LATERAL COMPARTMENT: NONNODAL INFECTIOUS AND INFLAMMATORY CONDITIONS
KEY POINTS
- Magnetic resonance imaging and computed tomography provide the critical and usually definitive data needed in the diagnosis and management of lateral compartment inflammatory and infectious diseases.
- Prompt and accurate imaging can help to avoid potentially severe airway and vascular complications and/or spread to the mediastinum.
- Imaging-guided aspiration and/or tissue sampling may be used to assist in the management of these infections.
INTRODUCTION
Nonnodal infection and inflammatory conditions of the lateral compartment discussed in this chapter include principally deep neck abscesses and conditions that mimic deep neck infection. The latter are predominantly infected developmental cysts of the branchial apparatus (Chapter 153), thrombophlebitis, arteritis, or occasionally a complication arising in a venolymphatic malformation (Chapter 154). The pathophysiology of these changes in the latter three conditions are discussed more generally in Chapters 9, 10, 13, 15, and 16. Thyroid pathology that may present in this manner is discussed in Chapter 173.
Clinical Presentation
The clinical presentations generally fall into one of several categories of neck masses, including the following:
- Acute febrile illness with a tender swollen neck likely due to either pyogenic lymphadenitis, a deep neck abscess, or an infected cyst
- Tender neck mass possibly due to a low-grade or chronic inflammatory process
- Penetrating trauma
- Surgical complication
APPLIED ANATOMY
The anatomy of the lateral compartment is essentially that of the carotid sheath and its relationship to the anterior and posterior triangles. The relationship to the retropharyngeal space medially and the thoracic inlet and suprahyoid neck space must be understood. Essentially, there is relatively free communication within the lateral compartment between the anterior and posterior triangles and the retropharyngeal space. The relationship of those spaces to the superficial fascia (platysma) and investing and prevertebral layers of the cervical fascia should be reviewed, if necessary, in Chapter 149.
Structures of Interest
The analysis of infectious conditions of the lateral compartment depends on an understanding of their possible origin from nodes or infected developmental cysts and how the infectious or otherwise inflammatory conditions might relate primarily or secondarily to the carotid sheath vessels and to the following anatomic boundaries:
- Superiorly: Hyoid bone as the arbitrary boundary
- Inferiorly: Thoracic inlet and supraclavicular fossa
- Anteriorly: Anterior triangle
- Posteriorly: Posterior triangle
- Medially: Retropharyngeal space
- Laterally: Sternocleidomastoid muscle
IMAGING APPROACH
Computed Tomography and Magnetic Resonance Imaging
The infrahyoid neck is mainly evaluated with computed tomography (CT) and magnetic resonance imaging (MRI). The specifics and relative value of using these studies in this anatomic region are reviewed in Chapter 149. Problem-driven protocols for CT and MRI are presented in Appendixes A and B. In general, CT is more definitive than MRI for efficient evaluation of inflammatory conditions of the lateral compartment and related carotid sheath vessels.
Other
Ultrasound has a potential limited triage role to play in the evaluation of an inflammatory process of nonthyroidal origin. It can be used to screen for vascular complications. It is most often cost additive and unlikely to consistently contribute to definitive medical decision making. It may actually delay a more timely use of a likely more definitive CT or magnetic resonance (MR) study.
Catheter angiography is use very selectively and most often as a prelude to endovascular intervention once the diagnosis of a vascular complication has been established by computed tomographic angiography or MR angiography.
PATHOPHYSIOLOGY AND PATTERNS OF DISEASE AND DIFFERENTIAL DIAGNOSIS AS SEEN ON MAGNETIC RESONANCE IMAGING AND COMPUTED TOMOGRAPHY
The pathophysiology and related imaging appearance of acute and chronic inflammation and infection is discussed in Chapters 13 and 16, respectively, and that of their vascular complications in is discussed in Chapter 15.
Differential Diagnosis
The initial evaluation of a disease process in the lateral compartment must determine whether the lateral compartment is only secondarily involved. Frequently, the infection in the lateral compartment is spreading from more cephalad sources, such as pharyngeal and dental infections. Most of the time, the source declares itself by its clinical circumstances, but sometimes the infection is so rapidly progressive or widespread at the time of presentation that only imaging provides definitive clues as to the source of infection.
Infectious disease occasionally begins in the lateral compartment from ruptured suppurative adenitis (Chapter 158), an infected branchial apparatus cyst (Chapter 153), postoperatively, or in a penetrating or perforating type of injury. The lateral compartment may be secondarily involved by inflammation beginning in the visceral compartment or retropharyngeal space (RS) (Chapter 151) and rarely in the posterior compartment (Chapter 160).
Lateral compartment edema and/or cellulitis may be generated by thrombophlebitis of the jugular venous system (Chapter 154) or carotid arteritis (Chapter 154) or may produce those conditions as a secondary effect of lateral compartment infection.
The basic pathophysiology of most of these conditions is discussed in Chapters 9, 10, 13, 15, and 16. Their appearance is also shown and discussed in the following figures and chapters in this section on the neck:
- Necrotizing fasciitis and other rapidly spreading infection, the morphology of which may vary considerably depending on the specific organism and immune status or comorbidities of the patients (Figs. 155.1–155.3)
- Jugular thrombosis and thrombophlebitis (Fig. 155.4 and Chapter 154)
- Perforated suppurative lymphadenitis, carotid arteritis, and related complications (Figs. 155.5 and 155.6 and Chapter 159)
- Iatrogenic and noniatrogenic trauma, such as abscess, infected hematoma, and lymphocele (Fig. 155.7 and Chapter 154)
- Infected or inflamed congenital cysts and venolymphatic malformations (Fig. 155.8 and Chapters 153 and 154)
- Other conditions that might arise from the visceral or posterior compartments (Fig. 155.8 and Chapters 151 and 160)
Aspiration
These infections may be sampled by using imaging guidance. Such tissue sampling can be part of the medical decision-making process if aspiration of an infected space or disc will contribute to care.
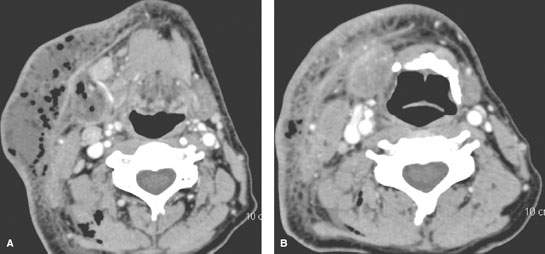

FIGURE 155.1. Contrast-enhanced computed tomography (CT) study of soft tissue windows showing a patient with severe necrotizing fasciitis in (A) and (B). Gas and necrotic, purulent material is spread in all compartments, respecting no tissue boundaries. The cause of this severe infection was shown on bone window CT to be from periapical disease dental (arrow in C). (continued)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








