LACRIMAL GLAND: ORBITAL PSEUDOTUMOR AND ACUTE AND CHRONIC INFECTIONS AND NONINFECTIOUS INFLAMMATORY CONDITIONS
KEY POINTS
- The imaging findings in inflammatory conditions involving the lacrimal gland are often nonspecific, but imaging can identify findings based on patterns of involvement that aid in the differential diagnosis of causative pathology in many patients.
- Imaging can identify causative conditions for infections that can lead to improved outcomes if treated promptly.
Any orbital mass or disease process may be approached by first establishing whether it is preseptal (Chapters 70 and 71) or postseptal (Chapters 57–60, 62, and 64). If postseptal, it should be established as a process arising primarily intraconally (Chapters 57–60), extraconally (Chapters 62 and 64), or transcompartmentally. If intraconal, it should be decided whether the mass is of optic nerve/sheath origin or arises from some other structure comprising or within the muscle cone. This chapter considers lacrimal gland inflammatory processes that by anatomic definition are both preseptal and postseptal and extraconal; these diseases may spread across the other orbital compartments and related spaces.
Orbital pseudotumor is the most common unilateral, noninfectious inflammatory condition that involves the lacrimal gland.1–3 Pseudotumor will most commonly involve the entire gland, eyelid, and adjacent extraconal fat (Fig. 65.1). The other noninfectious inflammatory conditions strongly tend to be bilateral, including the autoimmune Sjögren and Graves diseases (Fig. 65.2 and Chapters 20 and 58), sarcoidosis (Fig. 65.3 and Chapter 18), and Wegener granulomatosis (Fig. 65.4 and Chapter 17). The Langerhans (Chapter 19) and other histiocytoses, including Rosai-Dorfman, xanthogranulomatous disease, and Erdheim-Chester disease, may involve both or one gland. Lymphoepithelial cysts associated with HIV may be unilateral or bilateral.
Infections, like noninfectious inflammatory conditions, may be local or related to systemic disease. Most of these conditions are unilateral and viral (Fig. 65.5). Bacterial, protozoan, and parasitic infections are possible. Infection may be seen as a complication of sinonasal infection (Fig. 65.6).
The spread patterns of these inflammatory conditions are discussed in the following Pathophysiology and Patterns of Disease sections.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The relevant anatomy of the bony orbit, muscle cone, and related neurovascular structures is discussed in detail in Chapter 44. In particular, the anatomy of the palpebral and orbital portions of the lacrimal gland and the gland’s relationship to the orbital septum should be reviewed. It might also prove useful to review the related anatomy of the lacrimal drainage system.
IMAGING APPROACH
Techniques and Relevant Aspects
The orbit, eye, and optic nerve and sheath are studied with computed tomography (CT) and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. Specific CT protocols by indications are detailed in Appendix A. Specific MR protocols by indications are outlined in Appendix B. Almost all studies to investigate the lacrimal gland inflammatory pathology are done with contrast.
Pros and Cons
Disease of the lacrimal gland is studied primarily with CT and magnetic resonance imaging (MRI). MRI is far more definitive in its rendering of the gland. MRI is also far more sensitive than CT to possibly related meningeal pathology.
CT is typically used in acute situations when an aggressive infectious process is possible. It is also a first choice in patients too sick or for some other reason unable to complete a very high quality, free of motion artifact, MRI examination.
Either study is sufficient for a good evaluation of the lacrimal gland. Supplemental CT may need to be done if bone involvement or related sinonasal pathology needs to be evaluated definitively.
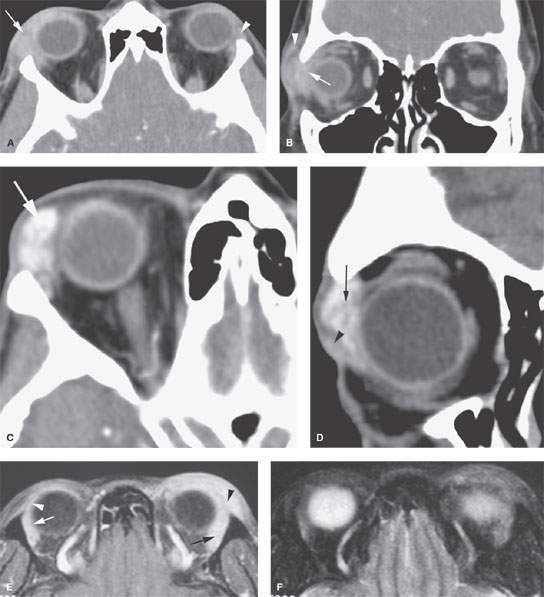
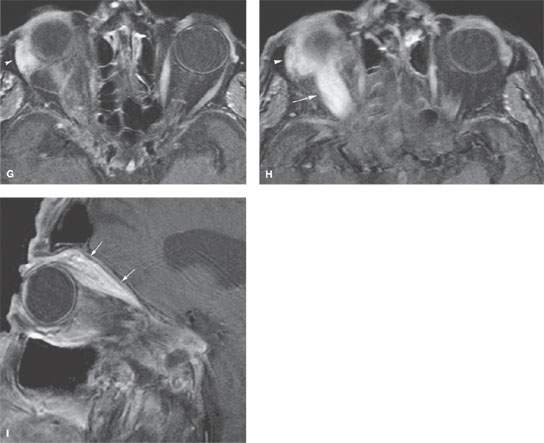
FIGURE 65.1. Four patients with orbital pseudotumor. A, B: The first patient with orbital pseudotumor. In (A), contrast-enhanced computed tomography shows an enlarged right lacrimal gland (arrow). Its margins are indistinct. The left lacrimal gland (arrowhead) is normal. In (B), a coronal section of the patient seen in (A) shows the enlargement and indistinctness of the right lacrimal gland region (arrow) that also extends into the preseptal soft tissues (arrowhead). C, D: A second patient with orbital pseudotumor. In (C), there is an unusual amount of contrast enhancement (arrow) of the emerged gland. In (D), the coronal section of this case shows the patchy enhancement of the abnormal lacrimal gland (arrow) and abnormal enhancing tissue surrounding the gland (arrowhead). E, F: Magnetic resonance imaging study of a third patient with orbital pseudotumor. In (E), the contrast-enhanced T1-weighted (T1W) fat-suppressed image shows marked enlargement of the lacrimal gland (arrow) and spread of inflammatory tissue into the preseptal soft tissues (arrowhead). Contrast that appearance with the normal lacrimal gland (white arrow) orbital portion and palpebral portion (arrowhead) on the opposite side. In (F), a T2-weighted image to compare with that in figure (E) shows diffusely abnormally increased signal in the areas involved with pseudotumor. G–I: In the fourth patient, axial and sagittal contrast-enhanced T1W fat-suppressed images show thickening and enhancement of the right lacrimal gland (arrowhead) and superior rectus/ levator palpebrae complex (arrow).
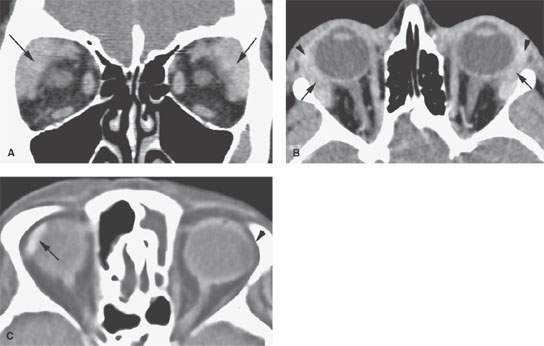
FIGURE 65.2. Two patients with autoimmune lacrimal gland disease due to Sjögren disease. A: Coronal contrast-enhanced computed tomography study shows enlargement of both lacrimal glands. Their margins are fairly well circumscribed. B: Axial section of the patient seen in (A) shows that on both sides, the orbital portion of the gland (arrows) and the palpebral portions of the gland (arrowhead) are enlarged but fairly well circumscribed. C: A second patient with long-standing Sjögren disease. The right lacrimal gland is atrophic and calcified (arrow). The left is so atrophic that it cannot be seen as an end-stage effect.
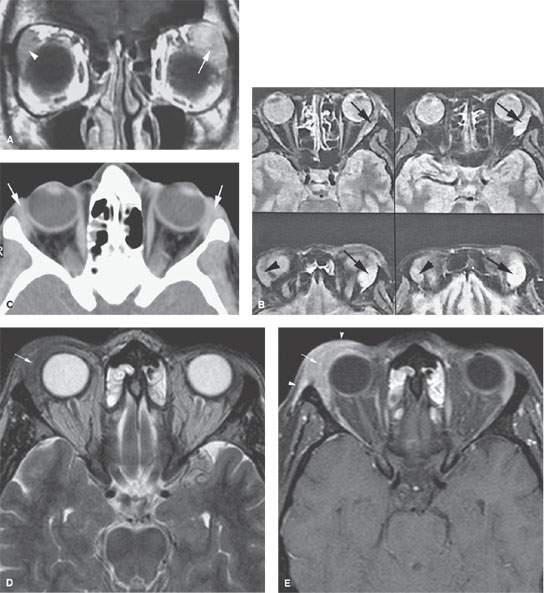
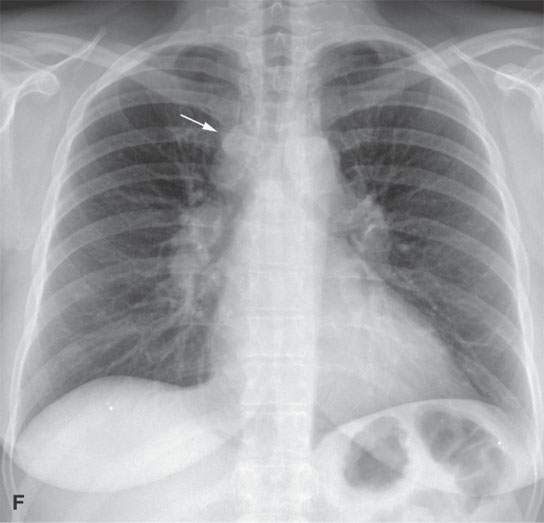
FIGURE 65.3. Three patients with sarcoidosis. A, B: In the first patient, contrast-enhanced T1-weighted (T1W) image shows a markedly enlarged and abnormally enhancing lacrimal gland seen on the left (arrow) compared to the slightly enlarged gland on the right (arrowhead). A series of density-weighted images show the disease as present bilaterally (B) but markedly more on the left (arrows) than the right (arrowhead). C: A second patient with multisystem involvement with sarcoidosis. This computed tomography shows bilateral slight enlargement of both lacrimal glands (arrows). D, E: The third patient presented with a swelling under the right eyelid. On T2-weighted and contrast-enhanced T1W fat-suppressed images, swelling and enhancement of the right lacrimal gland (arrow) is seen with involvement of the preseptal soft tissues (arrowheads). A biopsy was taken that revealed granulomatous inflammation. F: On chest x-ray, paratracheal (arrow) and hilar lymphadenopathy is present, which is consistent with sarcoidosis.
SPECIFIC DISEASE/CONDITION
Orbital Pseudotumor/Idiopathic Orbital Inflammatory Syndrome and Noninfectious Inflammatory Disease
Etiology
Idiopathic orbital inflammatory syndrome (IOIS) is an acquired immune-based process that lacks systemic involvement.
Other noninfectious inflammatory diseases may also be local or related to systemic disease. The etiology of autoimmune processes that may involve the lacrimal glands, including Graves dysthyroid orbitopathy and Sjögren disease, and their manifestations in other organ systems is discussed in Chapter 20 in general; Graves is discussed in Chapter 58. Sarcoidosis (Chapter 18) and Wegener granulomatosis (Chapter 17) are the granulomatoses that may involve the gland. Langerhans (Chapter 19) and other histiocytoses, including Rosai-Dorfman, xanthogranulomatous disease, and Erdheim-Chester disease, may involve both or one gland. The etiology of all these diseases is not well understood. They all likely represent some type of aberrant immune response. Lymphoepithelial cysts are associated with HIV infection.
Prevalence and Epidemiology
IOIS is a sporadic disease with no known predisposing factors. Although not as common as thyroid ophthalmopathy, it is one of the more frequent causes of orbital disease and is diagnosed in approximately 5% of these cases.
The prevalence and etiology of the granulomatoses and autoimmune diseases that affect the lacrimal gland are discussed in the chapters on those entities as noted in the previous section.
Clinical Presentation
Pseudotumor almost always presents as a unilateral swollen and painful orbital mass, most typically in the upper outer quadrant when it is of primarily lacrimal origin. It may present acutely, in which case there is greater pain and redness, or it may present more chronically, in which case there may only be a painless superior temporal mass variably associated with fixation of the globe and/or its muscles. It is occasionally bilateral. The other noninfectious inflammatory diseases are more likely bilateral than pseudotumor and the degree of pain and swelling in the lacrimal gland region less. All disease may have associated conjunctivitis and a discharge. The eye may be displaced inferior and medially.
Pathophysiology and Patterns of Disease
Although IOIS has several morphologic forms, its pathologic basis remains the same; only its distribution varies. These include the episcleral (or anterior orbital), myositic, perineuritic, diffuse, and dacryocystic forms. The actual distribution of the disease frequently spills over from one of these predominant sites of involvement to other areas. The pathophysiology of this disease has been discussed in Chapters 57 and 62. When arising in the lacrimal gland, it will cause the gland to swell with associated periglandular inflammatory changes (Chapter 13).
The granulomatoses often involve the orbit secondarily. Wegener granulomatosis is often seen as a result of spread from the sinonasal region. However, orbital disease without paranasal involvement or bilateral lacrimal gland swelling may be present in Wegener granulomatosis (Fig. 65.4). Sinonasal sarcoidosis is uncommon but may be associated with orbital involvement.4 In sarcoidosis, involvement of the lacrimal gland may be bilateral (Fig. 65.4) and may precede systemic disease.
Langerhans cell histiocytosis (LCH) may involve the orbit in children and rarely in young adults, most often as a bony lesion with secondary extraconal or transcompartmental orbital extension. The disease may permeate the orbital soft tissues; thus, it might only secondarily involve the lacrimal gland. In children, LCH is most commonly centered on the area of the lacrimal fossa (frontal bone). In adults, LCH lesions are located more posteriorly on the greater wing of the sphenoid bone, where there is still active bone marrow.5 Bilateral or unilateral involvement of the lacrimal glands may occur in LCH and the more rare histiocytic diseases. These other rare, infiltrating processes can mimic IOIS and the granulomatoses and histiocytoses. These include predominantly dermatologic diseases, such as Erdheim-Chester disease in adults and juvenile xanthogranulomatosis in children, that may secondarily involve the orbit and in particular the lacrimal glands. Necrobiotic xanthogranuloma, pseudorheumatoid nodules, amyloidosis, panniculitis, and other disease states must be distinguished on clinical grounds or by biopsy.
Manifestations and Findings
Computed Tomography and Magnetic Resonance Imaging
The general morphology of inflammatory disease as seen on CT and MRI is described in Chapter 13 and other diseases in this category in chapters as indicated earlier in this section.
On CT and MRI, this inflammatory morphology appears as an indistinct, contrast-enhancing, and infiltrating process involving the orbital fat, sclera, extraocular muscles, lacrimal gland, optic nerve, or some combination of these structures. There is frequently nonenhancing edema in adjacent fat and of the preseptal soft tissues (Figs. 65.1–65.6).
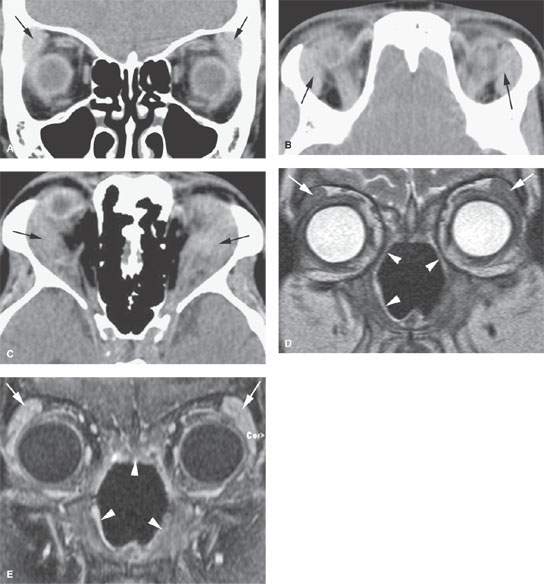
FIGURE 65.4. Three patients with Wegener granulomatosis (WG). A, B: Bilateral, symmetric enlargement of the lacrimal gland (arrows) with a slight degree of indistinctness of their margins. C: A second patient with WG and marked enlargement of the lacrimal glands with spread of disease well beyond the gland capsules within the orbit (arrows). D, E: A third patient with the excavating enhancing changes of WG involving the nasal cavity (arrowheads) and bilateral lacrimal gland involvement (arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








