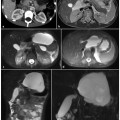
Fig. 3.1
Gallbladder stones. a Ultrasound showing confluent shadowing (arrow) caused by multiple small stones located in the dependent wall of the gallbladder. b An axial T2-weighted image shows small gallbladder stones as round hypointense stones (arrow)in less hypointense biliary sludge located in the dependent portion of gallbladder. c A coronal T2-weighted image from another patient shows multiple hypointense stones (arrow) in hyperintense bile of the gallbladder. d A magnetic resonance cholangiopancreatography (MRCP) image shows the stones as filling defects (arrow) and provides a cholangiographic display of the biliary system as a result of displaying only non-flowing fluid in the biliary and pancreatic ducts
The following techniques assist in the demonstration of an acoustic shadow posterior to a stone: (1) reducing the overall or far gain, (2) increasing the frequency of the transducer, and (3) changing the angle and distance between the transducer and stone so that the stone lies perpendicular to and within the center of the focal zone of the transducer. Gallstones typically produce „clean” shadowing without reverberation because most of the sound is absorbed by the stone. This is in contradistinction to bowel gas, in which 99% of the incident sound energy is reflected and produces reverberations and backscatter echoes (dirty shadowing). Reverberation artifacts may be seen posterior to calcified stones, which contain gas within fissures [8].
Gallbladder stones have a various appearance at computerized tomography (CT), from very calcified to very-low-density stones typical of pure cholesterol bile stones. Because of its low sensitivity, CT is not suggested in the diagnostic flow chart for biliary system ducts.
Magnetic resonance cholangiopancreatography (MRCP) has a high sensitivity in the detection of gallbladder stones (Fig. 3.1b–d), but its use becomes necessary only in the suspected presence of common bile duct stones [14, 15a].
3.4.2 Common Bile Duct Stones
Suspicion of the presence of common bile duct stones usually arises at abdominal US, which is the first-line imaging investigation when biliary tree calculi are suspected. At US, the presence of echogenic materials with a distal acoustic shadow within the common bile duct can be seen (Fig. 3.2a). However, they are more easily seen when surrounded by anechoic bile and when large enough to cast an acoustic shadow. Stones impacted in the distal duct may be difficult to recognize when their margins are inseparable from the adjacent duct walls and surrounding echogenic fat [10].
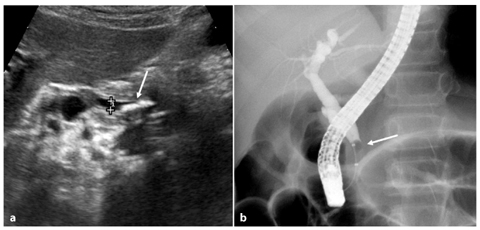
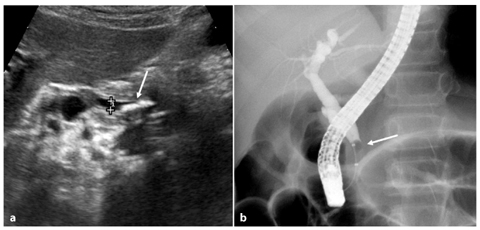
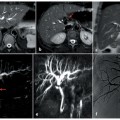
Fig. 3.2
Distal common bile duct stones. a Ultrasound in a patient with biliary colic shows a dilated common bile duct with hyperechogenic materials with a distal acoustic shadow (arrow) within the distal part. The hyperechogenic stones are large enough to cast an acoustic shadow that allows them to be detected. b Endoscopic retrograde cholangiopancreatography of the same patient. It is the treatment of choice in this case because there is a high probability of the presence of common bile duct stones; an obstruction (arrow) is seen in the distal portion of the common bile duct and is caused by common bile duct stones. A sphincterotomy and endoscopic stone extraction was performed in this patient
Detecting stones in the ducts is easier when biliary dilatation is also present. Unfortunately, because biliary dilatation is present in only about two-thirds to three-quarters of patients, it can be difficult to image stones in many patients.
The detection rate for common bile duct stones at US is also influenced by patient factors such as the number, size and site of the stones, patient body habitus, and the presence of overlying bowel gas; detection is more difficult in patients who have undergone cholecystectomy.
Endoscopic retrograde cholangiopancreatography (ERCP) has long been considered the standard of reference for examination of common bile duct stones. However, a diagnostic strategy based on routine instrumentation of the biliary system, particularly in patients who have a low pre-test probability of disease, is undesirable.
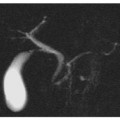
In many recent studies, MRCP has been shown to have a diagnostic accuracy comparable to that of ERCP, with the ability to demonstrate small biliary stones and the advantage of not using ionizing radiation [13, 16]. In current practice, where initial assessment suggests a high probability of common bile duct stones, it is reasonable to proceed directly to ERCP (Fig. 3.2b) if this is considered to be the treatment of choice; however, in cases of inconclusive US where initial assessment suggests a low or uncertain index of suspicion for common bile duct stones prior to interventional procedures such as ERCP, it is recommended that patients undergo magnetic resonance imaging (MRI) (Fig 3.3).
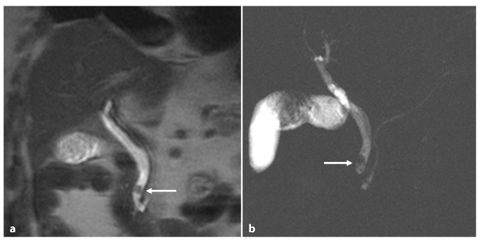
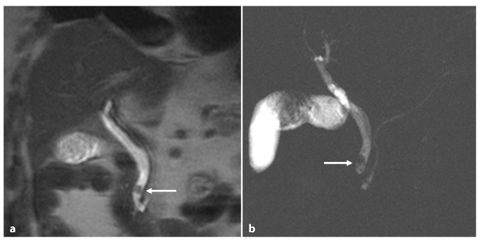
Fig. 3.3
Patient with biliary colic and cholelithiasis, but no sign of choledocholithiasis at ultrasound. A coronal T2- weighted image (a) and a coronal magnetic resonance cholangiopancreatography image (b) show a small filling defect (arrow) in the juxta-papillary tract of the common bile duct
3.4.3 Intrahepatic Duct Stones
In the detection of intrahepatic duct stones, US shows the same signs, and has the same advantages and limitations, as in the detection of common bile duct stones.
Intrahepatic stones can be seen on nonenhanced CT, but the detection rate is not satisfactory (60–80%) because pigmented stones are sometimes not sufficiently hyperattenuating to be visible on CT.
ERCP has long been considered the standard of reference for examination of intrahepatic stones, such as common bile duct stones, but MRCP has proven to be superior to ERCP for the diagnosis of intrahepatic bile duct stones because ERCP cannot opacify the biliary duct system upstream to a stenosis. Lack of an endoluminal contrast agent impairs the possible identification of endoluminal filling defects. The ability of MRCP to visualize peripheral intrahepatic bile ducts makes this technique well suited to the evaluation of stones in this site (Fig. 3.4) [16, 17].
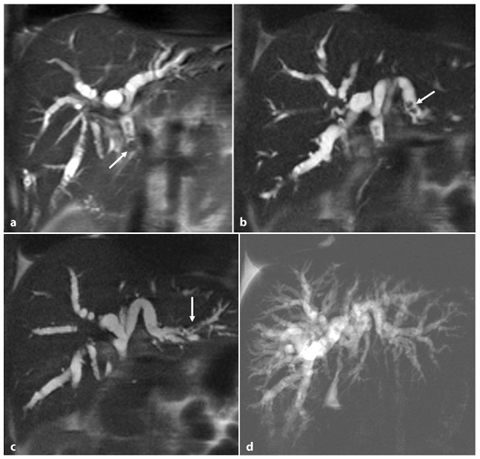
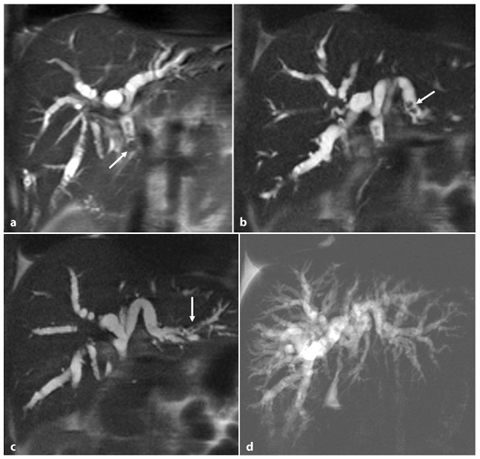
Fig. 3.4
Intrahepatic bile duct stones. a A coronal T2-weighted image shows a stone (arrow) in the common hepatic duct, with dilatation of the intrahepatic biliary system. b, c Coronal oblique T2-weighted images show multiple intrahepatic duct stones (arrow) in the same patient. d A maximum intensity projection reconstruction of magnetic resonance cholangiopancreatography allows visualization of all the intrahepatic ductal segments in one image
When looking for the presence of intrahepatic biliary stones, half-Fourier T2-weighted images with paracoronal or oblique acquisition can be very useful. In such cases, we obtain MRCP images with parallel scans of the primary intrahepatic bile ducts. In these sequences we can visualize stones of the intrahepatic ducts that are present in different planes of the spaces.
Consecutive maximum intensity projection (MIP) reconstruction of a thin-slab acquisition can help us to completely visualize the intrahepatic biliary system, and it mimics the images of direct cholangiography.
3.5 MRCP Imaging in Choledocholithiasis
3.5.1 MRCP Signs
Study of the biliary tract is performed using axial and coronal half-Fourier T2-weighted images with long TR (Fig. 3.5a–c), followed by MRCP performed using oblique half-Fourier T2-weighted images with a maximum TE (> 800 ms) and a short time of echo (TE), which provide a cholangiographic display (Fig. 3.5d).
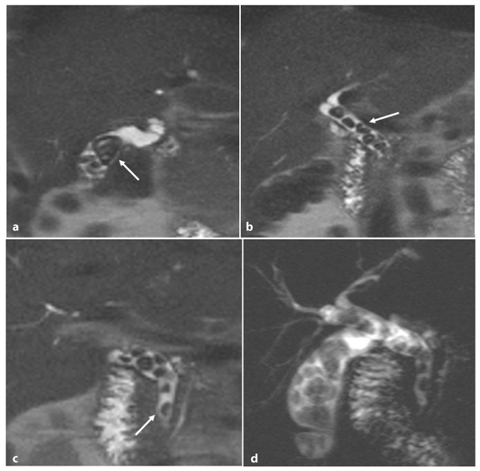
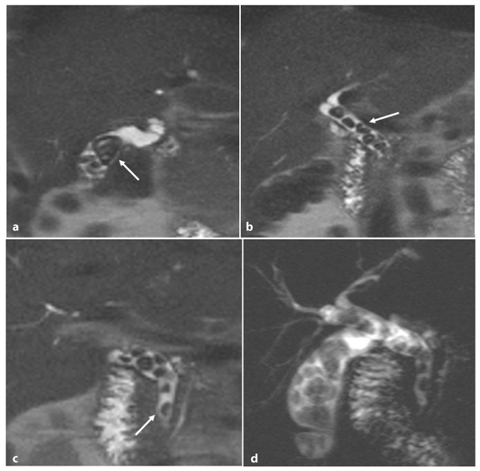
Fig. 3.5
Multiple biliary stones in the gallbladder and common bile duct. a–c Coronal thin-slab T2-weighted images show endoluminal filling defects (arrow) within the lumens of the gallbladder and in the common hepatic duct, surrounded by hyperintense bile. There is enlargement of the bile duct and cystic duct. d A coronal magnetic resonance cholangiopancreatography shows all the filling defects with good spatial resolution and provides a cholangiographic display of the biliary system
Currently, we use half-Fourier T2-weighted images and RARE (rapid acquisition with relaxation enhancement) T2-weighted images, which are less sensitive to inhomogeneity of magnetic field and movement artifacts
RARE sequences make use of a heavily weighted T2 pulse sequence using the RARE and half-Fourier RARE pulse sequences, and they have proved to be reliable in the detection of choledocholithiasis [18, 19]. Currently, they are the sequences of choice for MRCP because they have a long TE, which allows display of non-flowing fluid in the biliary and pancreatic ducts and solid organs, and flowing blood, which gives little or no signal. They essentially eliminate the problem of motion artifact and have a greater contrast-to-noise ratio and increased spatial resolution.
MRCP can be performed with both a thickcollimation (single-section) and a thin-collimation (multisection) technique with a torso phased-array coil. The coronal plane is used to provide a cholangiographic display and the axial plane is used to evaluate the pancreatic duct and the distal common bile duct [20, 21a].
Biliary stones, independently from calcium content, almost always present with low signal intensity on magnetic resonance images. Therefore the stone is identified as a round or oval-shaped „filling defect” within the biliary system, surrounded by the highsignal-intensity bile [22–24].
In axial T2-weighted images, the „target sign”, representing a central hypointense filling defect surrounded by hyperintense bile, is seen when the stone is not in the dependent portion of the duct (Fig. 3.6a–c) or when the convex margin of an impacted large stone is seen (Fig. 3.6d–f).
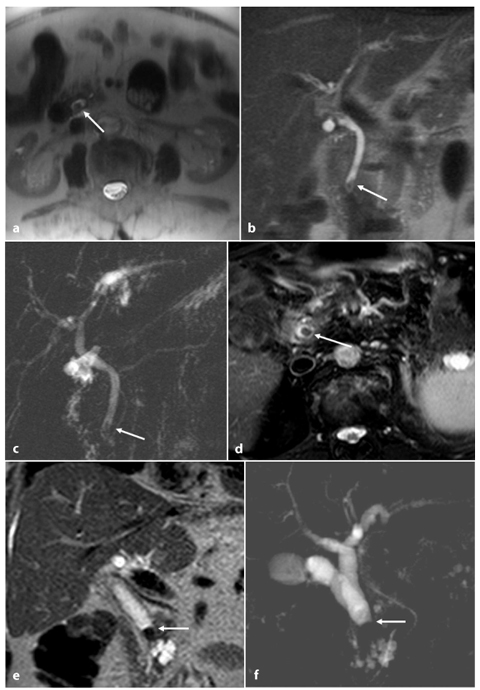
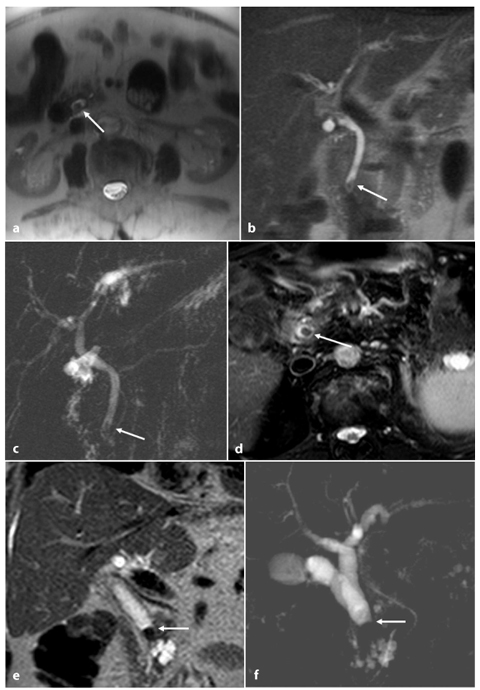
Fig. 3.6
Magnetic resonance cholangiopancreatography (MRCP) signs of common bile duct stones: „target sign” on axial image and „convex margin” on coronal image. a Small stone not located in dependent portion of lumen. An axial T2-weighted image shows a central filling defect with a thin coat of hyperintense bile around it („target sign”) (arrow). Coronal T2-weighted thick-slab (b) and MRCP (c) images show a small filling defect in the pre-papillary portion of the common bile duct, with a superior „convex margin” and surrounded by bile (arrow). d Large impacted stone in the common bile duct. An axial T2-weighted image at the highest level of the obstruction shows a central filling defect with a thin coat of hyperintense bile around it („target sign”) (arrow). Coronal T2-weighted image thick-slab (e) and MRCP (f) images demonstrate a dilated common bile duct with occlusion in the intermediate portion, without visualization of the duct distally. At the site of obstruction, the hyperintense bile produces a „convex margin” (arrow)
In cases where there is a large impacted stone that is not outlined at all by the hyperintense bile, searching carefully for this sign in axial images can help us to exclude a malignant disease that causes an abrupt stop of the common bile duct.
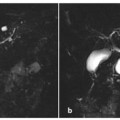
The „crescent-shaped duct” is a sign that results from visualization of an axial image through a non-impacted stone that is located in the dependent portion of the duct (Fig. 3.7), and it consists of a visible hyperintense flattened duct that forms a crescent at the level of the calculus in axial images. This sign is also useful in situations in which a diagnosis is inconclusive. Impacted stones are more difficult to identify on MRCP images, because in cases where there is absence of bile it is impossible to distinguish the stone from the biliary duct wall, since they have the same signal intensity. Therefore the presence of an impacted stone may simulate biliary stenosis. In this situation, we repeat the axial images with a thinner collimation to be able to see through the convex margins of the stone and detect a thin crescent or surrounding rim of bile between the non-dependent duct wall and stones [25, 26].
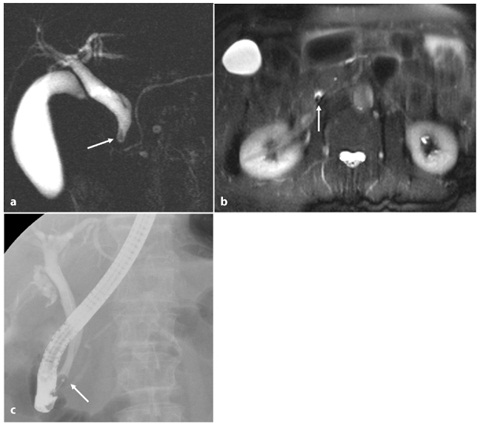
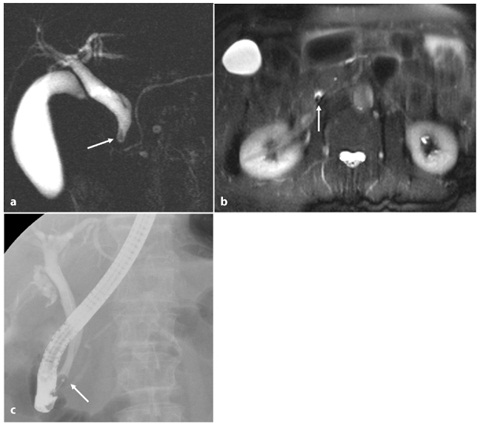
Fig. 3.7
Magnetic resonance cholangiopancreatography (MRCP) shows small common bile duct stones: the „crescent-shaped duct” sign. a An MRCP thick-slab T2-weighted image shows a filling defect in distal portion of the common bile duct (arrow). b An axial T2-weighted image shows the small calculus as a filling defect in the dependent position (arrow) with the „crescent- shaped duct” sign produced by the bile anterior to the calculus. c Endoscopic retrograde cholangiopancreatography confirms the presence of the stone in the distal common bile duct (arrow), with consecutive sphincterotomy and stone extraction
Coronal T2-weighted images are useful to evaluate the shape, location and number of filling defects in the coronal plane, and the effects that they produce on the proximal portion of the biliary duct. On coronal T2-weighted images, it is necessary to pay attention to the presence of the superior convex margin of the filling defect (Figs. 3.6 and 3.7), as this allows us to make a differential diagnosis with other causes of filling defects, such as malignant diseases that cause an abrupt stop of the common bile duct without a visible superior convex margin [26, 27].
It is possible to perform coronal T2- weighted imaging with a thin slice to search for small calculi, and then to repeat the same sequence with a thicker slice or to perform a MIP reconstruction to depict a greater length of the duct in a single image (Fig. 3.8).
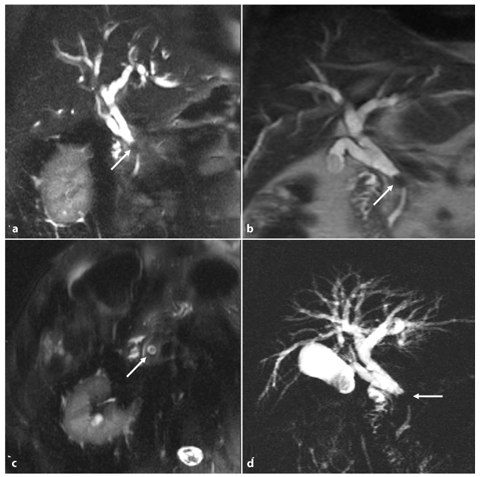
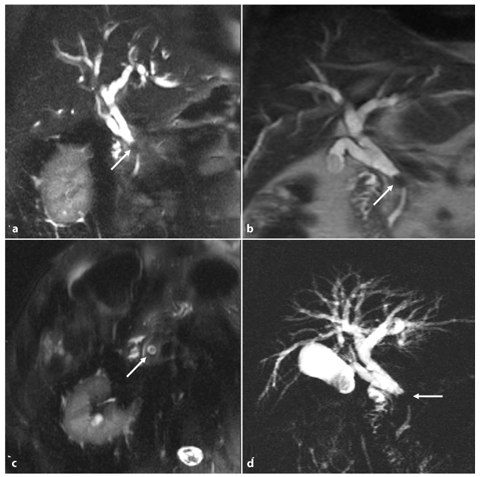
Fig. 3.8
Intermediate common bile duct stones and gallstones in the infundibulum: use of thinner and thicker collimation coronal T2-weighted images. a A coronal T2-weighted image shows a filling defect in the intermediate tract of the common bile duct (arrow). b A coronal half-Fourier acquisition single-shot turbo-spin-echo (HASTE) T2-weighted image with thicker collimation allows depiction of a greater length of the duct, and also depiction of a gallbladder stone (arrow) on a single image rather than on the thin-collimation image. c An axial T2-weighted image at the level of the common bile duct stone shows the „target sign” (arrow). d A coronal thick-slab T2-weighted image shows filling defects in the gallbladder and common bile duct (arrow), with dilatation of the common bile duct, cystic duct and intrahepatic biliary system
Some radiologists prefer to perform MRCP examinations using three-dimensional (3D) reconstructions by using a MIP algorithm on the thin-collimation source images (Fig. 3.9). Therefore, they use the T2-weighted half-Fourier 3D with a thin slab (3 mm), since the volume acquired encompasses the whole bile duct; in this manner MIP reconstruction can be obtained without loss of anatomical detail, which is different from any one thin-collimation source image [28, 29]. Although MIP images more closely resemble conventional cholangiograms, and are familiar to many clinicians, spatial resolution is degraded because of volume-averaging effects. Diagnostic decisions are usually made on the basis of the thin-collimation source images.
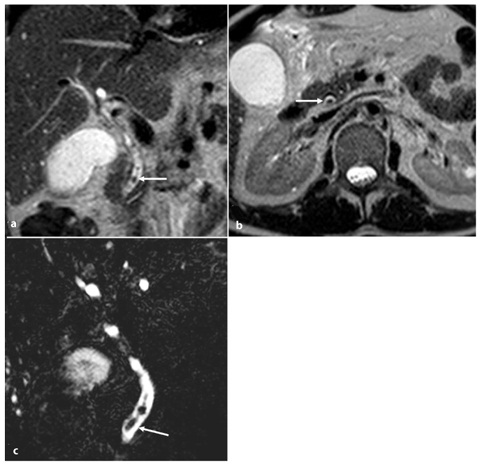
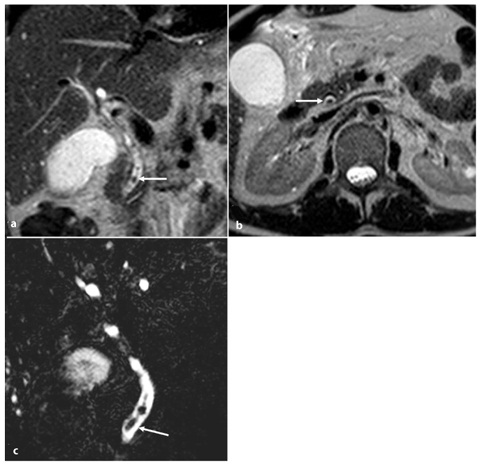
Fig. 3.9
Three-dimensional (3D) magnetic resonance cholangiopancreatography (MRCP) of common bile duct stones. a A coronal T2-weighted image shows a small endoluminal filling defect within the lumen of the distal portion of the common bile duct, surrounded by hyperintense bile (arrow). b An axial T2-weighted image demonstrates a round filling defect in the intrapancreatic portion of the common bile duct, surrounded by bile (arrow). c A coronal half-Fourier 3D T2-weighted image with thin collimation shows an even smaller filling defect (arrow)
MIP images are useful in the 3D depiction of ductal anatomy and in planning surgical procedures, but the source images, which provide greater spatial resolution, must be carefully scrutinized so as not to overlook small luminal filling defects and strictures that may be obscured on the thicker collimation images [29, 30].
3.5.2 Advantages of MRCP
At the time of the first clinical application of MRCP over a decade ago, it was regarded, at best, as a novel technique with questionable potential for imaging the biliary tract and pancreatic duct. However, since then MRCP has undergone a number of technical refinements and has been shown to have a wide range of clinical applications. These factors have contributed to the evolution of MRCP as an accepted and accurate technique for non-invasive imaging of the pancreaticobiliary tract [17, 31].
MRCP offers a number of advantages compared with ERCP, which is the standard of reference for imaging the biliary tract and pancreatic duct. MRCP is a non-invasive examination, and it avoids entirely the complications of ERCP that occur in up to 5% of all ERCP procedures; these complications include pancreatitis, hemorrhage, and gastrointestinal tract perforation and hemorrhage. Unlike ERCP, MRCP is performed rapidly and does not expose patients to ionizing radiation or iodinated contrast material. The major disadvantage of MRCP is that it is entirely diagnostic, and this is in contrast to ERCP, which provides diagnostic information as well as access for therapeutic interventions [12, 32].
The clinical applications of MRCP are numerous, and they include the diagnosis of common bile duct stones, malignancies of the pancreaticobiliary tract, congenital anomalies such as choledochal cysts, aberrant bile ducts and pancreas divisum, primary sclerosing cholangitis, acute and chronic pancreatitis, and gallbladder disease such as stones and carcinoma. MRCP is also useful in the evaluation of patients who have experienced an incomplete or failed ERCP attempt and in the evaluation of patients in whom the performance of ERCP is difficult or impossible because of surgical alterations of the gastrointestinal tract [33, 34].
As a result of this expanding range of clinical applications, MRCP has replaced diagnostic ERCP in some institutions as a means of identifying diseases of the bile and pancreatic ducts. Once disease has been detected with MRCP, patients may then be triaged appropriately for therapy with ERCP, surgery or radiological intervention [34–39].
Currently, the primary role of ERCP is to provide access to the pancreaticobiliary tract for stone extraction, stent placement, balloon dilatation and other interventions. Diagnostic ERCP continues to be useful in identifying bile duct and cystic duct leaks, clarifying complex ductal anatomy, and providing information in the setting of an equivocal or nondiagnostic MRCP.
3.6 Differential Diagnosis
A differential diagnosis has to be made with an endoluminal cause of obstruction, parietal causes, extrinsic conditions that cause narrowing of the common bile duct, and proximal dilatation mimicking the presence of an obstruction.
3.6.1 Endoluminal Causes of Obstruction
3.6.1.1 Pneumobilia
Pneumobilia may be misinterpreted as bile duct stones, although it is easily recognized at axial MRCP or T2-weighted MRI because it produces a filling defect in an antidependent position of the duct (Fig. 3.10).
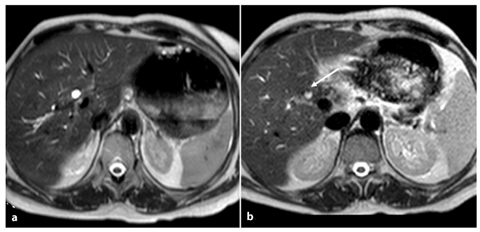
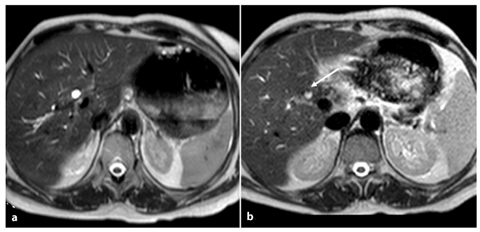
Fig. 3.10
Pneumobilia. Axial T2-weighted image. a Common hepatic duct with a caliber of 8 mm. b In the common bile duct there is a filling defect ventrally to the bile (air bubble) (arrow)
Small amounts of air cannot be clearly seen at MRI, and often differentiation can be impossible unless anamnestic information of endoscopic treatments or CT correlation is obtained.
3.6.1.2 Signal Void
Signal void is seen occasionally in the nondependent central portion of the bile duct and may be misinterpreted as stones (Fig. 3.11). The signal void tends to appear in dilated ducts and at the point of insertion of a large cystic duct, where swirling flow can occur, and it is considered to be a flow artifact [40




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree