Abstract
This chapter discusses drivers, domains, and concepts of quality improvement (QI). Communicating drivers can be useful in convincing stakeholders and are often the initial step in creating a culture of improvement. Drivers include our ethical commitment to avoiding harm and taking good care of patients, our fiscal responsibility as medical professionals, and the need for bringing scientific evidence to patient care much faster. Many frameworks exist to look at QI, such as the Donabedian model of structure, process, and outcome, or the six aims for patient care set forth by the Institute of Medicine: safe, timely, efficient, effective, equitable, and patient centered. Other key elements of QI include the aspiration to become a high-reliability organization, using Deming’s approach of profound knowledge, and creating a safety culture that understands human errors and values a just culture.
Keywords
Donabedian model, high-reliability organizations, IOM aims, key concepts, narrative of harm
Concepts for Quality Improvement
Quality improvement (QI) methods are not new; they are just relatively new to the healthcare industry and the field of radiology. As a result, there is currently a gap between the high desire and need to apply QI methods in daily practice and a lack of radiologists who are sufficiently trained in the proper use of these methods. In response to this gap, many medical schools and radiology residency programs have now started to teach QI methods to medical students and residents, and the American Board of Radiology (ABR) has incorporated QI into the certification exam curriculum.
Before delving into the study and application of QI methods, several key concepts in QI need to be understood. For example, to solicit and motivate a local QI team, one needs to understand and communicate the reasons why we embark on QI initiatives. A basic understanding of the major domains of QI is necessary when identifying QI projects that support the greater mission for improvement in healthcare. To execute QI methods successfully, several basic philosophical principles need to be applied and are described here.
Drivers of Quality Improvement
What drives us to do QI in radiology? How can we persuade the skeptics to join our efforts? The rationale for doing QI encompasses ethics, the economy, science, and gripping patient narratives ( Fig. 2.1 ).
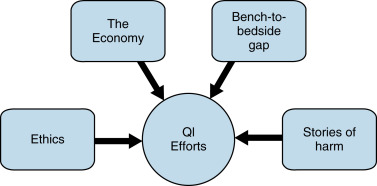
Physicians practice according to high ethical standards and principles , such as those attributed to Hippocrates in the Hippocratic Oath . The statement Primum non nocere (First, do no harm) is frequently quoted when promoting QI in healthcare. Just how do we harm patients in healthcare today? According to the 1999 Institute of Medicine (IOM) report To Err Is Human , preventable causes of patient deaths are the result of erroneous or delayed diagnoses, treatment errors such as a wrong operation and medication errors, failure to give prophylaxis, inadequate monitoring/follow-up, and communication and equipment failures. The IOM reported in 1999 that between 44,000 and 98,000 people died in hospitals each year as a result of preventable medical errors. An analysis published in 2013 estimated that there are more than 400,000 premature deaths associated with preventable harm to patients per year. How can we simply go on about our business in light of such shocking numbers? What happened to Primum non nocere ? I do not know about you, but I have a sense of urgency to start improving patient care!
There is also an economic argument supporting QI in healthcare. As of the first quarter of 2014 the total US net worth was estimated to be $269.6 trillion, the national debt was $145.8 trillion, and the annual gross domestic product (GDP) was $123.8 trillion. Very plainly, we are in debt because we spend more than we produce, and healthcare is one of the areas where we spend a lot (Kaiser Family Foundation [KFF]). In 2009, health spending per capita in the United States was $7598, which was 48% higher than in the next highest spending country, Switzerland (KFF). Despite this high investment in healthcare, the United States does not appear to achieve substantially better health outcomes. For example, in 2015 the Central Intelligence Institute (CIA) ranked US life expectancy No. 43, while Switzerland ranked No. 9 (CIA). The discrepancy between high spending and suboptimal outcomes is explained by a multitude of factors. About half of the spending growth in healthcare is being attributed to the availability of new medical technology. The development and use of healthcare technology are thriving because health insurance bears a substantial share of the incurred cost to patients (KFF). Another factor contributing to rising healthcare costs is the aging of the US baby boomer population. Baby boomers are expected to have more health problems and require more care between 2012 and 2022. In addition, about 20% or more of total healthcare expenditures are being attributed to various forms of waste (overutilization, failed care coordination or failed care delivery, and administrative waste, fraud, and abuse) (KFF). According to a Kaiser Health Tracking Poll, rising healthcare costs have caused many American families to cut back on medical care by using home remedies rather than medical professionals, cutting back on dental care, or postponing the care they need. Many of these issues need to be addressed at a political level, through legislation and modifications to our insurance payer system. However, eliminating waste from the system can be done locally, by anyone, right now.
Another big driver for QI in healthcare is to provide more effective care , meaning care that is proven to achieve its purpose. There is currently a wide temporal gap between publication of scientific knowledge and its application to patient care. It is said, for example, that it takes 17 years for research evidence to reach clinical practice, due to the time required and the complexities of performing basic research, translating lab results into human trials, using experiences in humans for clinical trials, becoming a practice guideline, and becoming an established practice. There are time-consuming matters of getting access to facilities and funding, addressing human subject protection, federal regulations for drug and device development, and efforts invested in manuscript writing that have to be surmounted prior to publication. In addition, all practitioners harbor a wealth of cognitive biases against new treatments and processes and it has been shown that these cognitive biases can cause underuse of effective new strategies in favor of old suboptimal therapies. Closing the gap between research and clinical practice can be as simple as review and implementation of one of the many clinical guidelines or American College of Radiology (ACR) appropriateness criteria, which are built on current scientific knowledge.
When logic and science fail to persuade others of the importance of QI in radiology, there is still a possibility that a narrative of harm can do so. The story of harm is very similar to an account given in mortality and morbidity (M&M) meetings. In contrast to M&M accounts, the story of harm may be told by the person who experienced the harm (usually the patient or a relative) or by the caregiver involved in events that caused harm and is always told in a setting that is supportive of the narrator and with an emphasis on learning from mistakes. A story of harm appeals at an emotional level and can be a strong motivator for joining or initiating QI efforts.
Twenty-eight-year-old Angela Myers was awaiting an outpatient angiogram for an arteriovenous malformation on her leg. She was very anxious about the impending procedure. The patient spoke English and appeared to be of average intelligence. David, a 45-year-old interventional radiology (IR) technologist: “ I went to the waiting room to meet my next patient. I picked up the chart that was next to this patient. The chart had the correct name for my next patient. I verbally stated the patient’s name and this woman confirmed her name. She also confirmed other information, including the type of procedure. I walked the patient to the IR suite and had her positioned on the IR table. The certified nurse anesthetist checked the patient’s wristband and alerted me that this was not the correct patient for the uterine fibroid embolization procedure. I was shocked. I apologized. I explained she was in the wrong room. I had to take the patient off the IR table and return her to the waiting room.” Upon reflection David realized: “ This patient was so anxious she was not actually hearing much of anything I said to her. She continued to agree and confirm whatever I said to her. The error on my part was that I stated her name, and did not check her wristband.” Luckily, the error was caught and the patient was not harmed. As David recalled, “ I learned a serious lesson, which I certainly had been taught by my supervisor, which is to always check the wristband. I don’t know just how far this mistake would have gone, because the patient is frequently asleep when the surgeon enters the suite. I now reinforce the importance of always checking the wristband whenever I have an opportunity to with my colleagues. ”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree