Fig. 11.1
The acetabular labrum outlines the rim of the acetabulum from anterior to superior and posterior. Inferiorly, at the margins of the acetabular notch, it merges imperceptibly with the transverse ligament
The labrum provides stability against femoral head translation by increasing the depth of the acetabulum [2]. It also provides a seal, which aids in keeping synovial fluid in the intra-articular space, thus facilitating joint lubrication and load distribution [3, 4]. The hydrostatic fluid pressure within the intra-articular space enhances joint stability, whereas disruption of the fluid seal can make the joint unstable.
Lesions of the labrum typically present with groin pain and mechanical symptoms such as clicking or locking, although atypical symptoms for labral lesions are not uncommon [5]. Notably, labrum pathology is associated with early osteoarthritis (OA) of the hip joint, whereas disorders of the labrum have been reported to potentially precede articular cartilage damage [6, 7]. Therefore, early diagnosis and reliable determination of the location and severity of labrum pathology are important to allow for a timely surgical intervention, and thus obviate the risk for the development of advanced osteoarthritic damage. Furthermore, exclusion of differential diagnoses or recognition of potential etiologies such as trauma, femoroacetabular impingement (FAI) (Fig. 11.2), Legg Calvé Perthes disease, hip dysplasia, and degeneration is a clinical necessity [5].


Fig. 11.2
PD-weighted radial MR arthrogram depicting a detached labrum and cartilage signal changes at the anterior-superior aspect of the hip joint of a symptomatic cam-FAI patient. Note the non-spherical shape of the femoral head along with insufficient femoral head–neck offset that causes mechanical impaction involving the proximal femur and acetabular rim, inducing labral failure and varying degrees of cartilage damage
Magnetic resonance imaging (MRI) and MR arthrography (MRA), with their superior soft tissue contrast and capability of multiplanar imaging, are the modalities of choice in noninvasively visualizing the hip joint. Nevertheless, the acetabular labrum may be difficult to image due to its small size, curved orientation, variable morphological appearance, redundancy of the joint capsule when not distended, and several technical limitations such as volume averaging and a decrease in signal intensity owing to the relatively large distance between the labrum and the coil.
This chapter reviews the technical aspects of MRI and MRA in the evaluation of labrum pathology. Approved imaging protocols at 1.5 and 3 T, including two-dimensional (2D) and three-dimensional (3D) sequences, are provided. It also illustrates the radiological appearance of commonly encountered conditions and seeks to raise awareness of potential pitfalls.
Technique
Non-contrast Magnetic Resonance Imaging Versus Magnetic Resonance Arthrography
Numerous studies seeking the most appropriate method for imaging the hip joint and labrum have been performed. While most studies have revealed superior diagnostic accuracy for acetabular tears when using MRA (sensitivity values ranging from 66 % [8] to 100 % [9]), current reports also indicate high diagnostic accuracy without the instillation of contrast medium by using high-resolution, proton-density (PD)-weighted MRI (reported sensitivity values of 94 % [10] to 100 % [11]).
A recent meta-analysis indicated that both non-contrast MRI and MRA provide acceptable accuracy in evaluating the acetabular labrum [12]. However, in particular at 1.5 T, the sensitivity of MRA in detecting acetabular labral tears was to some extent greater when compared to conventional MRI, although considerable variations and/or limitations in methodology (i.e., inapplicable sequence setting when performing non-contrast MRI) have to be taken into account.
There are advantages and disadvantages with both non-contrast MRI and MRA. The intra-articular application of contrast medium in MRA facilitates the detection of labrum pathology by distending the hip capsule off the labrum, outlining the labrum with contrast, and by filling any clefts that are associated with labral tears and labrum detachment. Thereby, even distinct fissures within the labrum surface and at the transitional zone between the labrum and cartilage or subchondral bone can be identified (Fig. 11.3). The intra-articular technique, on the other hand, is certainly more invasive and uncomfortable for the patient, needs a more stringent sterile environment, and poses, although extremely rare, the risk of joint infection that could turn out to be disastrous. The non-contrast approach may be less sensitive for subtle labral surface changes but it is noninvasive and no extra time and expenses are required to process its application. Of note, the sensitivity in detecting intra-labral changes, which have no connection to the labrum surface, is similar for both non-contrast MRI and MRA (Fig. 11.4).
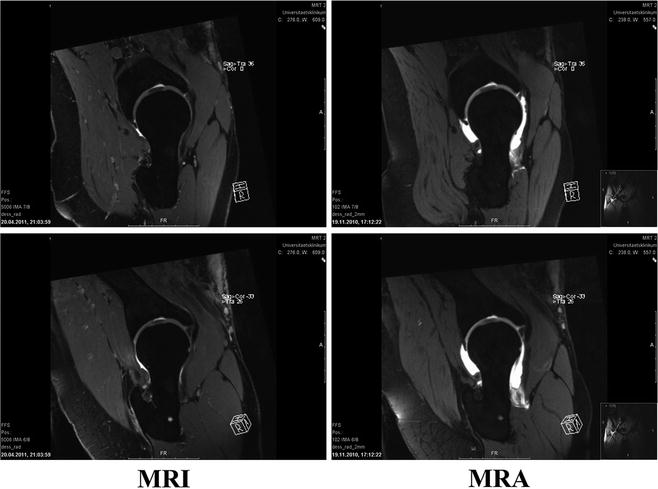
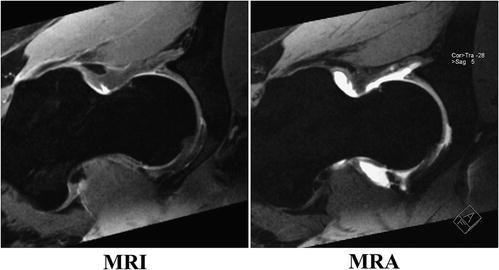
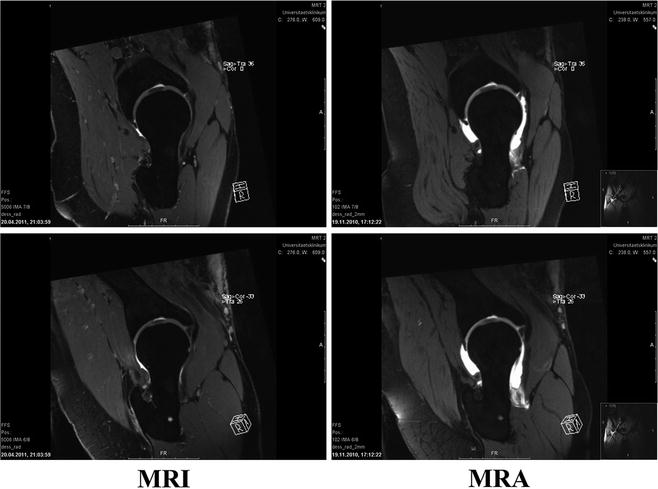
Fig. 11.3
Corresponding 3D DESS MRI (left) and MRA (right) reformat revealing minor, yet important, differences between both MR imaging techniques. The intra-articular application of contrast medium in MRA facilitates the detection of labrum pathology by distending the hip capsule off the labrum, outlining the labrum with contrast, and by filling any clefts that are associated with labral tears and labrum detachment. Thereby, fissures within the labrum surface and at the transitional zone between labrum and cartilage or subchondral bone may be better identified than with MRI
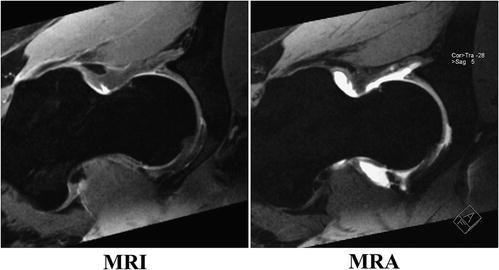
Fig. 11.4
Corresponding 3D DESS MRI (left) and MRA (right) reformat revealing no differences between both MR imaging techniques in detecting intra-labral changes, which have no connection to the labrum surface
Indirect MRA after intravenous contrast medium application has been reported to be an effective means of hip evaluation for labral tears [13]. The motivation to perform indirect MRA is that it provides superior contrast resolution relative to non-contrast MRI, but it is less invasive compared to direct MRA. Furthermore, it does not require fluoroscopy or a physician to perform the injection, it is easy to schedule, and is able to depict synovitis and extra-articular enhancement.
Nevertheless, labrum evaluations based on indirect MRA (enhancement of joint fluid with intravenously administered contrast medium) [14] compare poorly with direct MRA due to lack of capsular distension which can help delineate intra-articular structure such as labrum. Furthermore, indirect MRA includes a higher contrast load compared to direct MRA and necessitates at least 15 min of exercise prior to MR imaging for contrast medium uptake, causing relevant lengthening of the total scan time.
The role of 3 T MRI or 3 T MRA on the hip joint and acetabular labrum imaging is still being investigated. However, primary studies and our own data suggest that the evaluation of the acetabular labrum and cartilage will be notably improved owing to the increased signal to noise ratio (SNR) and contrast to noise ratio (CNR) [15]. Notably, Sundberg et al. reported that all surgically confirmed labral tears diagnosed by 1.5 T MRA were detected on 3 T MRI, whereas 3 T MRI also detected an additional confirmed labral tear that was missed on MRA [16]. Furthermore, 3 T MRI was superior to 1.5 T MRA in differentiating chondral lesions. Both techniques (1.5 T MRA and 3 T MRI) were superior to 1.5 T MRI.
Imaging Protocol
MRA, if indicated, consists of two steps. First, using a 20-gauge spinal needle, 10–20 mL of a 2 mM solution of Gd-DTPA2- (1.88 mg/mL, Magnevist, Schering AG, Berlin, Germany) diluted in sterile saline is injected into the hip joint by an experienced radiologist or an orthopedic surgeon under fluoroscopic guidance and strict sterile precautions. Alternatively, 10–20 mL of a 2 mM solution of Gd-DOTA– (1.88 mg/mL, Artirem, Bayer AG, Leverkusen, Germany) may be used. Iodinated contrast material is utilized to document the intra-articular position of the needle. Subsequently, the patient is transferred to the MR scanner. No exercise is performed after intra-articular contrast medium application in order to avoid discharge of the contrast medium from the hip joint.
Bilateral hip examination combined with a large field of view (FOV) may be a good screening instrument for hip and pelvic abnormalities. However, it is not useful for diagnosing labral tears and cartilage damage given the small size and narrowness of these structures. Therefore, in cases where pathology is expected to be unilateral (such as a labral tear), unilateral hip imaging should be performed and a smaller FOV should be utilized by employing a dedicated surface coil (i.e., a flexible four-channel flex coil) to keep the SNR and CNR acceptable while increasing the spatial resolution.
The subject is examined in the supine position with the pelvis at the isocenter of the magnet and the coil accurately placed on top of the hip joint to be scanned. MRI and MRA protocols that have been successfully implemented for the diagnosis of hip anomalies and joint damage [17, 18] include (1) an axial 2D turbo spin echo (TSE) sequence with T1-weighting to evaluate the femoral head–neck offset, joint capsule, and peri-articular soft tissues; (2) a high-resolution, thin-sectioned axial 2D fast low angle shot (FLASH) sequence with T1-weighting for acetabular version assessment; (3) a coronal 2D TSE sequence with PD-weighting; (4) a sagittal 2D TSE sequence with PD-weighting; and (5) a radial 2D TSE sequence with PD-weighting that is planned around the femoral neck perpendicular to the acetabular rim. Fat suppression may be used in order to reduce the chemical shift and improve the visualization of contrast material uptake.
The radial sequence is created on two planes (a sagittal-oblique and a coronal-oblique localizer image) in order to reduce saturation effects. Saturation effects, appearing as a band of low signal in the center of the acetabulum and femoral neck, are always present in 2D radial MR imaging. However, saturation does not involve the relevant capsular–labrum–cartilage complex and thus diagnostic imaging of the labrum and cartilage will be unaffected (Figs. 11.2 and 11.5).
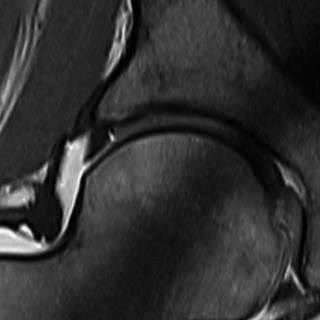
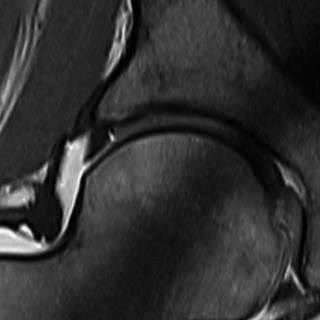
Fig. 11.5
2D PD-weighted radial image depicting a partial labral tear at the transition zone between the fibrocartilaginous labrum and the articular hyaline cartilage. This type of tear is frequently perpendicular to the articular surface and, in some cases, extends to the subchondral bone. Note the saturation effect, appearing as a band of low signal in the center of acetabulum and femoral neck, which are constantly present in 2D radial MR imaging. As saturation does not involve the relevant capsular– labrum–cartilage complex, diagnostic imaging of the labrum and cartilage will be unaffected
A TSE sequence with PD-weighting is selected due to its high spatial resolution and ability to outline cartilage and labrum tissue. The coronal and the sagittal sequences are used to visualize the labrum and the limbus. Coronal images are suitable to depict the suprafoveal articular cartilage over the femoral head, lateral dome, and superior labrum, whereas sagittal images are optimal for the assessment of the anterior labrum and cartilage (Fig. 11.6).


Fig. 11.6
PD-weighted sagittal MRA image visualizing a partial labral tear at the base of the labrum at the anterior aspect of the hip joint
Radial imaging with (MRA) and without contrast-enhancement (MRI) is a standard approach to evaluate the hip as it minimizes volume averaging by displaying the joint in perpendicular sections around the entire circumference [19–22]. Anatomy and potential abnormalities of the femur, acetabulum, and labrum are, by this means, optimally visualized in one step. Furthermore, the risk of missing etiological factors and the patho-mechanism of a labral tear and cartilage aberration, which could eventually initiate early OA, such as circumscribed osseous bump formation, may be minimized. It also provides useful information on the localization and extent of labral tears (i.e., anterior to superior-anterior), which is critical if surgical treatment is intended. Alternatively, a clock-face localization, which is consistent with arthroscopic interpretation, may be implemented, in which the 6 o’clock position depicts the acetabular notch and 3 o’clock is anterior (Fig. 11.7).
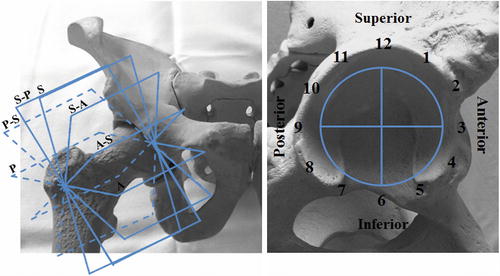
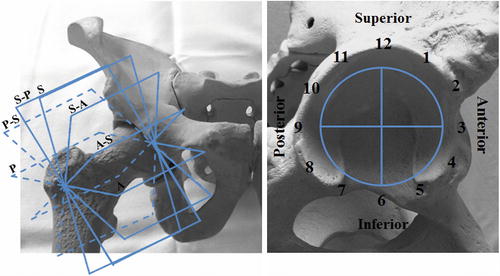
Fig. 11.7
2D or 3D radial imaging with (MRA) and without contrast-enhancement (MRI) is a standard approach to evaluate the hip because it minimizes volume averaging by displaying the joint in perpendicular sections around the entire circumference whereas anatomy and potential abnormalities of femur, acetabulum, and labrum are optimally visualized. Furthermore, it provides useful information on the localization and extent of labral tears from anterior to superior and posterior (left) that is critical if surgical treatment is intended. Alternatively, a clock-face localization (right), which is consistent with arthroscopic interpretation, may be implemented where the 6 o’clock position depicts the acetabular notch and 3 o’clock is anterior
High-resolution 3D sequences allowing for multiplanar and radial reconstructions are potential alternatives in the assessment of the hip joint. A 3D double-echo steady state (DESS) sequence with water excitation is an effective instrument in labrum and cartilage assessment, owing to its strong fluid signal that creates an arthrogram-like effect within the joint that may increase the conspicuity of the labrum and cartilage lesions, in particular if non-contrast imaging is being performed.
Further details on the imaging parameters are provided in Tables 11.1 and 11.2.
Table 11.1
MRI/MRA protocol at 1.5 T
Axial 2D TSE | Coronal 2D TSE | Sagittal 2D TSE | Axial 2D FLASH | Radial 2D TSE | |
|---|---|---|---|---|---|
TR (repetition time, ms) | 491 | 3,060 | 2,900 | 250 | 1,800 |
TE (echo time, ms) | 13 | 9.1 | 9.1 | 12 | 13 |
FA (flip angle, degree) | 150 | 150 | 150 | 90 | 180 |
NEX (number of excitation) | 2 | 3 | 3 | 2 | 2 |
FOV (field of view, mm2) | 160 | 130 | 130 | 120 |