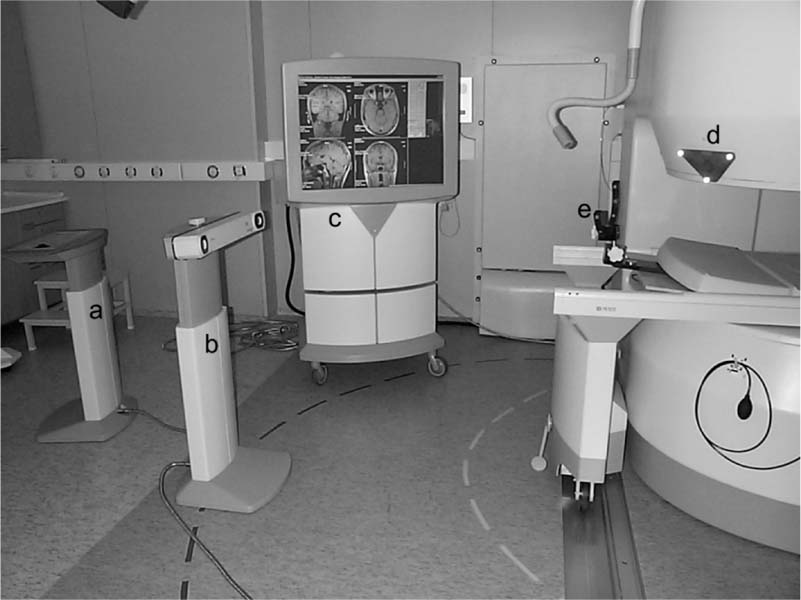
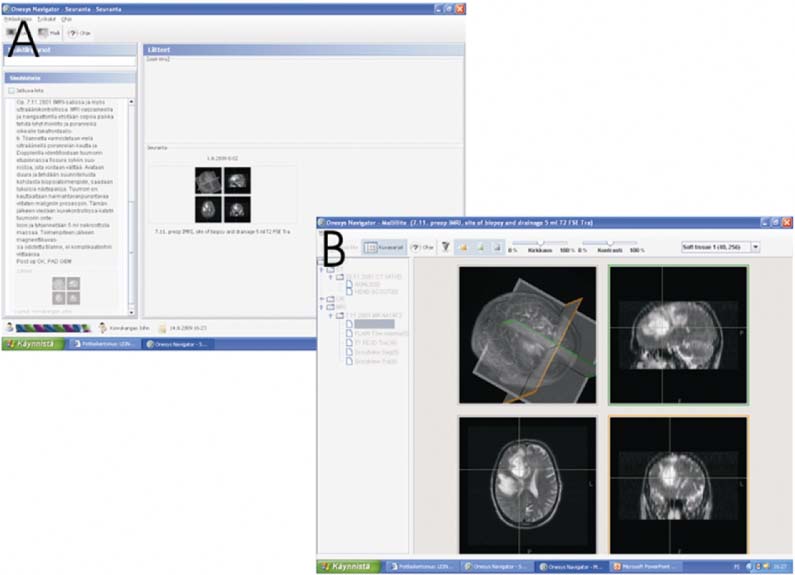
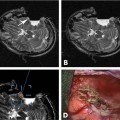
7 Low-field MRI scanners are well suited for brain biopsies because of the short distance from the edge of the magnet to the isocenter and the relatively minor susceptibility artifacts. High-field imaging data obtained routinely in the course of diagnostic imaging preoperatively can be fused to low-field intraoperative images if needed. There are only a few patient series published on brain biopsies performed using low-field imagers. Tronnier et al1 reported on a series of 60 patients biopsied using a 0.2 tesla (T) imager as early as 1999. However, most of the publications on experiences at low-field strength contain relatively few biopsy cases. Lewin et al2 included only three biopsies in a series of 130 operations using a 0.2 T scanner. Kanner et al3 had 15 biopsy cases in their series of 70 neurosurgical procedures performed using the 0.12 T imaging system. Using the 0.12 T scanner, Schulder et al4 reported only three biopsies out of 93 operations. Indeed, for some of the pioneering centers, the goal of application of intraoperative magnetic resonance imaging (iMRI) has been to improve tumor resection results, with no biopsies being performed.5 The low number of brain biopsies may reflect treatment practices preferring tumor resection over biopsy in many centers using low-field MRI. Although in some centers a “watch and wait” approach favors diagnostic biopsy over more risky tumor resection, the tendency in other centers prefers removing as much tumor as possible while obtaining a histologic diagnosis. Advocates of the latter approach stress delaying future neurologic compromise due to the mass effect of the growing tumor as well as the delay of the malignant transformation of low-grade tumors and reduction of tumor burden for adjuvant therapy of high-grade tumors. Some studies indicate that biopsy may cause morbidity comparable to that of resection, which speaks for the latter approach.6 This chapter is based on our experience in Oulu, Finland: (1) since 1996 with one of the first iMRI concepts in the world7 – the application of a new commercially successful Finnish low-field MRI scanner (at the time, Picker Nordstar Oy, Vantaa, Finland, but later acquired by Philips Healthcare,Andover, MA), (2) pioneering experience since 1981 with real-time intraoperative ultrasound imaging (iUS),8 and (3) since 1990 with neuronavigation.9,10 Most of the low-field systems originally offered by vendors, with the notable exception of the 0.15 T scanner (PoleStar-N20, Medtronic Navigation, Louisville, CO), have since been replaced by high-field ones. However, the lessons learned in all of the early centers need to be brought over to the newer systems. One of the important aspects of the Oulu experience has been the feasibility of formally sharing the scanner with other specialties, including radiology, pediatric surgery, and ear, nose and throat surgery. Another important aspect has been the realization that iMRI, and other intraoperative technology, is complicated: the full realization of its potential will continue to require dedicated technical and scientific collaboration at leading development centers. The Oulu low-field iMRI concept was based on a single room concept featuring a commercially successful low-field scanner that could be turned off and on again within minutes (Fig. 7.1). This scanner was originally developed over a 20-year period at Picker-Nordstar Oy, Vantaa, Finland (acquired by Philips). The patient was operated on in the scanner or more commonly adjacent to it. When operating outside of the scanner, the magnetic field could be turned off, and all regular instruments and devices could be used next to the scanner. The ramp-up time for the scanner was 6 minutes. Together with the vendor, we developed the entire suite, including an optical neuronavigator system complete with custom-made visualization software. Because it was an early concept, all aspects of the operating room had to be modified for the new concept of having an MRI scanner in the operating room. Also, the idea of sharing the room with other specialties, and especially with outpatient radiologic imaging was a departure from the usual neurosurgical suite setting.11 Fig. 7.1 The Oulu single-room intraoperative magnetic resonance imaging (iMRI) suite. (A) In-room MRI scanner control panel. (B) Polaris optical neuronavigator camera. (C) Large movable image display. It is important for the neurosurgeon to meticulously plan each procedure. The patient also needs to be well informed as to the purpose and nature of the procedure. For over 10 years, we have routinely informed our patients about iMRI procedures using preoperative neuronavigation either in the patient examination room on the ward or in the actual iMRI suite. The patient education session facilitates preoperative workup, in which the patient has recently been imaged; these images are used with a neuronavigator to not only plan the operation hands on, but to show the patient and significant others what the operation will actually look like. Because our clinic was one of the early developers of neuronavigation, several of these expensive and sensitive systems were available. For biopsies, patients were routinely imaged with MRI on the day before surgery, with fiduciary markers (i.e., fiducials) or other markings. We simply took one of our neuronavigators into the patient examination room, fixed the patient’s head with a ring cushion, and performed a navigation exercise, including registration of the device to the skin fiducials on the patient’s head. At first, we were apprehensive about whether or not the patient was interested in following the procedure on the navigation display. As it seemed to lessen anxiety, and certainly served to inform the patient about the upcoming surgery, it soon became a routine part of workup of all of our iMRI patients. Since 2002, the patient education session has been performed on the day before surgery in conjunction with the preoperative MRI study in the actual iMRI scanner.12 The patient information and planning session forms the first part of the overall documentation of the iMRI procedure using the Onesys Navigator software program to be reported elsewhere (Fig. 7.2). This is a novel graphical user interface, integrated to the electronic medical record. It allows us to condense all of the essential information and images related to any procedure onto one single workspace with links to the pertinent images on various hospital databases, including the Picture Archiving and Communication System (PACS). On this unique workspace the preoperative, intraoperative, and postoperative information can be collected for later quick retrieval. The workspace also serves prospective follow-up studies, with scientific information being an integral part of the Hospital Information System (HIS) and not standalone documentation. Fig. 7.2 The Onesys Navigator workspace. (A)
Low-Field Brain Biopsy
The Oulu Low-Field iMRI Concept and Experiences
The Low-Field iMRI Suite
Preoperative Workup
Biopsy Documentation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree