, Mark J. Jameson2, Max Wintermark3 and Prashant Raghavan4
(1)
Division of Neuroradiology, Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(2)
Division of Head and Neck Surgical Oncology, Department of Otolaryngology – Head and Neck Surgery, University of Virginia Health System, Charlottesville, VA, USA
(3)
Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(4)
Division of Neuroradiology, Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
Abstract
While there are a variety of causes of cervical lymphadenopathy (see Box 2.1), the primary role for imaging in cervical lymphadenopathy is to diagnose metastatic disease in head and neck squamous cell carcinoma (HNSCC), which significantly impacts treatment. Other nonneoplastic causes of cervical lymphadenopathy, including various infectious and inflammatory diseases, usually do not require routine imaging. This chapter reviews the anatomy and classification of cervical lymph nodes, diagnostic criteria, and imaging findings of lymph node metastasis and the imaging appearance of other benign cervical lymphadenopathies.
2.1 Introduction
While there are a variety of causes of cervical lymphadenopathy (see Box 2.1), the primary role for imaging in cervical lymphadenopathy is to diagnose metastatic disease in head and neck squamous cell carcinoma (HNSCC), which significantly impacts treatment. Other nonneoplastic causes of cervical lymphadenopathy, including various infectious and inflammatory diseases, usually do not require routine imaging. This chapter reviews the anatomy and classification of cervical lymph nodes, diagnostic criteria, and imaging findings of lymph node metastasis and the imaging appearance of other benign cervical lymphadenopathies.
Box 2.1. Causes of Cervical Lymphadenopathy
Neoplastic | Squamous cell carcinoma |
Lymphoma | |
Thyroid carcinoma (papillary most common) | |
Kaposi sarcoma | |
Metastases (lung, breast, melanoma, renal cell, carcinoid) | |
Infection | Bacterial |
Mycobacterium tuberculosis | |
Infectious mononucleosis | |
Cytomegalovirus | |
Rubella | |
Cat-scratch disease | |
Brucellosis | |
Lyme disease | |
Granulomatous disease | Sarcoidosis |
Langerhans cell histiocytosis | |
Miscellaneous | Castleman’s disease (angiofollicular lymphoid hyperplasia) |
Posttransplantation lymphoproliferative disease | |
Sinus histiocytosis with massive lymphadenopathy | |
Kimura disease |
2.2 Anatomy and Pathophysiology
Given that regional nodal metastasis is the single most important prognostic factor for HNSCC, evaluation of cervical nodes is an essential component of staging and treatment planning. Cross-sectional imaging significantly improves accuracy of detection of metastatic nodal disease, particularly when non-palpable.
Knowledge of cervical anatomy and nodal classification is essential to accurately describe cervical nodal metastases in HNSCC. The American Joint Committee on Cancer (AJCC) has classified neck lymph nodes from levels I through VII. Level I refers to nodes in the submandibular and submental regions. Levels II, III, and IV refer to lymph nodes along the anterior cervical chain. Level V and VI nodes are in the posterior and visceral compartments of the neck, respectively, and level VII nodes are in the superior mediastinum (Fig. 2.1).
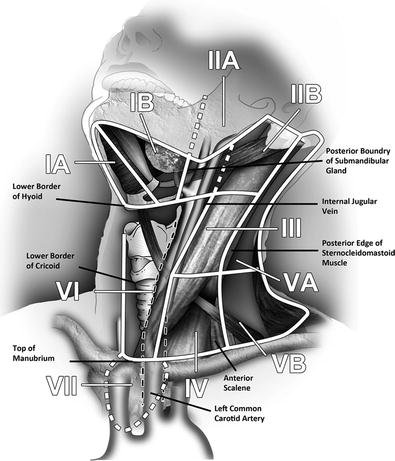
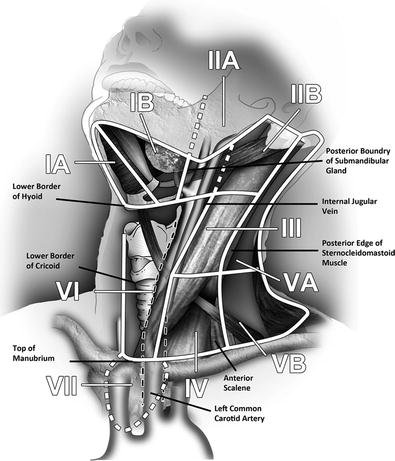
Fig. 2.1
Oblique sagittal graphic showing the relevant anatomic landmarks for imaging-based nodal classification. The important landmarks visible on this graphic include lower border of hyoid (levels I and II), lower border of cricoid (levels III and IV), (levels VA and VB) top of manubrium (levels VI and VII), anterior belly of digastric (levels IA and IB), posterior border of submandibular gland (levels IB and IIA), and posterior border of internal jugular vein (levels IIA and IIB). The anterior scalene (levels IV and VB) and carotid arteries (levels II and IV from VI) are not well visualized on this image
The essential anatomic landmarks used for imaging classification are depicted in Fig. 2.1 and are described in Box 2.2. Certain nodes are still classified according to their anatomic names, including supraclavicular, retropharyngeal, parotid, facial, occipital, and postauricular.
The clinically important internal jugular nodes are classified as level II, III, or IV nodes (previously referred to as upper, mid-, and lower jugular nodes). On axial imaging, levels II and III are separated by the bottom of the body of the hyoid bone, and levels III and IV are separated by the bottom of the arch (anterior rim) of the cricoid cartilage (Figs. 2.2 and 2.3). All three levels are bounded posteriorly by the posterior edge of sternocleidomastoid muscle (SCM). Level II is also bounded posteriorly by the posterior edge of the submandibular gland. Level IIA nodes lie adjacent to the internal jugular vein (IJV); any level II nodes that are posterior to the IJV and are separated from the vein by a fat plane are level IIB nodes. Level I nodes are above the hyoid bone, below the mylohyoid muscle, and anterior to posterior margin of submandibular gland. They are subdivided into levels IA (submental) and IB (submandibular) based on whether they are medial or posterolateral to the anterior belly of digastric muscle, respectively. Level III nodes lie anterior to the posterior margin of the SCM and in between the lower margin of the body of the hyoid bone and the lower margin of the cricoid cartilage arch. Level III nodes also lie lateral to the medial margin of either the common carotid artery or the internal carotid artery. On each side of the neck, the medial margin of these arteries separates level III (lateral) from level VI (medial) nodes. Level IV nodes lie between the level of the lower margin of the cricoid cartilage arch and the level of the clavicle as seen on each axial scan. These nodes are anteromedial to a line drawn through the posterior edge of the SCM and the posterolateral edge of the anterior scalene muscle on each axial image. Also, the medial aspect of the common carotid artery separates level IV (lateral to the artery) from level VI nodes (medial to the artery) (Figs. 2.1 and 2.4).
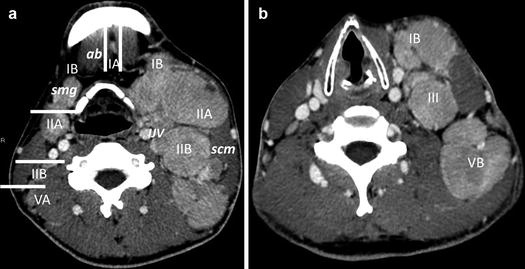
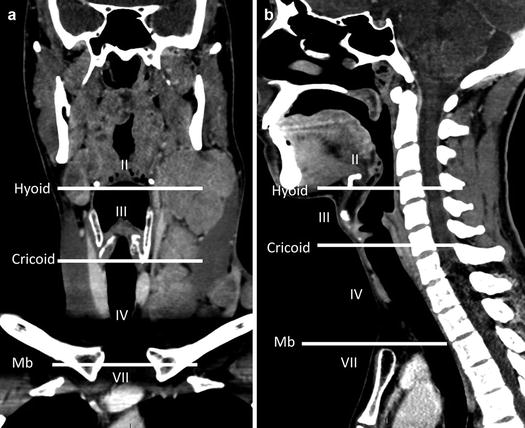
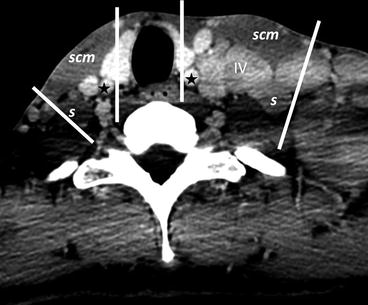
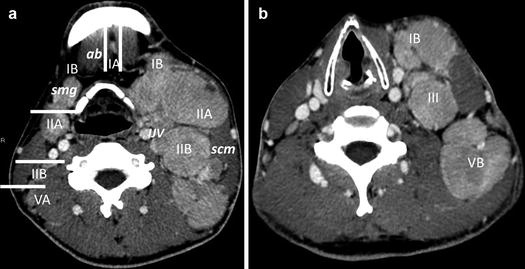
Fig. 2.2
(a and b) A 23 year-old with Hodgkin’s lymphoma above and below the hyoid cartilage. ab anterior belly of digastric, smg submandibular gland, scm sternocleidomastoid, IJV internal jugular vein. White lines divide the different nodal compartments. Level IA is in between the anterior belly of digastric, while level IB is in between the anterior belly of digastric and posterior margin of submandibular gland. Levels II/III/IV are separated from level V by posterior border of sternocleidomastoid. Levels IIA and IIB are divided by internal jugular vein (IJV). Nodes that lie anterior or contact IJV are IIA nodes. Levels II and III and III and IV are defined by the inferior borders of hyoid and cricoid cartilages, respectively
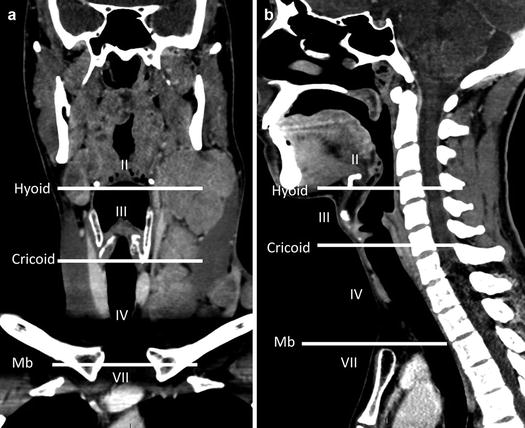
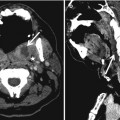
Fig. 2.3
(a and b) Coronal and sagittal CT images show levels II, III, and IV sites divided by inferior border of hyoid and inferior border of cricoid. Levels VI and VII are separated by the superior border of manubrium
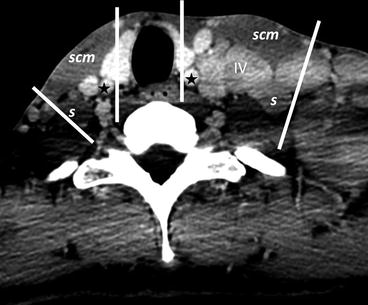
Fig. 2.4
Axial contrast-enhanced CT scans through the infrahyoid lower neck show levels IV, V, and VI sites, defined by medial margin of common carotid artery (star) and oblique line from lateral anterior scalene muscle (s) to posterior border of sternocleidomastoid muscle (scm)
Level V nodes extend from the skull base, at the posterior border of the attachment of the SCM, to the level of the clavicle as seen on each axial scan. Level VA (upper level V) nodes lie between the skull base and the lower margin of the cricoid cartilage arch, behind the posterior edge of the SCM, while level VB (lower level V) nodes lie between the level of the lower margin of the cricoid cartilage arch and the level of the clavicle as seen on each axial scan. Their anterior boundary if formed by the posterior edge of the SCM (Figs. 2.1, 2.2, and 2.3).
Identification of the clavicle allows one to separate the supraclavicular from axillary nodes on axial CT slices. When any portion of the clavicle is seen on the scan, the visible nodes are classified as supraclavicular nodes, while any nodes below the level of the clavicle and lateral to the ribs are classified as axillary nodes.
Level VI nodes or the visceral nodes lie inferior to the lower body of the hyoid bone, superior to the top of the manubrium, and between the medial margins of the left and right common carotid arteries or the internal carotid arteries. Level VII nodes lie inferior to the top of the manubrium in the superior mediastinum, between the medial margins of the common carotid arteries. These superior mediastinal nodes extend caudally to the level of the innominate vein (Figs. 2.3 and 2.4).
Box 2.2. Imaging-Based Nodal Classification
Levels | Boundaries | |||
|---|---|---|---|---|
Superior | Inferior | Anterior (medial) | Posterior (lateral) | |
IA Submental group | Symphysis of mandible | Body of hyoid | Anterior belly of contralateral digastric muscle | Anterior belly of ipsilateral digastric muscle |
IB Submandibular group | Body of mandible | Posterior belly of digastric muscle | Anterior belly of digastric muscle | Stylohyoid muscle |
IIA Upper jugular group nodes | Skull base | Horizontal plane defined by the inferior border of hyoid bone | Stylohyoid muscle | Vertical plane defined by the spinal accessory nerve |
IIB Upper jugular group nodes | Skull base | Horizontal plane defined by the inferior border of hyoid bone | Vertical plane defined by the spinal accessory nerve | Lateral border of the sternocleidomastoid muscle |
III Mid-jugular group | Horizontal plane defined by the inferior border of hyoid bone | Horizontal plane defined by the inferior border of cricoid cartilage | Lateral border of the sternohyoid muscle | Lateral border of the sternocleidomastoid muscle or sensory branches of the cervical plexus |
IV Lower jugular group | Horizontal plane defined by the inferior border of cricoid cartilage | Clavicle | Lateral border of the sternohyoid muscle | Lateral border of the sternocleidomastoid muscle or sensory branches of the cervical plexus |
VA Posterior triangle group | Apex of the convergence of sternocleidomastoid and trapezius muscles | Horizontal plane defined by the inferior border of the cricoid cartilage | Lateral border of the sternocleidomastoid muscle or sensory branches of the cervical plexus | Anterior border of the trapezius muscle |
VB Posterior triangle group | Horizontal plane defined by the inferior border of cricoid cartilage | Clavicle | Lateral border of the sternocleidomastoid muscle or sensory branches of the cervical plexus | Anterior border of the trapezius muscle |
VI Central or anterior group | Hyoid bone | Top of manubrium | Common carotid artery | Common carotid artery |
VII Superior mediastinal group | Top of manubrium | Innominate vein | Common carotid artery | Common carotid artery |
Note: Other superficial nodal groups continue to be referred to by their anatomic names including parotid, facial, and postauricular lymph nodes | ||||