LARYNX: INFECTIOUS AND NONINFECTIOUS INFLAMMATORY DISEASES
KEY POINTS
- Imaging is occasionally useful in the management of epiglottitis, supraglottitis, and other acute pyogenic laryngeal infections.
- Computed tomography can provide a safe and rapid assessment of the airway in a patient who is stable, under the control of the treating physician for airway management decisions, and in whom one wishes to avoid endoscopy.
- Imaging in inflammatory diseases, except in relapsing polychondritis, is generally nonspecific for diagnostic purposes.
- Atypical clinical and imaging features of laryngeal pathology should raise the possibility of an inflammatory process.
A variety of infectious and noninfectious inflammatory disorders may affect the larynx. The vast majority never come to imaging. Many that do really do not require imaging, but the imaging study is obtained because the etiology of the disease is uncertain and it is thought that imaging might help with the diagnostic process (Figs. 204.1–204.3). This typically occurs in diseases that may mimic cancer, and several diseases in this category are fully capable of that masquerade. Others come to imaging for a noninvasive assessment of the static airway dimensions when it is felt that this might be less risky and/or sufficient to decide on the proper course of airway management.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
A thorough knowledge of laryngeal anatomy and anatomic variations in each of the following areas is required for the evaluation of laryngeal inflammatory diseases. This anatomy is presented in detail with the introductory material on the larynx, hypopharynx, cervical esophagus, and infrahyoid neck in general.
Evaluation of laryngeal and related structures frequently involved with contiguous disease in these conditions should include the following:
- Larynx, including the laryngeal skeleton, deep tissue spaces within the larynx, mucosal landmarks, and functional structures within the larynx (Chapter 201)
- Hypopharynx (Chapter 215)
- Tongue base region and low oropharyngeal wall (Chapter 190)
- Cervical esophagus and its junction with the postcricoid portion of the hypopharynx (Chapter 221)
- Trachea (Chapter 209)
Evaluation of Extralaryngeal Spread
- Visceral compartment of the neck and related fasciae (Chapter 149)
Evaluation of Regional Lymph Node Disease
- Detailed knowledge of normal node and perinodal morphology and the common drainage pathways of laryngeal disease, which emphasizes nodal levels 2 through 6 (Chapters 149 and 159)
Evaluation of Perivascular and Perineural Spread
- Knowledge of the entire course of the vagus and recurrent laryngeal nerves on both sides and of the superior laryngeal neurovascular bundle (Chapter 201)
IMAGING APPROACH
Techniques and Relevant Aspects
The neck should always be slightly hyperextended for laryngeal computed tomography (CT). This pulls the larynx higher in the neck, thus reducing artifacts produced by the shoulders.
It is often less critical to view images parallel to the true vocal cords for medical decision making in inflammatory laryngeal conditions than with tumors or in cases of trauma. This is mainly because these frequently are medical diseases that will not require precise anatomic delineation for planning surgery or deciding between surgery and radiotherapy as treatment options. However, a primary goal of data acquisition and viewing in any laryngeal study should be that images should lead to optimal medical decision making. To allow for this detail, specific protocols appear in Appendix A.
When viewed on a workstation, such data sets provided by an optimized protocol allow off-axis reformations to correct for skewed acquisitions relative to the plane of the true vocal cords as well as coronal and sagittal images orthogonal to the axial plane of the true cords. Viewing tools also allow for virtual endoscopic images that can help to avoid some endoscopic and bronchoscopy procedures for at least gross airway assessment, even though these virtual, usually static, images lack dynamic and functional information.
Intravenous contrast is usually used for all studies of laryngeal inflammatory disease unless there is a very compelling reason not to use contrast or if the studies are being done to only evaluate the airway lumen. Many conditions will enhance, improving the lesion-to-muscle contrast. If iodinated contrast is necessary and cannot be used, then magnetic resonance imaging (MRI) should be considered as the primary study.
Magnetic resonance (MR) studies should be done with receiver coils that are custom designed to study the neck. Small loop or posteriorly placed surface coils meant to study the spine are not adequate. The use of intravenous paramagnetic contrast is individualized, but generally it is used. Specific protocols are presented in Appendix B.

FIGURE 204.1. A patient presenting with hoarseness and some dyspnea on exertion. A contrast-enhanced computed tomography study was done. In (A) and (B), there is an enhancing mass surrounding the region of the arytenoid cartilage and cricoarytenoid joint and eroding the top of the thyroid cartilage. The lesion shows more generalized surrounding soft tissue swelling than most cancers. It also appears somewhat atypical clinically. The patient was started on antibiotics, and a follow-up study in (C) and (D) shows resolution of most of the enhancement and mass with a sequestrum (arrow in D). The final diagnosis was laryngeal syphilis.
Pros and Cons
Evaluation of Disease of Uncertain Etiology
Inflammatory disease limited to the larynx may mimic the initial presentation of laryngeal cancer (Figs. 204.1–204.3). Any condition, regardless of etiology, that is suspicious for deep infiltration or cancer should be studied primarily with CT if imaging is desired as part of the evaluation. MRI is rarely indicated in inflammatory conditions of the larynx since a significant proportion of MR studies will be of poor quality owing to motion artifacts, and such studies will add limited additional information that might alter medical decision making, especially with regard to the laryngeal skeleton (Fig. 204.4). Supplemental MR study, in the uncommon situation where it might add meaningful incremental data, is best directed by CT findings to a localized area of interest where its strengths related to better soft tissue contrast resolution may be exploited.
Any imaging study of the larynx for a disease condition must be evaluated for its effect on the airway; the extent of the endolaryngeal spread; cartilage involvement or origin; spread to adjacent structures including the hypopharynx, tongue base, trachea, and esophagus; and extralaryngeal spread to the soft tissues of the neck. The evaluation must also include a search for regional adenopathy and spread along neurovascular bundles at risk. There are several areas where CT or MR images consistently provide better information than the endoscopic examination. These include the subglottis, paraglottic space, pre-epiglottic space, tongue base (possibly involved via the pre-epiglottic space), and the laryngeal cartilage.
Integrity of the Airway
Any imaging study of the larynx for a disease condition must be evaluated for its effect on the airway (Fig. 204.5). This is frequently the initial and main indication in the case of infectious and noninfectious inflammatory conditions, with the etiology being known or at least highly suspected. The anatomic status of the airway, as well as the risk of any acute adverse complication such as the potential for rapidly progressive airway obstruction, should be reported.

FIGURE 204.2. Two patients with laryngeal tuberculosis. Contrast-enhanced computed tomography studies were done in both patients because of a clinical suspicion of cancer. A, B: Patient 1 showing an enhancing mass along the aryepiglottic fold and epiglottis (arrows). The abnormality is indistinguishable from cancer, and the diagnosis was only made by biopsy and histologic examination. C, D: In Patient 2, the findings due to tuberculosis more involve the vallecula, epiglottis, and upper aryepiglottic folds (arrows). In (D), the symmetric thickening and infiltration of the aryepiglottic folds (arrows) is atypical of cancer and suggests a possible inflammatory etiology. However, based on these imaging findings, carcinoma cannot be ruled out with certainty.
Evaluation of Laryngeal Dysfunction Due to Submucosal Masses
Some patients have processes predominantly occurring beneath intact mucosa. These diseases may also begin on the mucosa within the laryngeal ventricle and spread within the paraglottic space, or may primarily arise from the laryngeal cartilages (Figs. 204.4 and 204.5D–F). About half of all submucosal laryngeal masses will be laryngoceles that may present due to a complicating purulent infection that cannot be simply distinguished on a clinical basis from other inflammatory disease of the larynx (Fig. 204.6). This is discussed more fully in conjunction with laryngoceles (Chapter 203).
Vocal Cord Dysfunction and Weakness
An inflammatory process can affect the cricoarytenoid joint (Figs. 204.4 and 204.5D–F). CT can be useful in showing such an involvement as a cause for true vocal cord dysfunction.

FIGURE 204.3. Contrast-enhanced computed tomography of an infiltrating laryngeal mass due to sarcoidosis (arrows) that is indistinguishable from cancer (A–C) with cricoid cartilage erosion (arrowhead in D). The clue to the diagnosis was the hilar and mediastinal adenopathy (not shown). It is very unusual to have laryngeal sarcoid as an isolated manifestation or presenting disease locale.

FIGURE 204.4. A patient who had a chronic burn injury to the upper airway resulting in dysphagia and chronic hoarseness without an obvious mucosal lesion. The contrast-enhanced computed tomography in (A) shows enhancing tissue (arrows) surrounding lower-density, likely necrotic, tissue (arrowhead). A coronal reformatted image (B) shows the eroded cricoarytenoid joint (arrow).

FIGURE 204.5. Two patients presenting with airway obstruction and neck tenderness. Computed tomography studies with contrast were done in both. A–C: Patient 1 with acute upper airway symptoms, fever, and throat pain. The study shows extensive edema in the vallecula and supraglottic larynx extending down to the aryepiglottic folds. This was proven to be due to supraglottis due to Hemophilus influenzae infection. D–F: Patient 2 had a more subacute presentation, and the prior history of attempted intubation was not available. There is extensive edema involving the right true vocal cord and right subglottic region as well as the soft tissues adjacent to the larynx. There is also erosion of the upper margin and body and right side of the cricoid cartilage. These changes were due to infectious chondritis following traumatic intubation.

FIGURE 204.6. A patient presenting with upper airway symptoms and hoarseness. The patient was febrile and also had some slight throat pain. Clinically, the patient was believed to possibly have laryngeal cancer. In (A) and (B), a fluid attenuation process can be seen in the right paraglottic space with an appearance suggesting that it is arising within an internal laryngocele, possibly perforating (arrow) into the pharynx. The extension inferiorly to the false cord level in the paraglottic space is seen in (B) as well as its extension to the pharynx. Surgery confirmed the imaging suggestion that this was a laryngopyocele that perforated into the adjacent pharynx.
Controversies
Some believe that MRI should be the primary study for evaluating the larynx in most conditions. This is discussed in more detail in the introductory material about the larynx (Chapter 201).
SPECIFIC DISEASE/CONDITION
Acute Pyogenic Bacterial Infections Including Epiglottitis/Supraglottitis
Etiology
Epiglottitis, also known as supraglottitis since it involves not only the epiglottis but may also diffuse to involve the entire supraglottis, including the aryepiglottic fold, critically narrows the airway at the level of the laryngeal vestibule (Figs. 204.5A–C and 204.7). It is caused by Hemophilus influenzae type B in 90% of cases.
The effects of acute bacterial laryngopyocele (Fig. 204.6 and Chapter 203), spread of an acute suppurative deep neck or pharyngeal infection to the larynx (Chapters 155 and 217), and pyogenic infection related to penetrating or blunt trauma or retained foreign bodies (Chapters 207 and 220) are discussed more fully elsewhere.
Prevalence and Epidemiology
Epiglottitis/supraglottitis is predominantly a disease of 3 to 5 year olds. In adults, it is more commonly referred to as adult supraglottitis and tends to be less immediately life threatening, perhaps because the airway is larger or perhaps related to the ability to mount an immunologic response.
Clinical Presentation
Epiglottitis/supraglottitis and other laryngeal pyogenic infections will present with fever, upper airway obstruction, and hoarseness. It can rapidly progress to life-threatening airway obstruction.
Pathophysiology and Patterns of Disease
Epiglottitis/supraglottitis causes severe mucosal disease in the supraglottis with secondary edema that spreads freely within the loose spaces of the supraglottis. Those deep spaces are relatively tight at the true cord level, so the vocal cords are relatively less affected. Rarely, an epiglottic abscess develops in adult patients (Fig. 204.8); formation of an epiglottic abscess is much rarer in children.
The pathophysiology of other acute bacterial infections including laryngopyocele (Chapter 203), spread of an acute suppurative deep neck or pharyngeal infection to the larynx (Chapters 155 and 217), and pyogenic infection related to penetrating or blunt trauma or retained foreign bodies (Chapters 207 and 220) are discussed more fully elsewhere.
Manifestations and Findings
Plain Film
No imaging study should be performed until an expert at managing the airway is supervising the patient and directing care.
Plain films may be used to screen for epiglottitis/supraglottitis, especially if there is not a very skilled examiner available who can take immediate charge of establishing the airway if lost during the examination.
Plain films will show thickening of the suprahyoid epiglottis and aryepiglottic folds and posterior pharyngeal wall down to the true vocal cord level. The airway at the laryngeal vestibule level will be narrowed.
Computed Tomography
No imaging study should be performed until an expert at managing the airway is supervising the patient and directing care.
If CT is done for epiglottitis/supraglottitis, it will show diffuse edema and marked swelling from the vallecula to just above the true cords (Figs. 204.5A–C and 204.7). If contrast is given, there will be relatively avid, diffuse enhancement in an untreated patient. Rarely, an epiglottic abscess will be visible (Fig. 204.8).

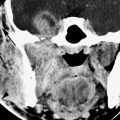
FIGURE 204.7. An adult patient presenting with throat pain and mild upper airway symptoms due to bacterial supraglottitis. A contrast-enhanced computed tomography study shows extensive swelling (A, B) of the aryepiglottic folds, the arytenoids pad, and the false cords.
Magnetic Resonance
In the rare event that MRI is done for epiglottitis/supraglottitis, it will show diffuse edema and marked swelling from the vallecula to just above the true cords. If contrast is given, there will be relatively avid, diffuse enhancement in an untreated patient.
Endoscopy
Endoscopy may be used to confirm or rule out epiglottitis/supraglottitis but must only be done by a very skilled examiner who can take immediate charge of establishing the airway if it is lost during the examination.
Differential Diagnosis
From Clinical Data
Differentiation is primarily from other upper respiratory infections on the basis of the clinical situation and sometimes imaging.


FIGURE 204.8. Two patients with supraglottitis complicated by abscess formation. Contrast-enhanced computed tomography (CECT) studies were done. A: Patient 1. An adult with progressive throat pain, dysphagia, and dyspnea. The study showed an epiglottic abscess (arrowheads). B–H: Patient 2. In (B) through (D), there is extensive edema along the pharyngeal wall and supraglottic larynx on the right but no definitely drainable fluid collection. This was considered consistent with severe supraglottitis. A repeat CECT study done 3 days later because the patient was still symptomatic shows that the pharyngeal and laryngeal infection had matured to a drainable collection of purulent material (arrows) extending along the paraglottic space. In (H), communication with the saccule is likely present (arrowhead).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree