Knee
Patellofemoral Joint
Vertical Position of the Patella, Patellar Dystopia
Insall–Salvati Index
The Insall–Salvati index is perhaps the most widely used method for measuring the vertical position of the patella. On a lateral radiograph of the knee, the greatest diagonal length of the patella (LP) is measured from its posterosuperior corner to the apex. The length of the patellar tendon (LT) is measured from the patellar apex to the tibial tuberosity. The ratio of these two measurements (LP/LT) is the Insall–Salvati index ( Fig. 3.1 ).
Insall–Salvati index
• Normal range: | LP/LT = 0.8–1.2 |
• High-riding patella (patella alta): | LP/LT < 0.8 |
• Low-riding patella (patella baja, patella infera): | LP/LT > 1.2 |
Since the measurement is largely independent of joint position, it can be performed on routine X-ray films. The radiographs used by Insall and Salvati were obtained between 20° and 70° of knee flexion.
Insall J, Salvati E. Patella position in the normal knee joint. Radiology 1971;101(1):101–104 Insall J, Goldberg V, Salvati E. Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res 1972;88:67–69Caton–Deschamps Index
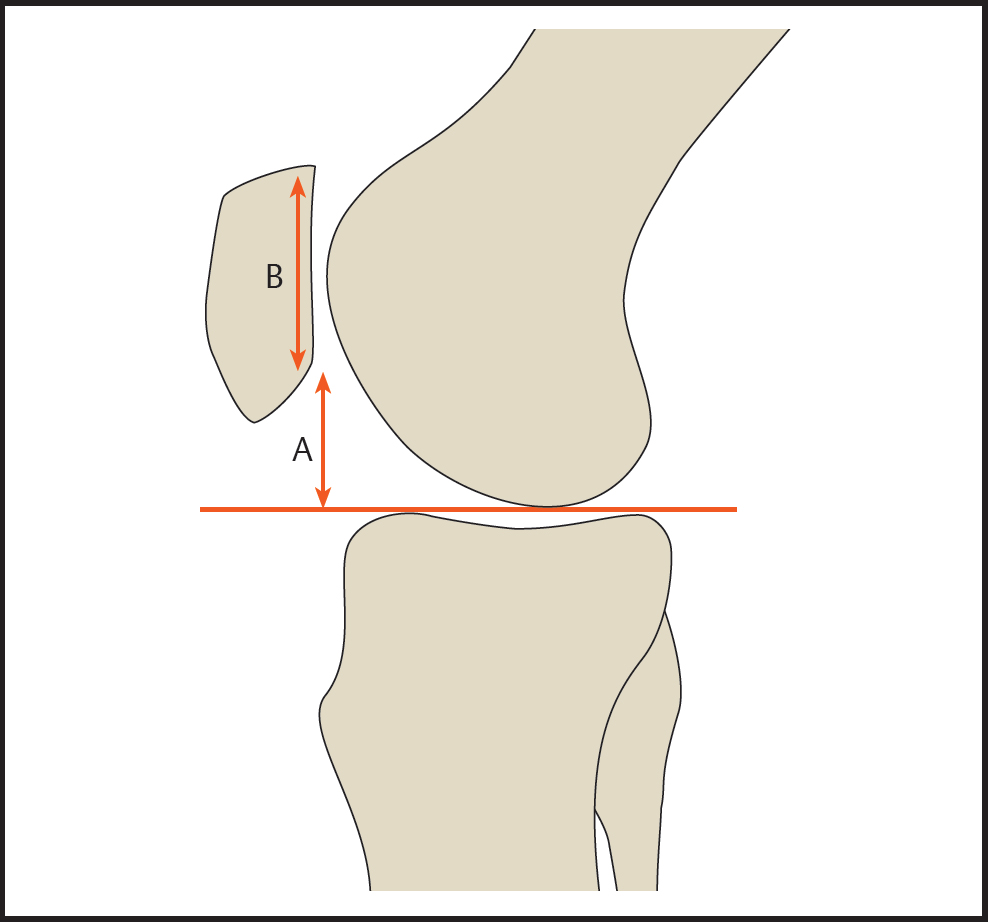
In the Caton or Caton–Deschamps method, the vertical position of the patella is defined by the ratio of the distance from the inferior border of the patellar articular surface to the anterior border of the upper tibia (B) and the length of the patellar articular surface (A) ( Fig. 3.2 ). The measurements are made on a lateral radiograph of the knee, which may be flexed between 10° and 80°.


Caton–Deschamps index
Normal range: B/A = 0.6 or 0.8–1.2
High-riding patella (patella alta): B/A ≥ 1.2
Low-riding patella (patella baja, patella infera): B/A ≤ 0.6
Blackburne–Peel Index
The method proposed by Blackburne and Peel for measuring patellar height differs from the two previous methods by its more precise definition of the distal reference point. First a line is drawn along the tibial plateau, and the perpendicular height of the lower edge of the patellar articular surface from the tibial plateau line is determined (A). The length of the patellar articular surface (B) is then measured, and the ratio A/B gives the Blackburne–Peel index ( Fig. 3.3 ). The measurements are made on a lateral radiograph of the knee flexed at least 30° to tighten the patellar tendon.
Blackburne–Peel index
| A/B = 0.8 (0.6–1) |
| A/B > 1 |
The reproducibility of the Insall–Salvati index is limited by inaccuracies in identifying the insertion of the patellar tendon. Because the index is not changed by surgical advancement of the tibial tuberosity, this method is not very useful for preoperative planning. The Caton–Deschamps and Blackburne–Peel indices are advantageous in this respect.
Horizontal Position of the Patella, Patellar Dystopia
Congruence Angle
The congruence angle of the patellofemoral joint describes the relationship between the patella and the trochlear articular surface of the femur. It is influenced by the shape of the patella and trochlea (dysplasia) and especially by the mediolateral position of the patella (lateral patellar shift). The congruence angle is measured on an axial “sunrise” view of the patella. First, the deepest point of the trochlea is identified (A), and the highest points on the medial (B) and lateral femoral condyles (C) are marked. The angle formed by lines AB and AC is the sulcus angle (see below). The bisector of that angle is drawn as reference line AO. Next the lowest point on the articular ridge of the patella (D) is determined. The angle between an extension of line AD and reference line AO is the patellofemoral congruence angle (α, Fig. 3.4 ). If line AD is medial to AO, the angle has a negative value; if AD is lateral to AO, the angle is positive.

Patellofemoral congruence angle
Mean value: α = – 6°
Standard deviation: 11°
Abnormal: α > + 16°
Axial Linear Patellar Displacement
Axial linear patellar displacement provides a simple, reproducible alternative to the patellofemoral congruence angle. On a sunrise view of the patella, a line is drawn between the highest points on the medial (M) and lateral (L) femoral condyles, and a perpendicular is dropped from that line through the deepest point of the trochlear sulcus (S). Another perpendicular is dropped from the lowest point on the patellar ridge (P). The distance between the two perpendicular lines equals the axial linear patellar displacement ( Fig. 3.5 ). Its value is expressed in mm.
Axial linear patellar displacement
Normal range: ≤ 2 mm
Abnormal lateralization: > 2 mm
The absolute value of the measured axial linear patellar displacement depends on the magnification factor of the radiograph. This limits the value of comparative measurements, especially between different institutions and in scientific studies. The patellofemoral congruence angle appears to be a more reproducible measurement.

Patellar Tilt
Patellar tilt refers to an abnormal angulation of the patella in the horizontal plane. The degree of tilt can be quantified in various ways. Common tools are the lateral patellofemoral angle of Laurin and the patellar tilt angle of Grelsamer.
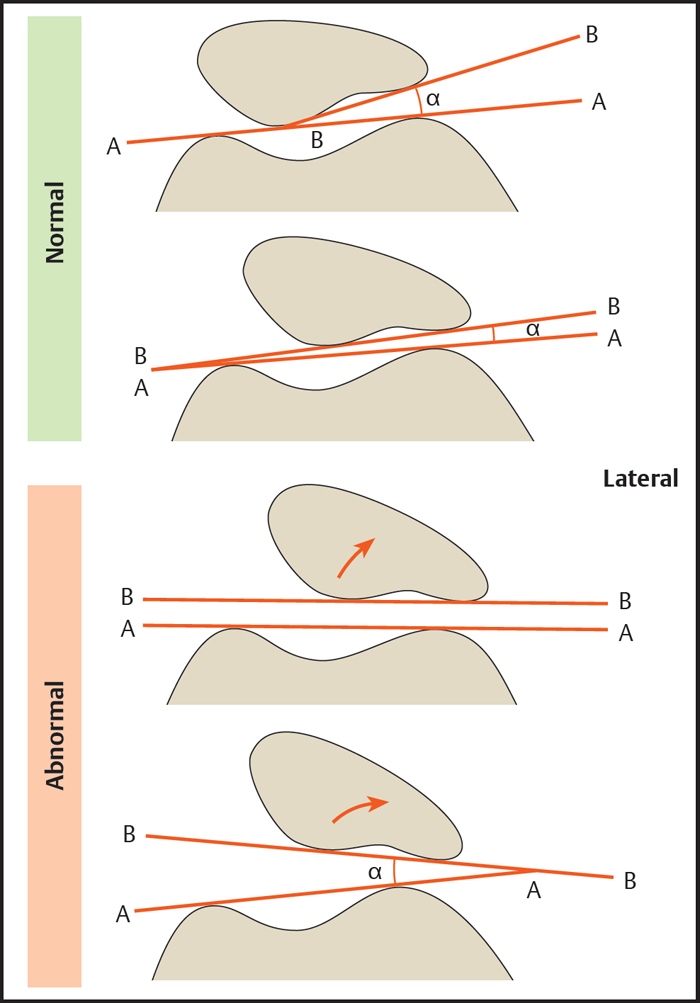
Lateral Patellofemoral Angle of Laurin
The lateral patellofemoral angle is determined on the patellar sunrise view by drawing a line tangent to the highest points on the medial and lateral femoral condyles (A) and drawing a second line (B) across the lateral patellar facet ( Fig. 3.6 ). In a normal joint, these lines will typically form an acute angle that opens on the lateral side. In patients with patellar instability, the lines will often be parallel or may even form an angle that opens on the medial side.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree