Fig. 11.1
AP and lateral views of an aseptic loosening of the tibial tray in total knee arthroplasty

Fig. 11.2
AP view of an aseptic loosening of the tibial tray in unicompartmental knee arthroplasty
11.4.1.5 Metal Synovitis
Metal-induced chronic synovitis results from metal wear debris caused by abrasion of metal components that occurs after failure of the interposed polyethylene-bearing surfaces. A line of linear opacity outlining a distended knee capsule or an articular surface on radiographs (metal line sign) is secondary to the deposit of metal debris in the joint causes and is diagnostic of metal synovitis.
11.4.1.6 Patellar and Extensor Mechanism Complications
The majority of patellar complications are commonly ruled out using both lateral and axial radiographs. Instability/dislocation and loosening of patellar components as well as stress patellar fractures are the most common complications reported. Patellar instability is related to imbalance of soft tissue (tight lateral retinaculum) and malposition and malalignment of components (Fig. 11.3). Tilt and subluxation of the patella are usually recognized on the axial views, although any underlying rotatory malalignment of components is best assessed on CT. The thin polyethylene liner may wear or displace from the metal backing into the Hoffa fat pad.
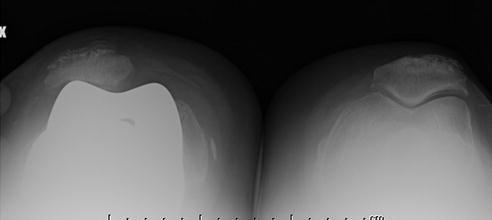
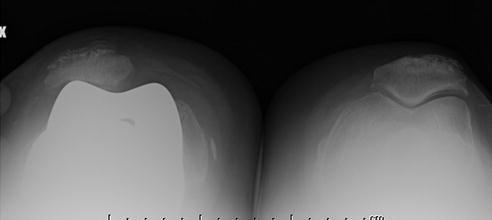
Fig. 11.3
Merchant view of patellar maltracking with lateral tilt in total knee arthroplasty
Patellar fractures have been reported to be up to 21 % of cases and are commonly seen in older patients [19]. Over-resection of the patella may predispose to fractures. Radiographs can easily detect fatigue fractures, which occur frequently at the peg-plate junction of metal-backed prosthesis. Occult fractures may be ruled out by MRI study. Quadriceps tendon tear and ruptures have also been described, resulting in abnormal position of the patella observed on radiographs. Ultrasonography and MRI confirms these complications. Fibrosis and scarring of the Hoffa pad may result in a low-lying patella (patella baja) [5].
11.4.1.7 Infection
The prevalence of infections in knee arthroplasty ranges from 0.5 to 2 % [5]. Infection is typically seen within the first 2 years of surgery, although sometimes may occur later. The diagnosis of low-grade and chronic infection may be particularly difficult, and the evidence of infection is often not obvious prior revision surgery. Microorganisms, introduced at the time of surgery (usually skin bacteria) or through hematogenous spread or direct contamination from compromised adjacent tissues, adhere to the prosthesis, residing in a biofilm that limits the effects of antimicrobial agents.
Conventional radiography does not show a high sensitivity since the appearance of infection can be variable, besides radiographs are normal in most patients. Radiologic distinction between septic and aseptic loosening can be challenging (Fig. 11.4). Periosteal reaction, periprosthetic widening, osteolysis, presence of bone destruction as well as irregular periprosthetic lucency or lucency that extends completely around the prosthesis are all signs which suggest septic loosening. Soft tissue swelling is also indicative for infection.


Fig. 11.4
AP view of septic loosening of a total knee replacement
Ultrasound is useful to detect joint effusions, soft tissue fluid collections, and in some cases, synovial hypertrophy and inflammation (aided by the use of color and power Doppler). The more advantageous use of ultrasound, however, is to guide intervention such as joint aspiration. Joint aspiration is a useful confirmatory test showing sensitivity and a specificity ranging from 67 to 82 % and from 91 to 95 %, respectively [20, 21]. In spite of the past limitation due to metal artifacts, nowadays, CT and MRI are useful tools to assess the extent of soft tissue infection in close proximity to the arthroplasty (Fig. 11.5).
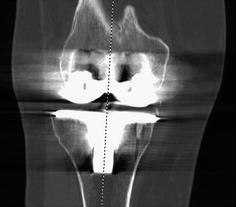
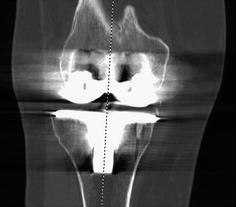
Fig. 11.5
CT scan in a correctly positioned total knee arthroplasty
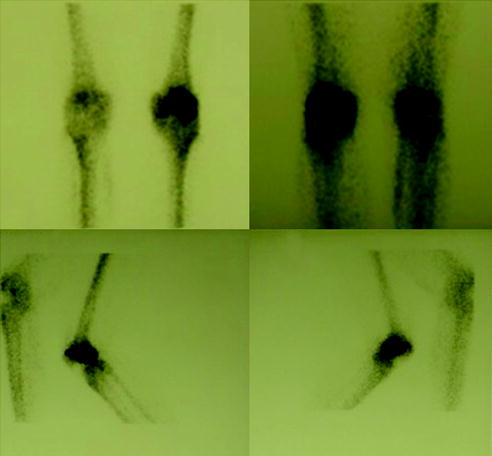
Nuclear medicine studies are extremely useful in the evaluation prosthetic complications. Bone scan, performed with technetium-99 m (Tc-99 m)-labeled diphosphonates, is highly sensitive for detecting complications of lower extremity prosthetic joint surgery (Fig. 11.6). Both infection and aseptic loosening may show increased uptake on delayed images, but the test is not specific mostly in the early post-operative period [22]. Furthermore, even in the absence of complications, persistent periprosthetic activity has been shown to be increased for up to 2 years because of continued post-operative reparative osteoblastic activity, and performing the bone scan as a three-phase study does not improve the accuracy of the test. As a matter of fact, the blood pool images may also show increased activity in both loosening and infection. Despite the overall accuracy of bone scintigraphy in evaluation of the painful prosthetic joint is about 50–70 %, this study has a high negative predictive value and a negative bone scan excludes both loosening and infection. Therefore, it may be use as an initial screening test in conjunction with other diagnostic tests [22].