risk emergency room patients presenting with chest pain. Current data supports the position that a CCTA-based strategy for low- to intermediate-risk patients presenting with a possible acute coronary syndrome allows for the safe, expedited discharge home rather than admission and continued monitoring.
Reference: Litt HI, et al. CT angiography for safe discharge of patients “with possible acute coronary syndromes. N Engl J Med 2012;366:1393-1403.
14 A patient presents for cardiac MRI 3 days following myocardial infarction. On admission, catheterization reveals severe stenosis in the left anterior descending and right coronary arteries. On admission day 2, new-onset mitral regurgitation is discovered, and the patient develops right upper lobe pulmonary edema. What complication of infarction should be considered?
A. Aneurysm formation
B. Thrombus formation
C. Papillary muscle infarction
D. Pericardial effusion
View Answer
14 Answer C. Myocardial infarction carries many associated complications that include apical aneurysm formation, decreased ejection fraction, ventriculoseptal defect formation and papillary muscle infarction.
In one study, the incidence of rupture of the papillary muscle was found to be 0.9%. The clinical features usually occur during the first week after infarction. More common is slight mitral regurgitation without pulmonary edema from papillary muscle dysfunction.
Reference: Clements, et al. Ruptured papillary muscle, a complication of myocardial infarction: clinical presentation, diagnosis, and treatment. Clin Cardiol 1985;8:93-103.
15 Which of the following features of the plaque shown deem it high risk for development of an acute coronary syndrome?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree